Human behaviours have different meanings depending on the historical moment and context. In this article, we analyse the way in which psychiatric nosology is structured in texts such as the DSM-5 by studying the category of sexual behaviours. The very design of these diagnostic manuals, in terms of their notion of health, disease, mental health and mental disorders, in short, what is normal and what is pathological, shows that they are far from objective tools, and are very much influenced by certain elements of power.
Each new diagnosis, or even the removal of existing diagnoses and the recomposition of the different diagnostic criteria, particularly in the field of sexual behaviour, represents a particular view of individual and collective human life, and constitutes an attempt to control human sexuality by medicalising behaviours and bringing to bear moral, religious and even legal considerations.
Categories such as gender dysphoria, paraphilia or paraphilic disorders are examples of how the limits imposed on biomedical perspectives, in addition to being incomplete and imprecise, violate the individual and social construction of sexual behaviour and the very notion of mental health, and are evidence of the ongoing difficulties and controversies involved in drawing up psychiatric classifications.
Los comportamientos humanos tienen diferentes significados según el momento histórico y el contexto. En este artículo se toman los comportamientos sexuales como categoría que permite analizar la manera en que se estructura la nosología psiquiátrica manifiesta en textos como el DSM-5. El desarrollo de estos manuales diagnósticos dista de hacerlos herramientas libres de subjetividades y de la injerencia de elementos de poder, expresados en cómo se asumen la salud, la enfermedad, la salud mental y los trastornos mentales, en suma, lo normal y lo patológico.
Cada nuevo diagnóstico o incluso su eliminación y la recomposición de los distintos criterios diagnósticos, especialmente en el campo de los comportamientos sexuales, representan visiones de cómo se concibe la vida humana individual y colectiva y una expresión de los intentos certeros de controlar las sexualidades humanas por medio de la medicalización de los comportamientos, a lo cual se suman consideraciones morales, religiosas e incluso legales.
Categorías como la disforia de género, las parafilias o los trastornos parafílicos son ejemplos de cómo los límites que se pretende instituir a una perspectiva biomédica son, además de incompletos e imprecisos, hechos que violentan la construcción individual y social de las sexualidades y la concepción misma de salud mental, con lo que se evidencian las dificultades y las controversias persistentes en cómo se elaboran las clasificaciones psiquiátricas.
Christian religions have considered the act of engaging in certain sexual behaviours not for the procreation of children to be a sin, or at least, something to be avoided.1–4 These behaviours have even been considered illegal and could be punishable by law.5–9 In the process of identifying the causes or predisposing factors for such “criminal” sexual behaviour, physicians and psychologists chose to categorise them as a “disease” or “mental disorder”, thus enabling them to be medicalised, pathologised and psychologised.5,10–13 Just as the “diagnosis” and aspects associated with the clinical context confer authority on the medical profession in general and doctors in particular, so mental disorder “empowers” psychiatry and psychiatrists.14
The medicalisation of sexual behaviours has been institutionalised by including them in international disease classification systems, such as the International Classification of Diseases of the World Health Organisation (WHO),15 and the Diagnostic and Statistical Manual of the American Psychiatric Association (APA).16 This has only fuelled the anti-hegemonic position of groups fighting for sexual equality and diversity who seek to exclude certain behaviours from such classifications.10–12,16–18
The aim of this review is to analyse the mental disorders’ categories listed in the most recent APA classification, the DSM-5, that include certain sexual behaviours among their diagnostic criteria.
BackgroundIn view of the controversy surrounding each new version of the DSM,19,20 the most recent version (DSM-5) updates the principles of the manual and introduces certain changes in the general approach to understanding or interpreting the thoughts, emotions and behaviours that can be considered to be involved in a mental disorder.21
However, given the growing importance of psychiatry in medicine,11,12,17,18 it is important to bear in mind that the definition of “disease” in the context of “physical” entities is far from straightforward, and can be interpreted in many different ways.22 The most prominent approach to defining disease, called “naturalism”, revolves around the notion that “disease” has a biological basis comprised of “reference functional classes” or uniform organisms, according to the sex or age of the species.23 This validates the notion of normal function, with a statistically typical distribution that allows for survival and reproduction of the species. Thus, “disease” is an abnormal functioning of the organism, and “health” is the absence of disease.22,23 A second approach is known as “normativism”. Normativism understands “disease” as a deviancy from a state of affairs which is considered more desirable, implying a gap between presented behaviour (or feeling) and established social norms.22 Thus, the definition of “health” includes a judgement, a pattern, of what is allowed or accepted, and consequently “disease” is the situation that deviates from the socially established norm.22,24 Finally, a third, hybrid perspective incorporates the favourable aspects and limitations of naturalism and normativism to define the health-disease phenomenon, since together they better explain a greater number of cases considered to involve “disease”.22 The current notion of “disease” is based on the presence of a body alteration that manifests as predictable signs and symptoms. According to naturalism, this is caused by damage to the structure or functioning of the diseased organ, while from the normativist perspective, the “disease” is intangible, essentially conceptual and inferential, and associated with the concept of “normality” in a particular context.22–24
From an institutional perspective, the WHO defines mental health as “a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community”.25 For its part, the APA defines “mental disorder” as “a mental disorder is a syndrome characterized by clinically significant disturbance in an individual's cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning. Mental disorders are usually associated with significant distress in social, occupational, or other important activities. An expectable or culturally approved response to a common stressor or loss, such as the death of a loved one, is not a mental disorder. Socially deviant behavior (e.g., political, religious, or sexual) and conflicts that are primarily between the individual and society are not mental disorders unless the deviance or conflict results from a dysfunction in the individual, as described above”.16
In Colombia, Act 1616 of 2013 defines mental health as “a dynamic state that is expressed in everyday life through behaviour and interaction in such a way as to allow individuals and groups to deploy their emotional, cognitive and mental resources to live their daily life, to work, to establish meaningful relationships and to contribute to the community”.26 This approach to mental health echoes the basic elements of the WHO's definition,25 and differs from a mental disorder as defined by the APA. Furthermore, it upholds as vital the bond between individuals and the productive apparatus, and thus validates the prevailing economic system in the western world.16
In light of the general definition of “disease”, the notion of “mental disorder” currently poses a major problem, since no studies have so far shown the existence of brain damage or dysfunction specific to each so-called mental disorder, so the signs and symptoms observed are assumed to be indirect manifestations of a lesion or functional alteration in a particular part of the brain.11,12,22–24,27 Similarly, the normativist component is more evident in the definition of “mental disorder” than in “physical disease”, since it explains the importance of cultural and contextual factors in reaching a formal diagnosis of “mental disorder”.12,22 In other words, it classes the set of symptoms as mental “illness” or “disorder”, with no clear aetiological, physiological or pathological explanation, thereby transforming a theoretical construct into a tangible entity.28
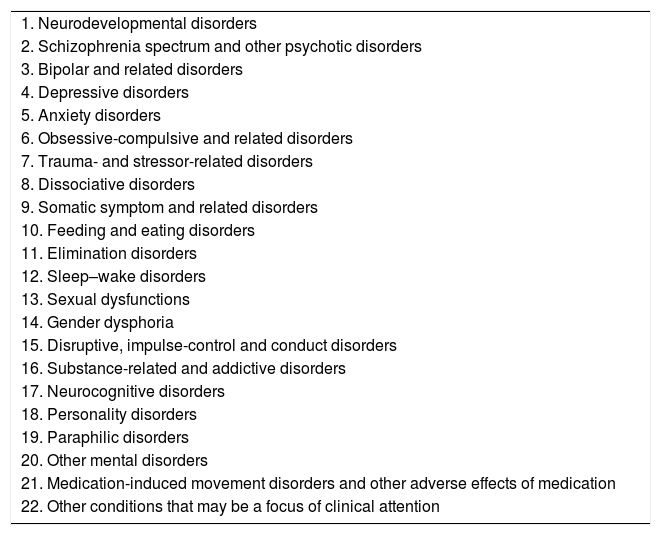
The DSM-5 follows a neurobiological model, and attempts, without fully succeeding, to present mental disorders as a spectrum of categories. It is arranged according to the main diagnoses, starting with neurodevelopmental disorders and ending with “other problems that may be the focus of clinical attention”29,30 (Table 1). The most important change made to categories that include sexual behaviours among their diagnostic criteria involves grouping the “disorders” included in these categories into three separate classes: sexual dysfunction, gender dysphoria and paraphilic disorders.31
Diagnostic categories.
| 1. Neurodevelopmental disorders |
| 2. Schizophrenia spectrum and other psychotic disorders |
| 3. Bipolar and related disorders |
| 4. Depressive disorders |
| 5. Anxiety disorders |
| 6. Obsessive-compulsive and related disorders |
| 7. Trauma- and stressor-related disorders |
| 8. Dissociative disorders |
| 9. Somatic symptom and related disorders |
| 10. Feeding and eating disorders |
| 11. Elimination disorders |
| 12. Sleep–wake disorders |
| 13. Sexual dysfunctions |
| 14. Gender dysphoria |
| 15. Disruptive, impulse-control and conduct disorders |
| 16. Substance-related and addictive disorders |
| 17. Neurocognitive disorders |
| 18. Personality disorders |
| 19. Paraphilic disorders |
| 20. Other mental disorders |
| 21. Medication-induced movement disorders and other adverse effects of medication |
| 22. Other conditions that may be a focus of clinical attention |
Based on DMS-5.16
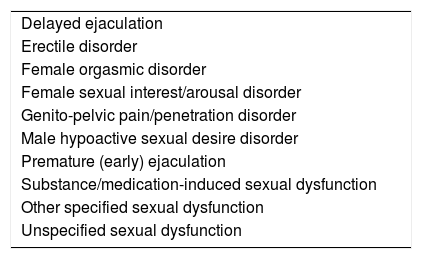
Sexual dysfunctions, based on the traditional physiological model of sexual response, are defined according to the different stages of sexual response: desire, arousal, plateau and resolution, the difference being that they occur exclusively between women and men16 (Table 2).
Sexual dysfunctions.
| Delayed ejaculation |
| Erectile disorder |
| Female orgasmic disorder |
| Female sexual interest/arousal disorder |
| Genito-pelvic pain/penetration disorder |
| Male hypoactive sexual desire disorder |
| Premature (early) ejaculation |
| Substance/medication-induced sexual dysfunction |
| Other specified sexual dysfunction |
| Unspecified sexual dysfunction |
Based on DMS-5.16
The main change regarding sexual behaviours is that sexual dysfunctions are now considered clinically distinct entities, significantly disconnected from gender behaviour which, however, is placed immediately after sexual dysfunctions.16 The new edition has eliminated, or has no equivalent for, “sexual aversion disorder”.32 Likewise, “female sexual interest/arousal disorder” combines two overlapping disorders which in the previous classification were presented as distinct: the “hypoactive sexual desire disorder” and the “female sexual arousal disorder”. The same has occurred with “dyspareunia” and “vaginismus”, which are regrouped as genito-pelvic pain/penetration disorder, thus placing more emphasis on penetration than on vaginal spasm for diagnosis.33,34 These changes could improve the validity and reliability of these diagnoses.33 Disorders included in this category are detailed in Table 3.
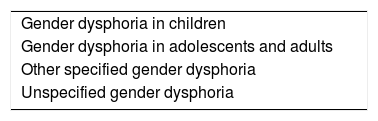
Gender dysphoria.
| Gender dysphoria in children |
| Gender dysphoria in adolescents and adults |
| Other specified gender dysphoria |
| Unspecified gender dysphoria |
Based on DMS-5.16
In “gender dysphoria”, formerly referred to as “gender identity disorder”, the exclusion criterion “intersex conditions” found in DSM-IV has been removed. However, it includes specifiers for concomitant sexual development disorders and the process of gender reassignment. Sexual orientation specifiers have been removed from the most recent version.34 In addition, clinicians must specify whether they are observed in the presence of a sexual developmental disorder, such as congenital adrenogenital disorder, congenital adrenal hyperplasia or androgen insensitivity syndrome. Likewise, a coding note for both gender dysphoria and sexual development disorder codes is added.16
The second change involves relocating paraphilic disorders from “sexual disorders” into a different category that occurs after personality disorders.29–31 This shows the renewed approach to paraphilic disorders as being more closely related to personality traits, as stable or persistent behavioural patterns that are difficult to substantially modify, and as entities that, if clinically significant, are sufficiently distinct from sexual dysfunctions and gender dysphoria.31
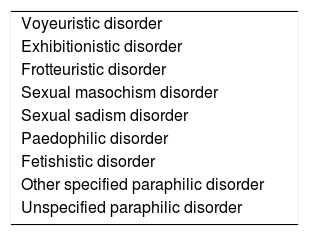
Likewise, a distinction is made between “paraphilia” and “paraphilic disorders”. The DSM-5 defines paraphilia as “any intense or persistent sexual interest other than sexual interest in genital stimulation or preparatory fondling with phenotypically normal, physically mature, consenting human partners”, and “paraphilic disorders” as paraphilias that cause distress, impairment or harm to others.16 The presence of paraphilia, albeit in association with other conditions, is necessary for the diagnosis of paraphilic disorder (Table 4).35
Paraphilic disorders.
| Voyeuristic disorder |
| Exhibitionistic disorder |
| Frotteuristic disorder |
| Sexual masochism disorder |
| Sexual sadism disorder |
| Paedophilic disorder |
| Fetishistic disorder |
| Other specified paraphilic disorder |
| Unspecified paraphilic disorder |
Based on DMS-5.16
On the one hand, it is very complicated to accurately differentiate between these two “conditions” and furthermore, in both groups, sexual desires not exclusively focused on the genitals are considered “pathological”. Merely differentiating between these disorders does not in itself indicate when they will require treatment or clinical interventions, since a paraphilia does not necessarily involve a paraphilic disorder.31,36 These categories are a good example of the use of medicine as a biopower that controls both the bodies and behaviours of individual subjects.37
On the other hand, “in remission” and “in a controlled environment” specifiers are included if the person is in an environment where he or she cannot engage in paraphilia.34 In addition, age differences are needed for the definition of paedophile disorder.38
In cases of voyeurism, it should be specified whether the subject is sexually aroused by exposing their genitals to prepubertal children, sexually aroused by exposing their genitals to physically mature individuals, or sexually aroused by exposing their genitals to prepubertal or physically mature individuals.16,31 For sexual masochism, the presence of asphyxiophilia must be specified. And in the case of transvestic disorder, clinicians must specify if the conditions coexist with fetishism or autogynephilia.16,36
Likewise, mention is made of sexual behaviour in criterion A, subsection 4, of borderline personality disorder in relation to impulsivity, which may be self-injurious in some way (e.g. spending, sex, drugs, reckless driving, binge eating, etc.).16
DiscussionThese three sections, and in particular the section on paraphilic disorders, show several contradictions that warrant a detailed review, and it is clear that the gender dysphoria category should have been omitted from this version of the DSM.5,31–33
Classifications, both in medicine in general and in psychiatry in particular, can give rise to reification and lend substance to theories and hypotheses. They can also legitimise the arbitrary categorisation of human behaviour and the social exclusion of people who “deviate” from hegemonic precepts, in an exercise of varying powers.20,22,28,39 The application of DSM-5 criteria will no doubt increase the number of diagnoses given, fashionable diagnoses will appear, normality and daily life will be medicalised, and mental disorders will become practically ubiquitous. The vast majority of people will fulfil some diagnostic criteria at some time in their lives, thus turning the global village into a community of mentally disturbed individuals.17,30
In relation to sexual behaviour, Di Segni observes that medicalisation has turned “natural” acts into ethical and moral considerations.10 And given the heuristic impression that many of these behaviours are the rule and not the exception, conventional “normality” calls for “abnormality” to be the most exceptional, and not the most common, behaviour. Furthermore, “oddity” is not a value in itself, and therefore should not be taken in psychiatry to mean “mental disorder”. In other words, it would appear that the “disorder” aspect of sexual behaviour is used to bring “rebels” into line, outlawing the use of sexuality purely for “naturalistic” purposes, and this is closer to authoritarian morality than to scientific endeavour. Medicine and psychiatry displaced religion and legal codes when they became the new “authority” over sexual behaviour in the context of a prevailing economic model based on capital and market expansion that introduced drugs and therapies designed to modify the new disorders, a situation that perfectly conforms to what has been described as the medical-industrial complex.40 We must understand that sexuality takes many forms, and the usual binarism (dichotomy) used to evaluate sexual behaviour (good-bad, permitted-forbidden) must be set aside. In human sexuality, diversity or multiplicity is the norm; it is not important what you do, but the context in which you do it.5
Although the APA tends to de-stigmatise non-standard, non-traditional or non-hegemonic sexual behaviours, according to the current classification, sexual desires at the upper limit of “normal” are included among sexual dysfunctions, controversially considering these variations of normal as “pathological” and assigning them diagnoses.41 Considering “female sexual interest/arousal disorder” and “male hypoactive sexual desire disorder” as clinical entities that warrant treatment ignores the fact that it is very difficult to define “normal” sexual desire, and will probably give rise to a large number of false positives,42 since there are no obvious differences between individuals with “normal” and “abnormal” sexual desires.41,43,44 If this is so, it would suggest, for example, that Catholic priests, who in theory must remain celibate, present one of these disorders. Although some will say that sexual desire can be managed and sublimated through the Catholic faith, this means that those who are not priests but engage in the same behaviour will indeed fulfil the criteria for one of these disorders. In this case, the absence of faith turns a behaviour into a disorder. These simple examples highlight the ambiguity of the inclusion of sexual desire “problems” in DSM-5.41,44
On the other hand, the diversity of sexual expression is not only due to constitutional, genetic and biological factors,45 but also to cultural components that shape the public and private sex lives of individuals.46,47 In summary, the social and medical differences on which sexuality is constructed are unknown.45,48,49 Sexual expression is so diverse and socially dependent that new forms have been introduced in recent decades with the advent of the Internet,50–52 and with them, new behaviours to pathologise.53,54
Gender dysphoria is undoubtedly the most controversial new category.31,32,36 Although some authors suggest that removing the word “disorder” from the description is a positive move, since “dysphoria” is a less serious situation or condition than a disorder,32 it still clearly “psychiatrises” an aspect of human behaviour.55
However, the persistence of this term in the new version of the DSM is inconsistent with other decisions related to similar conditions, specifically, with the decision to exclude homosexuality as a diagnosis, even after considering the conceptual differences between gender and sexual orientation.56–58 Likewise, the name “gender dysphoria” is exclusive and allows the stigma attached to trans people to persist.59 This process is similar to that spearheaded by the psychiatrist Robert Spitzer in 1973 within the APA, which led to the exclusion of homosexuality from the diagnostic manual, a decision, according to some, that owed more to politics than to science.31,60–62
Critics of the gender dysphoria diagnosis consider it to be related to prejudices that persist in the classification work group and in psychiatry in general, a field which has historically been tainted with racism, misogyny and homophobia, etc.,63,64 not to mention the links between psychiatrists and the Nazi regime,65,66 and more recently the role of some psychologists in the torture carried out by the United States Central Intelligence Agency, as stated in the 2015 Hoffman Report.67 In fact, Robert Spitzer himself published an article in 2001 showing the possibility of a “cure” for homosexuality.68 A decade later, he retracted the article and apologised to the gay community for falsely concluding in his study that “conversion therapy” can be effective in homosexual men and women.69
Gender dysphoria probably persists in DSM-5 due to the difficulty of completely reversing the tendency to consider any dissident sexual behaviour as a disease.5 This is evidence of a particularly biased and sexist view of sexuality that harks back to Victorian times, when medical knowledge was exclusively shaped by middle-class “heterosexual” males.5,70
Similarly, gender dysphoria is still classed as a mental disorder because medicine has a limited, dichotomous view of this component of sexual behaviour.5 Psychiatry is no stranger to this phenomenon, and expects gender expression to fully match the observed biological sex.5,11 Daily life and clinical practice show the extent to which biological sex and gender can diverge.5,11,12,28,71
However, most optimists expect gender dysphoria to be removed from a forthcoming version of the DSM due as much to the absence of studies that support the diagnosis as to constant calls for exclusion by political activists.5,32,71,72 This again proves that “diagnosis” is not only the result of scientific research, but also of political lobbying.12
With regard to paraphilic disorders, voyeurism, exhibitionism, frotteurism and paedophilia are behaviours that do not consider the consent of one or more participants,31,32,36 and it would be more appropriate to include them in criterion A, “…a pervasive pattern of disregard for and violation of the rights of others”, subsection 1 “failure to conform to social norms with respect to lawful behaviours” of the section on antisocial personality disorder. It is obvious that this requires eliminating the adjective “pervasive”. If these behaviours involve children or adolescents, the criterion “aggression towards people or animals and serious breach of norms”, which describes behavioural disorder, should be taken as a reference.16 Abuse, non-consensual or coerced sexual behaviours should be considered legal problems that should therefore be dealt with by the judicial system.5,31
Similarly, fetishism, transvestism, sexual masochism and sexual sadism had to be eliminated from the current classification, since they are private behaviours that do not violate the rights of others, are consensual, and are not associated with any greater risk than the stigma of categorising a private behaviour or activity as a “disease”.5,31,32,36,73 In addition, the adjective “sexual” would appear superfluous when describing masochism and sadism, since it is not considered in contexts other than genitality.31
Equally superfluous is the specifier for paedophilia disorder (“specify whether sexually aroused by exposure of genitals to prepubertal children, sexually aroused by exposure of genitals to physically mature individuals or sexually aroused by exposure of genitals to prepubertal or physically mature individuals”), the specification of the sex that causes the attraction, and whether it occurs within a sexual relationship between people with a close degree of consanguinity. Incest is more a moral judgement,38 and is directly related to the judicial system if it involves a non-consenting individual.31 It also makes no sense to set limits on age differences in defining paedophilia disorder when adolescents that can consent without coercion are involved, since the age gap does not necessarily imply aggression or violation of the rights of one of the participants in sexual intercourse. The age at which an individual may consent to sexual activity during adolescence or once puberty begins may vary considerably according to the cultural context or legal system in place in each country.38,74,75
In the case of sexual masochism disorder, the need to “specify whether with asphyxiophilia” and for transvestism disorder, “specify whether with fetishism or autogynephilia” is based more on expert consensus than on solid scientific evidence.31,32,76
All of the above is repeated in the most recent classifications published since 1980, which have been more concerned with the reproducibility (reliability) of diagnosed “disorders” than with their validity.11,12,28,77,78 In psychiatry, validity refers to whether the set of symptoms and clinical and paraclinical findings called a disorder is a specific entity with a cause, course, treatment and prognosis that is predictable enough to consider it “real”. Reliability, on the other hand, refers to whether different evaluators conducting a clinical interview at different times to assess the clinical symptoms will reach the same decision regarding the diagnosis or the criteria to be met.79
Zucker argues that the inconsistencies of the three diagnostic categories involving sexual behaviour can be divided into five overall groups: presenting some definitions by exclusion, using insufficiently justified individual or cultural criteria, ignoring the motivation behind sexual behaviours or possible “aetiological” factors, ignoring or minimising the importance of consent to engage in a particular sexual behaviour, and finally, the lack of evidence or studies that support the validity of each “disorder”.32
As paraphilic disorders do not respond to different pharmacological and non-pharmacological interventions, it would be preferable to consider them as persistent “personality traits” which, if they harm or violate the rights or integrity of other individual, should be classed as “antisocial” traits and dealt with in the same way as any other criminal behaviour.5,16
The depathologising of some sexual behaviours as a result of changes made to international classification systems does not guarantee de-stigmatisation,62,80 and it is easier to stigmatise than to eliminate the associated discrimination.81 This suggests that many people will probably decide to consult healthcare professionals, on their own initiative or due to family, social or institutional pressure, for sexual behaviours that do not violate the rights of others and that can be considered to fall within the broad spectrum of expected, functional manifestations of sexuality.82,83
From now on, since it is necessary to “diagnose” or record a presenting problem using a predetermined code given in the current classification system, the importance of these sexual behaviours should be played down during the consultation in order to avoid psychologising, psychiatrising or medicalising them. It would be preferable and almost always correct to choose some of the diagnoses included in “Other conditions that may be a focus of clinical attention”.16
This group of less stigmatising diagnoses that do not directly refer to sexual behaviour include “relationship problems” (parent/carer or parent/child relationships, or the like: Z62.820) for cases where the relationship is adversely affected by the gender or sexual orientation of the child, and “other disorders related to socioeconomic and psychosocial circumstances” (social exclusion or rejection: Z60.4; target – perceived – of adverse discrimination or persecution: Z60.5) in situations where stigma/discrimination causes dissatisfaction with sexual identity, and “other encounters with health services” (such as sexual counselling: Z70.9) related to combined concerns regarding sexual attitude, behaviour and orientation.16“Adult antisocial behaviour” (Z72.811) or “child or adolescent antisocial behaviour” (Z72.810) may also be preferred for isolated, non-repetitive sexual behaviours that disregard the rights of others.16 This, by analogy, is the case with antisocial personality disorder, which is considered a “mental disorder”; however, when it involves a violation of the rights of others, patients are mainly dealt with within the legal system instead of the health system. This is often the recommendation in the case of sexual offences or crimes, although the health sector will be involved in the process of re-socialisation of these individuals.84,85 This is the all-important point where psychiatry and the legal system overlap, as mental disorders, particularly those with a sexual component, have historically been associated with criminal activity.84,86,87 Foucault pointed out that associating unconventional, non-hegemonic sexual behaviour with criminal acts is often a means of monitoring, disciplining, controlling and punishing any behaviour considered “immoral”.86
It should be borne in mind that nowadays the concept of “disease” in psychiatry has several limitations, which are further evidenced by calling some sexual behaviours “disorders” instead of diseases.26,77,88–90 Sexual behaviour is highly varied, and divergence or variations do not in themselves constitute a disorder.91–93 Nonetheless, the moralistic and normativist attitude of pathologising certain behaviours has allowed psychiatry to become a tool for social control.38,55,87,91 Let us not forget that psychiatry, like other fields of medicine, has been an integral part of the global economy since the beginning of the industrial revolution, and the introduction of new mental disorders with each new version of the DSM is beneficial to the pharmaceutical industry, the drug dispensing or conversion therapy industry, and other elements of the medical-industrial complex.5,77,91,94,95
ConclusionsIn this article, the current difficulties faced by psychiatric classification systems that aim to address and explain human behaviour have been explored from the perspective of sexual behaviours. A critical analysis of psychiatric nosology must transcend agreements or disagreements about the diagnostic criteria included in or removed from each new version. In fact, as we can see from an examination of diagnoses that include sexual behaviour criteria, it explores the very notion of health, mental health, mental disorder, normality and abnormality.
The ongoing process of pathologising human behaviours and presenting them as medical diagnoses is irrefutable proof of the medicalisation of everyday life. This process also involves even the most intimate aspects of human sexuality, and becomes a means of controlling the bodies and lives of individuals in order to make them conform to a hegemonic vision of health. The pathologisation of sexual behaviours in particular, and psychiatric nosology in general, is still highly controversial.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank the Human Behavioural Research Institute in Bogotá, and the Universidad del Magdalena, Santa Marta, Colombia, for their financial support for this review.
Please cite this article as: Campo-Arias A, Herazo E. Novedades, críticas y propuestas al DSM-5: el caso de las disfunciones sexuales, la disforia de género y los trastornos parafílicos. Rev Colomb Psiquiat. 2018;47:56–64.