Hemolytic uremic syndrome (HUS) is a disorder characterized by the presence of the classic triad: microangiopathic hemolytic anemia, thrombocytopenia and acute renal injury. HUS without acute renal failure can be confused with other hematologic diseases. An infantile HUS caused by a Shiga-toxin-producing Escherichia coli (STEC) O145 strain carrying genotype stx2, ehxA, eae subtype β1 is herein reported. The infant did not require dialysis during the acute stage of HUS, evolved favorably, maintained normal blood pressure and normal renal function and had no recurrence until the last control. This could be due to several factors, such as the characteristics of infecting STEC strain and a reduction in host susceptibility to renal injury. This report highlights the regional participation of non-O157 STEC in childhood diseases and the importance of performing active surveillance for all forms of HUS.
El síndrome urémico hemolítico (SUH) es una afección caracterizada por la presencia de la tríada clásica: anemia hemolítica microangiopática, trombocitopenia y compromiso renal agudo. Los casos de SUH sin insuficiencia renal pueden confundirse con otras enfermedades hematológicas. Presentamos un caso de SUH pediátrico causado por una cepa de Escherichia coli productora de toxina Shiga [Shiga-toxin-producing Escherichia coli (STEC)] O145 con el genotipo stx2, ehxA, eae subtipo β1. El niño no requirió diálisis durante la etapa aguda del SUH, evolucionó favorablemente y no tuvo recurrencias hasta el último control; además, mantuvo cifras normales de presión arterial y función renal normal. Esto puede deberse a varios factores: características de la cepa STEC infectante y susceptibilidad del hospedero al daño renal, entre otros. Este hallazgo destaca la participación regional de STEC no-O157 en enfermedades de la infancia y la importancia de realizar una vigilancia activa de todas las formas de SUH.
Hemolytic uremic syndrome (HUS) is a disorder characterized by the presence of the classic triad: microangiopathic hemolytic anemia, thrombocytopenia, and acute renal injury8,10. There are 2 forms of HUS: typical (with diarrhea in the prodromal period) and atypical (without diarrhea in that period). In addition, HUS may be “complete” (complete triad: microangiopathic hemolytic anemia, thrombocytopenia, and acute renal involvement) or “incomplete” (when the patient does not have any of the manifestations of the classical triad). The typical one, also known as post-enteric HUS or STEC-HUS is the most common, being responsible for 90–95% of cases and occuring after intestinal infection by strains of Shiga-toxin-producing Escherichia coli (STEC). It occurs mainly in children under 5 years of age and is usually preceded by episodes of bloody diarrhea or hemorrhagic colitis. STEC-HUS is the leading cause of acute renal failure and the second leading cause of chronic renal failure and renal transplantation in children under 5 years of age10.
Sometimes, HUS cases present thrombocytopenia and anemia without acute renal failure, making diagnosis difficult4.
We here describe a case of a child with HUS, with the aim of alerting healthcare professionals, especially pediatricians, hematologists, nephrologists and microbiologists in this regard,
On January 16, 2013 a 1 year-old infant from “Las Piedras” (in the urban area of Canelones Department, Uruguay) was brought to the emergency room with vomiting and fever. During the preceding 48 hours, he had fever without diarrhea and had vomited on several occasions. On examination, he was febrile (38.5°C axillary), depressed, with intense mucocutaneous pallor and upper right foot petechiae. He was well hydrated and perfused with a heart rate of 150cpm, no murmurs and PA records of 110/86Hg mm. Edema was not present, and the remaining examination was normal. Hematological investigations revealed: RBC: 2,200,000/μl; WBC: 24,500/μl; neutrophils: 36%; lymphocytes: 44%; hemoglobin: 6.6g/dl; MCV: 75 fL; hematocrit: 18.7%; platelet count: 54,000/μl. Biochemical analysis displayed the following values: azotemia: 0.51g/l; creatinine: 0.47mg/dl (estimates of glomerular filtration: 99ml/min per 1.73m2); serum sodium, 143mEq/l and serum potassium, 4.1mEq/l. The urine analysis contained 20 erythrocytes per field with hyaline cylinders and showed proteinuria, intense hemoglobinuria and ketonuria.
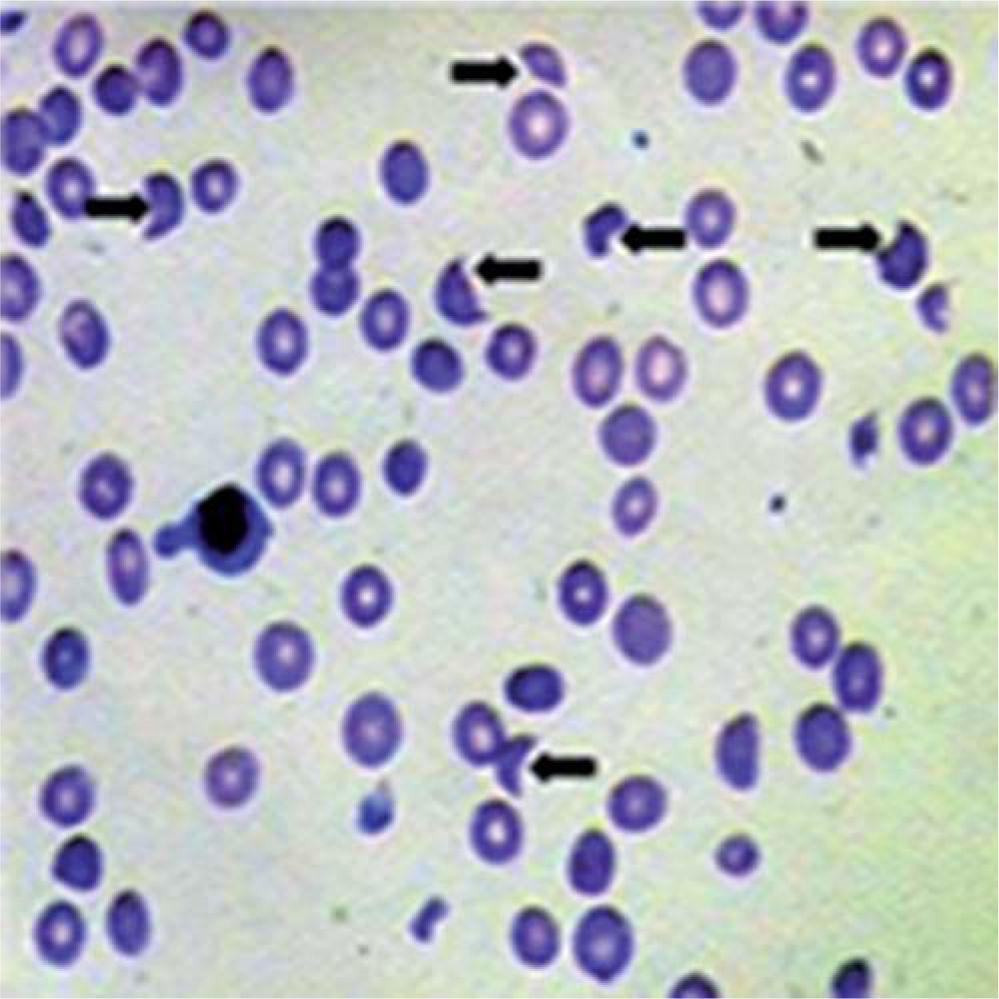
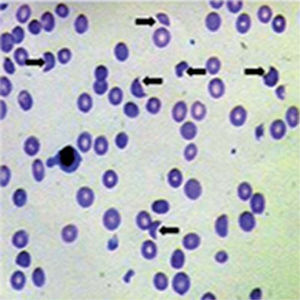
The infant was admitted to a pediatric ward with a diagnosis of hemolytic anemia. He remained hemodynamically stable with tachycardia and preserved diuresis. He was examined by a hemato-oncologist, who performed a new peripheral blood count and a peripheral blood smear, showing: Hb 5.2g/dl, RBC 2,000,000/μl, WBC 22,400/μl, reticulocytes 5%, platelets 71,000/μl and 5-10 fragmented erythrocytes (schizocytes) every 40 erythrocytes, respectively (Fig. 1) With these results, HUS without renal failure was diagnosed.
The stool sample collected on January 17th was sent to the Bacteriology and Virology Department for STEC screening according to the previously described procedure11. PCR was performed on 20 suspected E. coli colonies to detect stx1 and stx2 genes.
Confirmation of isolates as E. coli was performed through biochemical tests and serotyping was conducted using commercial antisera (Statens Serum Institute, Denmark) for serogrouping and our own antibodies for H antigens.
The presence of sequences related to the ehxA and eae genes was determined by PCR7. Subtyping of the eae gene was also performed by PCR1. Antimicrobial susceptibility to amikacin, ampicillin, ceftriaxone, cefuroxime, ciprofloxacin, cloramphenicol, colistin, gentamicin, nalidixic acid, nitrofurantoin, streptomycin, tetracycline, and trimethoprim-sulfamethoxazole was established according to the Clinical Laboratory Standards Institute (CLSI) guidelines3.
The 20 colonies of E. coli analyzed corresponded to STEC serotype O145:HNT, with genotype: stx2, ehxA, eae subtype β1, which were susceptible to all tested antibiotics.
On January 19th, 2013 the patient was admitted to an intermediate care unit for monitoring. He remained hemodynamically stable with preserved diuresis and hypertension for which he received inhibitors of the angiotensin-converting enzyme (IACE), 1.5mg/kg/day.
Azotemia and creatinine remained normal. On January 20th, 2013 he received a 180ml transfusion of concentrated red blood cells and antibiotic treatment with i/v ceftriaxone was started (100mg/ kg/day), due to suspected widespread bacterial infection from the gastrointestinal tract. As the infant showed progressive improvement with normal reticulocyte count and blood pressure, IACE administration was discontinued. Ten days of i/v ceftriaxone treatment were completed. After being examined by the pediatrician and the nephrologist, the child was discharged (01/29/13) with instructions of monthly clinical nephrologic controls.
Until the date of the last control (06/23/13) the infant had no recurrence, maintained normal blood pressure and normal renal function.
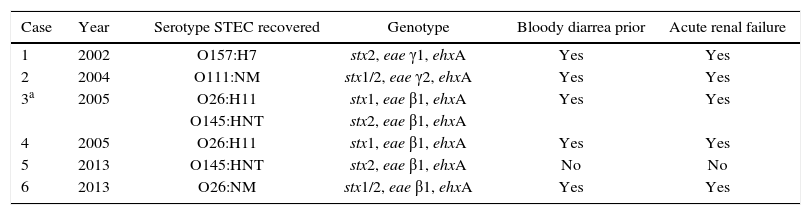
This is the first local report of a pediatric case of STEC-HUS caused by O145 STEC strain with hemolytic anemia and thrombocytopenia but without obvious acute renal failure (Table 1). By definition, all patients with HUS manifest some degree of renal involvement. This form of presentation without acute renal failure can be easily mistaken with other hematologic diseases4. In this case the guiding light was the finding of schizocytes in the peripheral blood smear. HUS is a relatively common disease in our country, having an estimated annual incidence of 4–5 cases per 100,000 children under 5 years of age11. This figure is lower than that reported by Argentina, where approximately 400 new cases are notified per year, with an incidence of 12.2/100,000 in children under 5 years of age9. Between 2002 and 2008 we studied 36 children with a clinical diagnosis of “complete” post-enteric HUS; in three cases we recovered STEC strains belonging to serotypes O157:H7, O111:NM, and STEC O26:H11; in a fourth case an O26:H11/O145:HNT STEC co-infection was detected6,11.
Characteristics of STEC strains recovered from children with HUS in Uruguay.
| Case | Year | Serotype STEC recovered | Genotype | Bloody diarrea prior | Acute renal failure |
|---|---|---|---|---|---|
| 1 | 2002 | O157:H7 | stx2, eae γ1, ehxA | Yes | Yes |
| 2 | 2004 | O111:NM | stx1/2, eae γ2, ehxA | Yes | Yes |
| 3a | 2005 | O26:H11 | stx1, eae β1, ehxA | Yes | Yes |
| O145:HNT | stx2, eae β1, ehxA | ||||
| 4 | 2005 | O26:H11 | stx1, eae β1, ehxA | Yes | Yes |
| 5 | 2013 | O145:HNT | stx2, eae β1, ehxA | No | No |
| 6 | 2013 | O26:NM | stx1/2, eae β1, ehxA | Yes | Yes |
Case number 3 was coinfected with both STEC serotypes (O26:H11 and O145:HNT).
In 2013, we analyzed 3 cases: the case reported here; another one of a 12 month-old infant with complete HUS from whom O26:NM STEC was recovered; and a third case of a two year-old infant who died in the acute phase of the illness and from whom it was not possible to recover STEC. Table 1 shows the characteristics of our recovered STEC strains.
In Uruguay, HUS cases usually occur in the warmer months (spring, summer and early fall) in eutrophic children, from homes with an acceptable socioeconomic level, often living in small villages but not in rural areas6,11. The cases are usually preceded by episodes of bloody diarrhea without an obvious inflammatory component, all showing values of azotemia, serum creatinine and glomerular filtration compatible with some degree of renal injury; most of them require dialysis in the acute phase.
The infant in the present case lived in a home belonging to an acceptable socioeconomic level, did not have previous diarrhea and did not require dialysis. The outcome was favorable despite antimicrobial therapy that can produce undesired effects. This could be due to several factors: the characteristics of the infecting STEC strain (e.g. type and amount of toxin produced; absence of other unknown virulence factors; etc.), the infecting dose or different host susceptibility to renal injury.
We could not establish the food involved and neither were there HUS cases or diarrhea in other members of the family. HUS is not listed as a notifiable event in Public Health regulations, and since the health team and the official health authorities do not usually perform the systematic epidemiological investigation of cases, most of them are not reported.
O145 STEC strains are part of Karmali's seropathotype B and have a pathogenic potential similar to that of O157 isolates.
The finding we here report reinforces our suggestion in previous communications about the comparative regional importance of non-O157 STEC and O157:H7 strains in severe cases of disease in children under 5 years of age, and also stresses the importance of performing active surveillance for all forms of HUS (with or without diarrhea at the prodromal stage), including those cases that can occur after extra-intestinal infection by STEC2,5,6,11.
Ethical responsabilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingCSIC.
AuthorshipL.P., L.A., C.P. and A.D. contributed equally to this work.
Conflicts of interestThe authors declare that they have no conflicts of interest.
This work was supported by CSIC-Grupos (University Research Committee, Uruguay), Universidad de la República (UdelaR).