Percutaneous mitral valvuloplasty is the treatment of choice for rheumatic mitral stenosis with favorable anatomy, for its ability to prevent complications inherent to a surgical procedure, while maintaining effectiveness. It is necessary to promote comparisons between the results obtained by the procedure performed at referral centers with high patient inflow and at institutions with lower volume and fewer patients, which represents the main objective of this study.
MethodsThirty-one consecutive patients undergoing percutaneous mitral valvuloplasty were analyzed from September 2006 to January 2015. Immediate procedural success and late event-free survival rates were evaluated, defined as cardiovascular death or need for a new mitral valve intervention.
ResultsThe mean age was 40.9 ± 14.2 years, with a predominance of females (96.8%). The mean Wilkins and Block score was 8.1 ± 1.2. All procedures were performed using the Inoue technique, with an immediate success rate of 90.3%. At mean follow-up of 6.8 ± 2.5 years, seven events (22.6%) were observed: two cardiovascular deaths, four surgeries for mitral valve replacement, and one mitral commissurotomy.
ConclusionsIn a hospital with intermediate procedure volume, the results of percutaneous mitral valvuloplasty in the treatment of rheumatic mitral stenosis with favorable anatomy were comparable to those achieved by high-volume centers.
A valvoplastia mitral percutânea é o tratamento de escolha da estenose mitral reumática com anatomia favorável, por sua capacidade de prevenir complicações inerentes ao tratamento cirúrgico e com manutenção da eficácia. Faz-se necessário promover comparações entre os resultados obtidos com o procedimento por centros de referência e alta drenagem de pacientes e por instituições de menor volume e casuística, sendo este o objetivo principal deste estudo.
MétodosForam analisados 31 pacientes consecutivos submetidos à valvoplastia mitral percutânea no período de setembro de 2006 a janeiro de 2015. Avaliaram-se o sucesso imediato do procedimento e a sobrevida livre de eventos tardios, definidos como morte cardiovascular ou necessidade de nova intervenção valvar mitral.
ResultadosA média de idade foi de 40,9 ± 14,2 anos, com predomínio do sexo feminino (96,8%). O escore médio de Wilkins e Block foi de 8,1 ± 1,2. A totalidade dos procedimentos foi efetivada pela técnica de Inoue, com taxa de sucesso imediato de 90,3%. Em acompanhamento médio de 6,8 ± 2,5 anos, foram constatados sete eventos (22,6%), sendo dois óbitos de etiologia cardiovascular, quatro cirurgias de troca valvar mitral e uma comissurotomia mitral.
ConclusõesEm um hospital com volume intermediário de procedimentos, os resultados da valvoplastia mitral percutânea no tratamento da estenose mitral reumática com anatomia favorável foram comparáveis àqueles alcançados por centros de alto referenciamento.
The prevalence of rheumatic fever, the predominant etiology of mitral stenosis, has undergone a significant reduction in Western countries, but percutaneous mitral valvuloplasty (PMV) is still the treatment of choice in patients with favorable valve anatomy, for its ability to prevent complications inherent to the surgical procedure, while maintaining effectiveness.1–3 The procedure can be accomplished by different methods, such as the single balloon, double balloon, or metallic commissurotomy method, with the Inoue4 technique representing the most commonly used, as it is simpler to perform, has a shorter procedure duration, and has lower incidence of complications, with late evolution comparable to that of the others.5–7
In spite of the frequent need for reinterventions after a successful PMV, survival free of cardiovascular death, surgical valve replacement or NYHA class III or IV are approximately 50% in a follow-up period of up to 20 years in high-volume centers.8,9 It is necessary, however, to promote comparisons between the results obtained with the procedure as performed by referral centers with high patient inflow and by institutions with lower volume and fewer patients, which represents the main objective of this study.
MethodsStudy populationThe study population consisted of a cohort of 31 consecutive patients with moderate to severe mitral stenosis of rheumatic etiology (mitral valve area ≤ 1.5cm2), clinically symptomatic (functional class > II), with favorable valve morphology, submitted to PMV at Santa Casa de Marília, in Marília (SP), Brazil, from September 2006 to January 2015.
ProceduresUnder superficial sedation and local anesthesia, right femoral venous access was obtained with a 7 F femoral sheath, while left femoral arterial access was obtained with a 5 F femoral sheath. Pulmonary capillary, main pulmonary artery, right ventricle, right atrium, left ventricle, and aorta pressures were obtained retrogradely. Left ventriculography was performed in right anterior oblique projection at 30°, and the degree of mitral regurgitation was established according to Sellers’ classification. In patients older than 40 years, the assessment was complemented with coronary angiography.
The Brockenbrough technique was used for the transseptal puncture, under continuous pressure monitoring and using a pigtail catheter positioned above the aortic valve as reference. After the transseptal puncture, a Mullins catheter was maintained in the left atrial cavity, and 2,500 IU of heparin were administered. After the mitral valve pressure gradient was recorded, the spiral guidewire was introduced up to the left atrium, followed by atrial septum dilation using a 14 F dilator. The Inoue balloon size was determined by the formula given by the equation:
maximum balloon diameter (mm) = [patient's height (m) × 10] + 10
The balloon was advanced over the guidewire, with its distal extremity close to the mitral valve orifice. The balloon was then partially inflated with 1 to 2mL of diluted contrast to facilitate its fluctuation through the valve orifice and prevent its passage through the chordae tendineae. With the help of a stylet, the balloon was directed in order to surpass the mitral valve. The distal portion of the balloon was inflated and the set was retracted up to its anchoring position at the ventricular face of the mitral valve. Then, the proximal portion of the balloon was inflated, resulting in an hourglass shape, until the medial constraint disappeared at full inflation. The pigtail catheter was advanced into the left ventricular cavity for analysis of residual mitral gradient. When available, two-dimensional transthoracic echocardiography was performed at this point. If the result was considered inadequate, the balloon was introduced again for additional inflations with larger volume. At the end of the procedure, manometry of the right chambers and the control left ventriculography were recorded. Echocardiography was routinely performed 24 to 48hours after the PMV, with the mitral valve area being assessed by planimetry.
Definitions and outcomes of interestProcedural success was defined by the increase in mitral valve area ≥ 25% of the original area and final valve area ≥ 1.5cm, in the absence of severe mitral regurgitation (> 2/4) and severe cardiac or cerebrovascular adverse events, such as death, stroke, cardiac tamponade, or mitral valve surgery. The outcomes assessed in the late follow-up were cardiovascular death and the need for a new percutaneous or surgical mitral valve intervention.
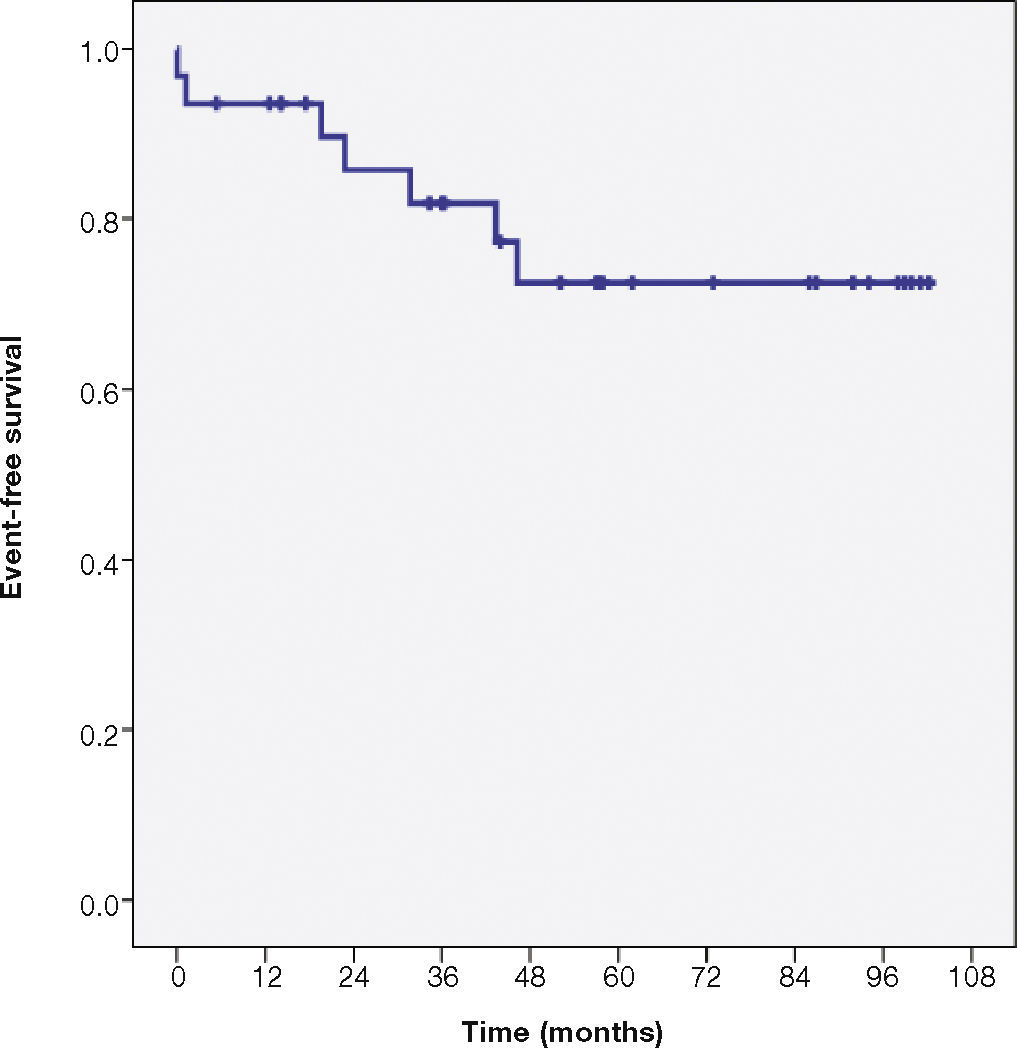
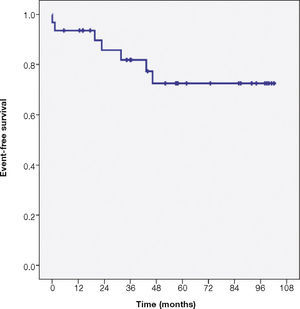
Statistical analysisAll data were prospectively stored in a registry started in 2006. The estimate of event-free survival was determined according to the Kaplan-Meier method. The qualitative variables were summarized as absolute frequencies and percentages. Quantitative data were expressed as means and standard deviations.
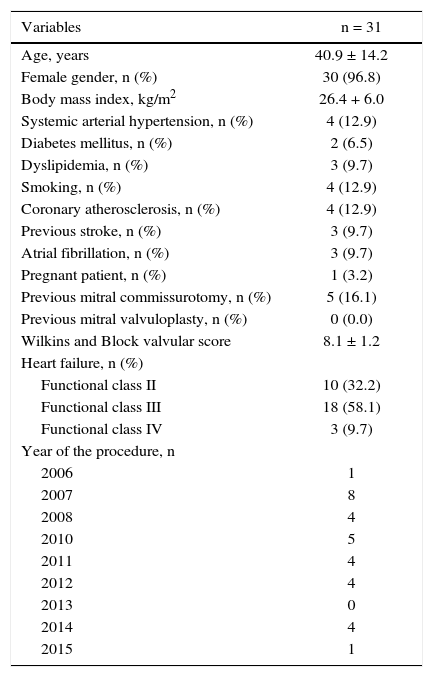
ResultsClinical and demographic characteristics of patients are shown in Table 1. The mean age was 40.9 ± 14.2 years, with a predominance of females (96.8%). The mean Wilkins and Block score was 8.1 ± 1.2. Among the procedures, one was performed in a pregnant woman and five in patients with previous mitral commissurotomy. After 2007, there was stabilization in the mean volume of cases, with the performance of approximately four PMVs per year.
Clinical and demographic characteristics of patients.
| Variables | n = 31 |
|---|---|
| Age, years | 40.9 ± 14.2 |
| Female gender, n (%) | 30 (96.8) |
| Body mass index, kg/m2 | 26.4 + 6.0 |
| Systemic arterial hypertension, n (%) | 4 (12.9) |
| Diabetes mellitus, n (%) | 2 (6.5) |
| Dyslipidemia, n (%) | 3 (9.7) |
| Smoking, n (%) | 4 (12.9) |
| Coronary atherosclerosis, n (%) | 4 (12.9) |
| Previous stroke, n (%) | 3 (9.7) |
| Atrial fibrillation, n (%) | 3 (9.7) |
| Pregnant patient, n (%) | 1 (3.2) |
| Previous mitral commissurotomy, n (%) | 5 (16.1) |
| Previous mitral valvuloplasty, n (%) | 0 (0.0) |
| Wilkins and Block valvular score | 8.1 ± 1.2 |
| Heart failure, n (%) | |
| Functional class II | 10 (32.2) |
| Functional class III | 18 (58.1) |
| Functional class IV | 3 (9.7) |
| Year of the procedure, n | |
| 2006 | 1 |
| 2007 | 8 |
| 2008 | 4 |
| 2010 | 5 |
| 2011 | 4 |
| 2012 | 4 |
| 2013 | 0 |
| 2014 | 4 |
| 2015 | 1 |
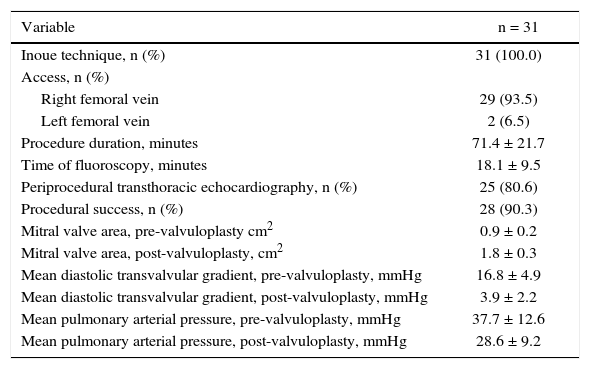
All of the procedures were carried out using the Inoue technique. The success rate was 90.3%, and the three unsuccessful procedures were attributed to transseptal puncture failure (n = 2) and cardiac tamponade (n = 1). Transthoracic echocardiography monitoring was used in 80.6% of cases. The characteristics of the echocardiographic procedures and information are shown in Table 2.
Characteristics and outcomes of percutaneous mitral valvuloplasty.
| Variable | n = 31 |
|---|---|
| Inoue technique, n (%) | 31 (100.0) |
| Access, n (%) | |
| Right femoral vein | 29 (93.5) |
| Left femoral vein | 2 (6.5) |
| Procedure duration, minutes | 71.4 ± 21.7 |
| Time of fluoroscopy, minutes | 18.1 ± 9.5 |
| Periprocedural transthoracic echocardiography, n (%) | 25 (80.6) |
| Procedural success, n (%) | 28 (90.3) |
| Mitral valve area, pre-valvuloplasty cm2 | 0.9 ± 0.2 |
| Mitral valve area, post-valvuloplasty, cm2 | 1.8 ± 0.3 |
| Mean diastolic transvalvular gradient, pre-valvuloplasty, mmHg | 16.8 ± 4.9 |
| Mean diastolic transvalvular gradient, post-valvuloplasty, mmHg | 3.9 ± 2.2 |
| Mean pulmonary arterial pressure, pre-valvuloplasty, mmHg | 37.7 ± 12.6 |
| Mean pulmonary arterial pressure, post-valvuloplasty, mmHg | 28.6 ± 9.2 |
Seven events (22.6%) were observed during a mean follow-up of 6.8 ± 2.5 years: two cardiovascular deaths, four mitral valve replacement surgeries, and one mitral commissurotomy. The estimate of event-free survival at 8 years by the Kaplan-Meier method was 72.5% (Fig. 1). In the subgroup of patients with previous mitral commissurotomy (16.1%), immediate success was obtained in all cases, and the late follow-up showed one case of restenosis with mitral valve replacement surgery.
DiscussionA pioneering modality in the non-surgical approach to acquired valvular disease, PMV is a complex procedure, associated with a learning curve, especially due to the need for transseptal puncture. Late outcomes of large series of patients have been recently published, demonstrating that it is a well-established technique that brings long-term benefits to patient prognosis.
Of the 1,024 patients undergoing PMV between the years 1986 and 1995 in France, the survival free of cardiovascular death or new surgical or percutaneous mitral valve intervention in 20 years was 30.2%.9 In mean follow-up of 11.6 years of 482 patients who underwent the procedure in an Italian registry, the event rate was 41.9%, mainly due to the need for mitral valve surgery (27%).10 In Brazil, very late outcomes involving up to 308 patients demonstrated lasting results, with restenosis-free survival over 20 years in more than one-third of the cases.11,12 Together, these data reflect the experience of major referral centers in structural interventions with high patient inflow.
The present series, although modest, shows a high success rate, and low complication and event-free survival rates, comparable to those in large centers.13 Some aspects may justify these findings. The main aspect is the selection of patients favorable to the used technique, such as non-advanced age, prevalence of sinus rhythm (90.3%), and mean echocardiographic score of 8.1 – factors that are known to be associated with better late outcomes.9,12,14 Speculatively, another strategy used on a recurring basis and that could help prevent complications was the periprocedural echocardiographic monitoring in 80.6% of cases. As the echocardiography in the intervention laboratory provides fast and accurate information of the mitral valve area and the degree of regurgitation, additional balloon inflations can be prevented and the subsequent establishment or worsening of valve regurgitation.
A subgroup of patients undergoing PMV of special interest are those with restenosis after surgical mitral commissurotomy, as percutaneous treatment, when feasible, prevents valve replacement and its consequent late implications. However, the previous commissurotomy is traditionally considered a variable that predicts worse immediate and late post-procedural outcomes.15 The present data were favorable in this population, in line with the most recent publications, which show immediate success in over 80% of cases and survival free of mitral surgery in 20 years in up to one-third of the patients.16
The main limitation of the study was the small sample size and the reproducibility of its findings. Despite the intermediate volume of procedures, the interventionists involved with these procedures directly participated, during their training, in approximately 30 PMV, thus meeting the learning curve. With the decrease in the prevalence of rheumatic mitral stenosis, acquiring proficiency in the stages of the procedure, such as transseptal puncture, becomes impaired. However, the advent of new imaging technologies and devices applicable in several types of structural and degenerative diseases, the left atrial appendage closure in patients with atrial fibrillation, and the therapeutic role in arrhythmias have the potential to rescue the puncture technique due to the common need to have antegrade access to the left atrium.
ConclusionsThe results obtained with the Inoue technique in percutaneous mitral valvuloplasty in patients with rheumatic mitral stenosis in a tertiary hospital with an intermediate volume of structural procedures were comparable to those achieved by reference centers with high patient inflow.
Funding sourceNone declared.
Conflicts of interestThe authors declare no conflicts of interest.
Peer review under the responsibility of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.