Human protothecosis is a rare infection caused by algae of the genus Prototheca. Prototheca wickerhamii has been recognized as the main species that causes infection in immunocompromised hosts with deficits in innate or cellular immunity. We report a case of persisting subcutaneous protothecosis in a patient with T-cell large granular lymphocyte leukemia, who also presented a history of disseminated histoplasmosis.
La prototecosis humana es una infección rara causada por algas del género Prototheca. Prototheca wickerhamii ha sido reconocida como la principal especie causante de infección en huéspedes inmunocomprometidos, con déficit de inmunidad innata o celular. Presentamos un caso de prototecosis subcutánea persistente en un paciente con leucemia linfocítica granular de células T, con antecedentes de histoplasmosis diseminada.
Human protothecosis is a rare infection caused by achlorophyllic algae of the genus Prototheca, being Prototheca wickerhamii the species most commonly isolated8,10,11. These organisms are ubiquitous and mainly found in soil, fresh and salty water, slime flux of trees, sewage, animal waste, as well as in some types of food. Protothecosis have been classified into three clinical forms (i) cutaneous/subcutaneous lesions, (ii) olecranon bursitis, and (iii) disseminated or systemic manifestations1,6,8,11. It is believed that Prototheca species may infect humans through contact with potential sources or by traumatic inoculation of the algae in exposed areas4–6,8,10.
Olecranon bursitis and localized cutaneous infections are more commonly developed in immunocompetent patients, whereas dissemination and visceral compromise mainly affect severely immunocompromised patients with cellular deficiency8,10. The most common clinical presentation is a vesiculobullous and ulcerative lesion with pustules and scabs, simulating bacterial, fungal or herpetic infections or eczema4.
We report a case of protothecosis caused by P. wickerhamii. For six years the patient developed diverse cold subcutaneous abscesses without an accurate diagnosis. In this period, she also presented a history of disseminated histoplasmosis and a diagnosis of chronic leukemia.
Case reportA Caucasian 56-year-old woman, born and living in Charata city, located in the southwest of Chaco province (Argentina) attended our Mycology Department in November 2014 (day 0) with an abscess on her left ankle (Fig. 1). In April 2009, the patient noticed the first abscess in her right hand palm, which disappeared without treatment. In January 2010, the patient is admitted to emergency for pneumonia and histoplasmosis diagnosis was confirmed. The patient was treated during 18 months. In February 2013, a second abscess developed in her left elbow. It was diagnosed as olecranon bursitis and an excision biopsy was performed. Histopathology revealed an inflammatory granuloma with abscessed center. Hematologic and biochemical laboratory findings revealed lymphocytosis and polyclonal hypergammaglobulinemia. Immunophenotyping using flow cytometry in peripheral blood and immunohistochemical techniques in the bone marrow biopsy suggested T-cell large granular lymphocyte (T-LGL) leukemia. In November 2013, a third abscess developed in her left hand palm. The abscess was surgically removed and histopathologically studied. Histopathological results reported organisms compatible with Paracoccidioides brasiliensis, not confirmed by microbiological or serological studies.
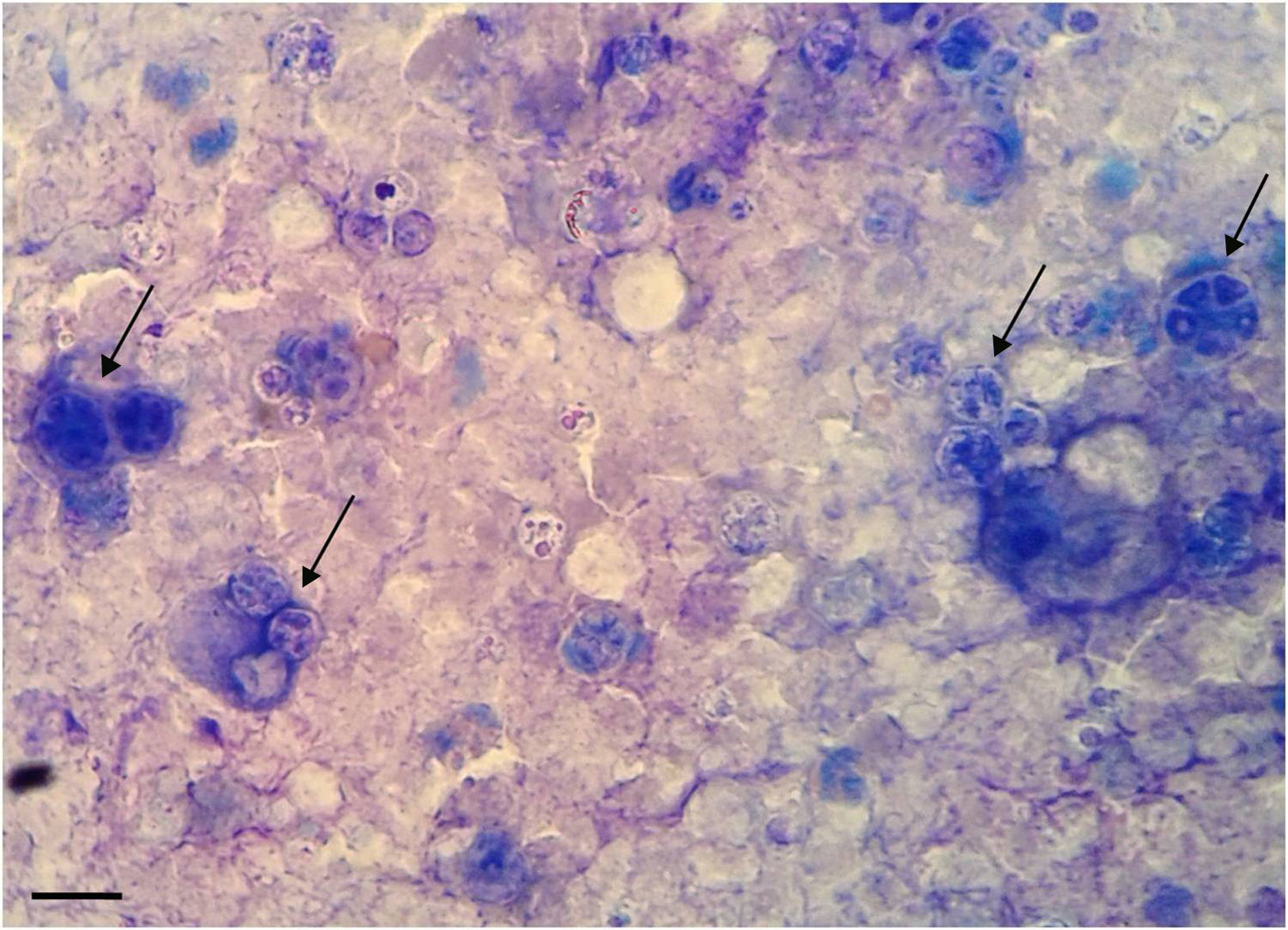
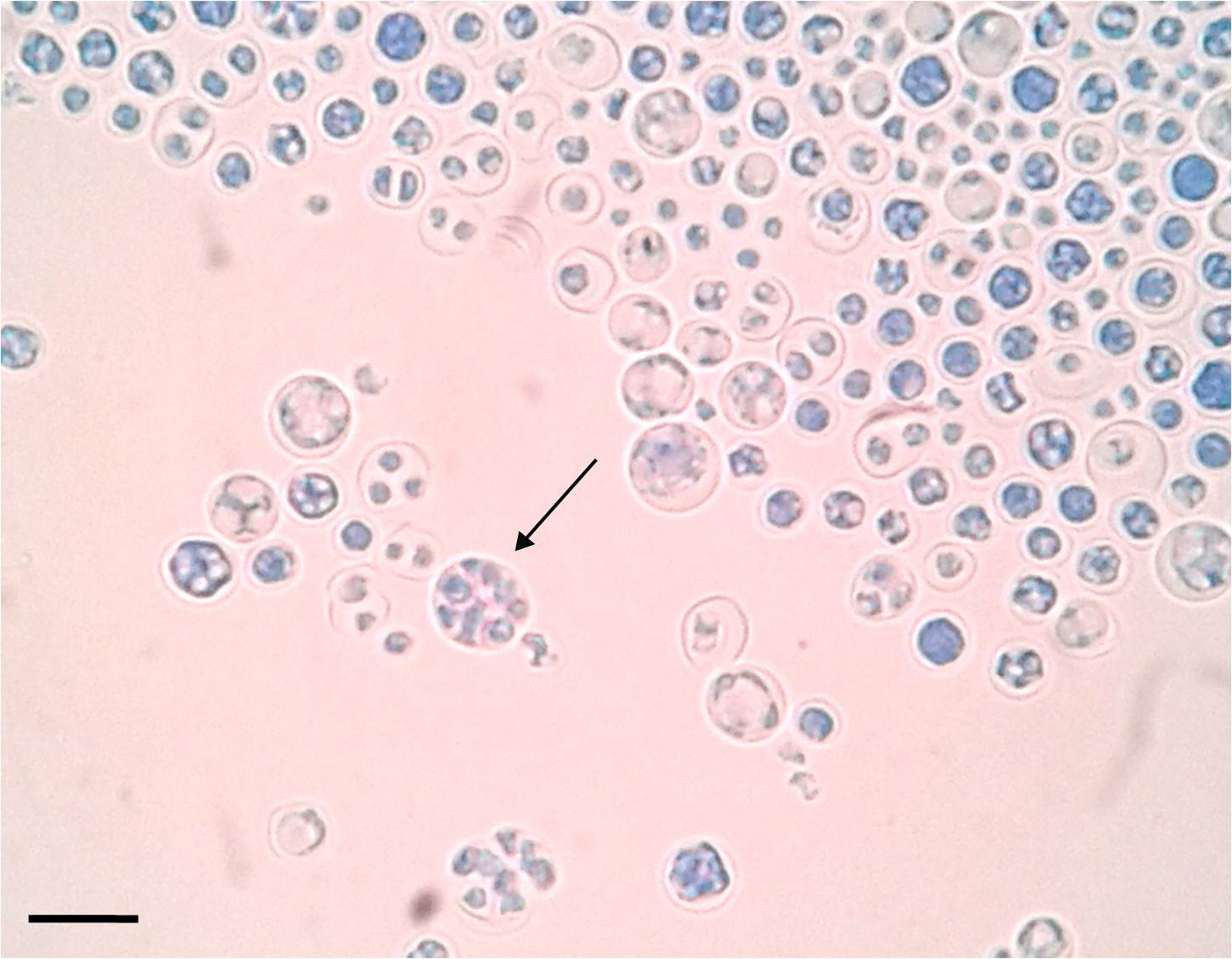
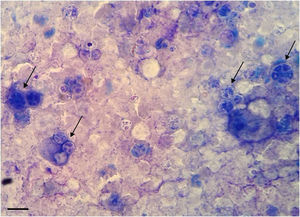
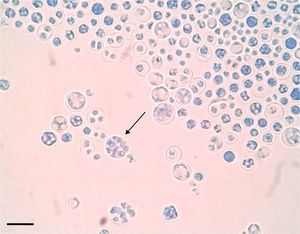
At day 0, the direct examination and Giemsa stain of the fourth abscess puncture revealed non-budding structures with morula-like appearance and sporangia (thecas), containing endospores, suggestive of Prototheca species (Fig. 2). The sample was inoculated onto Sabouraud's glucose agar (SGA) containing chloramphenicol and incubated at 37°C. After 48h, cultures showed cream whitish yeast-like colonies (Fig. 3). The agent was identified as P. wickerhamii using the API 20 C AUX V3.0 identification system (Profile 7040040) (bioMérieux, Marcy 64 l’Etoile, France). Antifungal susceptibility testing was determined using the broth microdilution method according to document M27-A3 CLSI3. Minimal inhibitory concentrations obtained were: fluconazole>64μg/ml; voriconazole 1μg/ml; itraconazole 2μg/ml; amphotericin B 0.5μg/ml; terbinafine>16μg/ml. Treatment was started with amphotericin B deoxycholate 0.7mg/kg/day to complete 3g.
In April 2015, the patient's condition worsened and was hospitalized in the intensive care unit, where she died two days later of a possible hemophagocytic syndrome.
DiscussionProtothecosis is a rare infection that is generally not suspected and its pathogenesis is largely unknown. Protothecal infection occurs mainly in immunocompromised patients with alterations in innate or cellular immunity12. Patients under steroid treatment, with diabetes mellitus, solid-tissue or hematologic malignancy (acute myelogenous leukemia, Hodgkin lymphoma, and chronic lymphocytic leukemia) are somehow at risk of protothecosis8,11,12. In this case, T-LGL leukemia could have been the predisposing factor that favored histoplasmosis and protothecosis.
Prototheca spp. are noted on routine hematoxylin–eosin staining but are best visualized with periodic acid-Schiff and Gomori methenamine-silver histochemical stains5. If endosporulation is found, Prototheca is easily recognizable in tissue, but if the morula is not present, it may be confused by inexperienced personnel. The lack of characteristic endospores causes Prototheca to resemble non-sporulating cells of Blastomyces dermatitidis, Cryptococcus spp., Paracoccidioides spp., and some stages of Coccidioides spp., Pneumocystis jirovecii, Rhinosporidium seeberi. Thus, diagnosis of Prototheca species infection by histopathology can be difficult5,6,8,10. In our case, direct examination of the purulent collection allowed a fast diagnosis, since asexual sporangia containing endospores were clearly and easily distinguished. However, in the biopsy of the second abscess, Prototheca was not observed and in the third one, P. brasiliensis was reported in the histopathological study. Although the diagnosis of protothecosis was confirmed in our Institute when the fourth abscess developed, the patient spent five years through different health centers without an accurate diagnosis. Protothecosis can be diagnosed from histopathological staining, but microbiological studies are required for an accurate diagnosis. In none of those opportunities the culture was made, which delayed the diagnosis.
At present, there are no available guidelines for the performance and interpretation of susceptibility testing for this genus. Furthermore, it is known that there is no direct correlation between in vitro activity and clinical response, with the exception of a few cases7,13. In the case reported, the performance and breakpoint interpretations were based on CLSI document M27-A3 for Candida3. In general, Prototheca species are susceptible to amphotericin B and variable to azoles such as fluconazole, itraconazole, and voriconazole2,7,9. In this case, the P. wickerhamii isolate showed high MIC against most tested antifungals except for AMB. Due to the patient's death, the therapeutic response could not be evaluated.
Around 160 cases of protothecosis have been reported worldwide12. To our knowledge, this is the first reported clinical case of protothecosis in a patient suffering from chronic leukemia and with a history of histoplasmosis.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflict of interest to declare.
We gratefully acknowledge Prof. Mariana Climent for checking the English language of the manuscript.