To compare short versus long intramedullary nails for intertrochanteric hip fractures in terms of efficacy and safety.
MethodsWe included cohort studies and randomized clinical trials. The methodological quality of the studies was assessed by the Newcastle–Ottawa Scale. The meta-analysis was performed using the Review Manager 5.4. Heterogeneity was checked with the I2 test. A fixed effects model was adopted if there was no heterogeneity.
ResultsTwelve studies were included. The reoperations rate was lower in the short nail group (OR 0.58, 95% CI 0.38–0.88) and there were no differences regarding the peri-implant fracture rate (OR 1.77, 95% CI 0.68–4.60). Surgery time and blood loss was significantly higher in the long nail group (MD −12.44, 95% CI −14.60 to (−10.28)) (MD −19.36, 95% CI −27.24 to (−11.48)). There were no differences in functional outcomes.
ConclusionsThe long nail showed a higher reoperation rate, blood loss and surgery time compared to the short nail.
Comparar el clavo intramedular corto frente al clavo largo en las fracturas intertrocantéricas de cadera en términos de eficacia y de seguridad.
MétodosSe incluyeron estudios de cohortes y ensayos clínicos aleatorizados. La calidad metodológica de los estudios se evaluó mediante la escala Newcastle-Ottawa. El metaanálisis se realizó mediante el Review Manager 5.4. La heterogeneidad se comprobó con la prueba I2. Se adoptó un modelo de efectos fijos si no existía heterogeneidad.
ResultadosSe incluyeron doce estudios. La tasa de reoperaciones fue inferior en el grupo de clavo corto (OR: 0,58; IC 95%: 0,38-0,88) y no existieron diferencias en cuanto a la tasa de fractura peri-implante (OR: 1,77; IC 95%: 0,68-4,60). El tiempo de cirugía y la pérdida de sangre fueron significativamente mayores en el grupo de clavo largo (DM: −12,44; IC 95%: −14,60 a −10,28) (DM: −19,36; IC 95%: −27,24 a −11,48). No existieron diferencias respecto a los resultados funcionales.
ConclusionesEl clavo largo mostró una mayor tasa de reoperación, pérdida de sangre y tiempo quirúrgico en comparación con el clavo corto.
Due to the increase in life expectancy, hip fracture is a growing problem in the traumatology department.1 Intertrochanteric fracture is the most frequent.2 This fracture is associated with comorbidities such as osteoporosis and usually occurs in frail elderly patients, with a reported mortality up to 30% in the first year.3,4 This fact along with the loss of functionality of the elderly patients and the quality of life becomes one of the important health problems to be addressed.4,5 In addition, it is expected to increase with the consequent economic burden.6 The most widespread classification is the one proposed by AO/OTA, which divides into stable (31A1) or unstable (31A2 and 31A3).7
The use of intramedullary devices has increased, representing the first treatment option in intertrochanteric fractures. The biomechanical advantages over extramedullary devices have been demonstrated.8 Short nails are expected to increase stress on the tip of the implant causing refracture, especially in osteoporotic patients.9 This point is controversial, especially with the new generation short nails.10 On the other hand, shorter surgery and fluoroscopy time has been observed with short nails.10,11 In patients with unstable fractures, subtrochanteric extension or multifragmentary fractures, long nails are considered to be the best choice since they involve a larger surface area of the femur.12,13
Intertrochanteric fracture is one of the most common fractures in a trauma department. This meta-analysis aims to address a controversial topic, the comparison of the results obtained with short nail and long nail in intertrochanteric fracture. Therefore, the aim of this study was to conduct a meta-analysis of the surgical treatment of intertrochanteric fractures comparing in terms of safety and efficacy the short nail versus long nail.
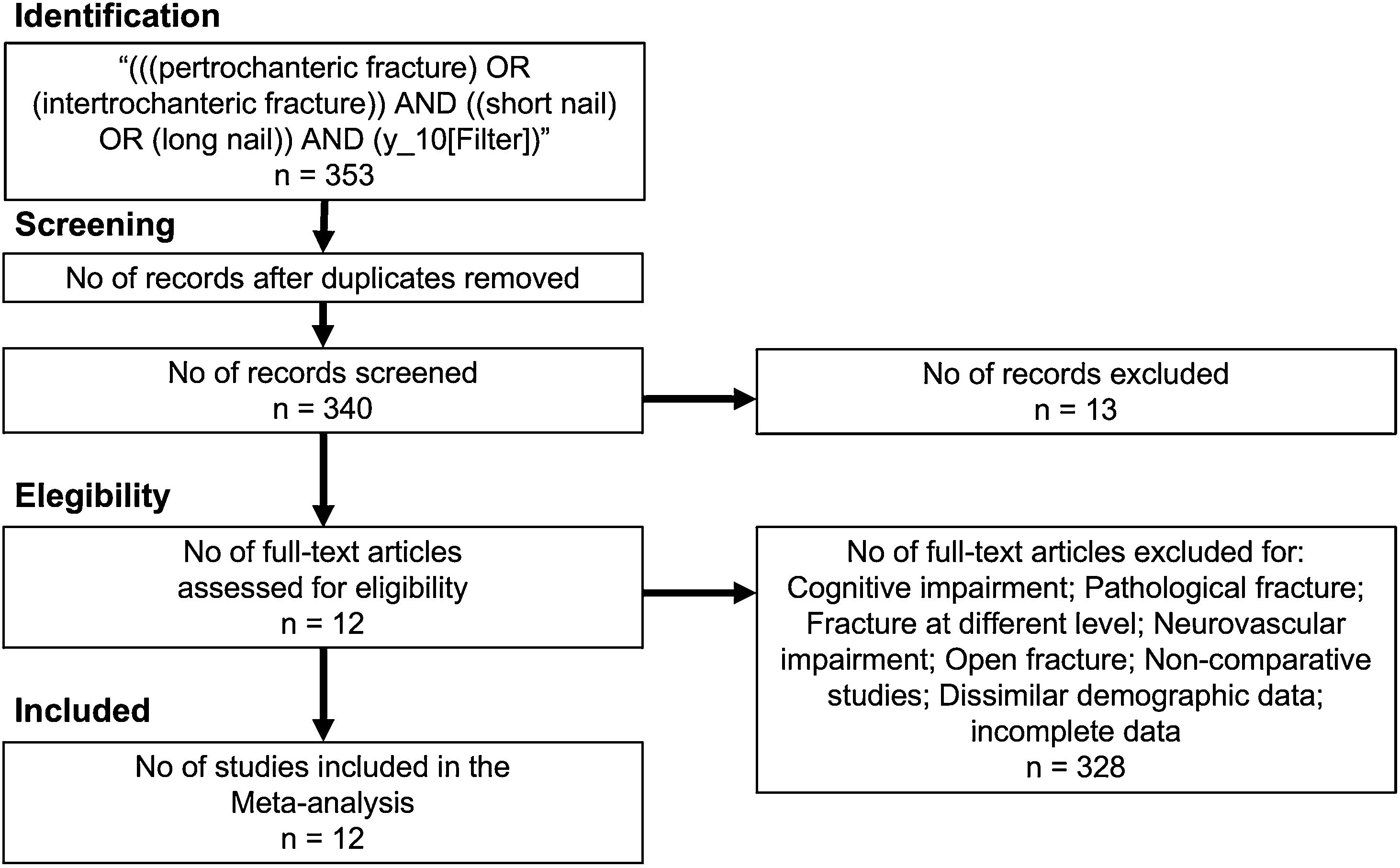
MethodsTypes of studiesThe current study followed PRISMA guidelines14 (Fig. 1). We followed the PICO strategy: (P) Patients with intertrochanteric hip fracture undergoing (I) short nail versus (C) long nail. (O) Outcomes were efficacy and adverse events. We included cohort retrospective/prospective studies and randomized clinical trials. Language was limited to English and we included patients older than 65 years old with intertrochanteric fracture. We excluded patients with cognitive impairment, pathologic fracture, coexistence of fracture at a different location, duplicated data, dissimilar demographis and incomplete data.
Types of outcome measuresThe baseline characteristics of each study article were obtained: number of participants, type of study, type of fracture according to the AO/OTA classification, manufacturer, follow-up and age. Measures of complications were analyzed: peri-implant fracture, reoperations, deep/superficial infection and mortality. Clinical variables consisted of blood loss (mL), length of stay (days), time of surgery (min) and number (n) of transfusions. Functional outcomes: number of patients who went from walking independently or with assistance to stop walking and number of patients who stopped walking independently.
Search methods for identification of studiesThe search strategy was the following: (((pertrochanteric fracture AND (y_10[Filter])) OR (intertrochanteric fracture)) AND ((short nail) OR (long nail)) AND (y_10[Filter]). Two authors independently reviewed the studies. An initial screening of titles and abstracts was performed to eliminate studies that were obviously outside the scope of the review. In cases of uncertainty based on title or abstract, the full text of each article was examined for further evaluation. All disagreements were resolved by discussion. A systematic search of the literature using PubMed, EMBASE, Scopus, and the Cochrane Collaboration Library database was carried out between 2011 and 2021.
Data collection and analysisThe meta-analysis was performed using the Review Manager 5.4 software package provided by the Cochrane Collaboration. For dichotomous variables, odds ratios with a confidence interval (CI) of 95% were calculated. The weighted mean difference (WMD) and the 95% CI were calculated for the continuous variables. Heterogeneity was checked with both the Chi2 and the I2 test. I2 varies from 0 to 100%, considering the values of 25, 50 and 75% as low, moderate, and high heterogeneity, respectively. A fixed effects model was adopted if there was no statistical evidence of heterogeneity, and a random effects model was adopted if significant heterogeneity was observed.
Additional analysesPublication bias was evaluated using the funnel plot diagrams. A sensitivity analysis was also carried out using Review Manager 5.4 software package eliminating the top-weight study from the comparisons in all the outcomes.
To assess the quality of the evidence and grade the strength of the recommendations, the Grade of Recommendation, Assessment, Development, and Evaluation (GRADE) system was used using GRADEpro for the critical variables. This system assesses study design, risk of bias, inconsistency, indirectness, imprecision, and summary of findings.
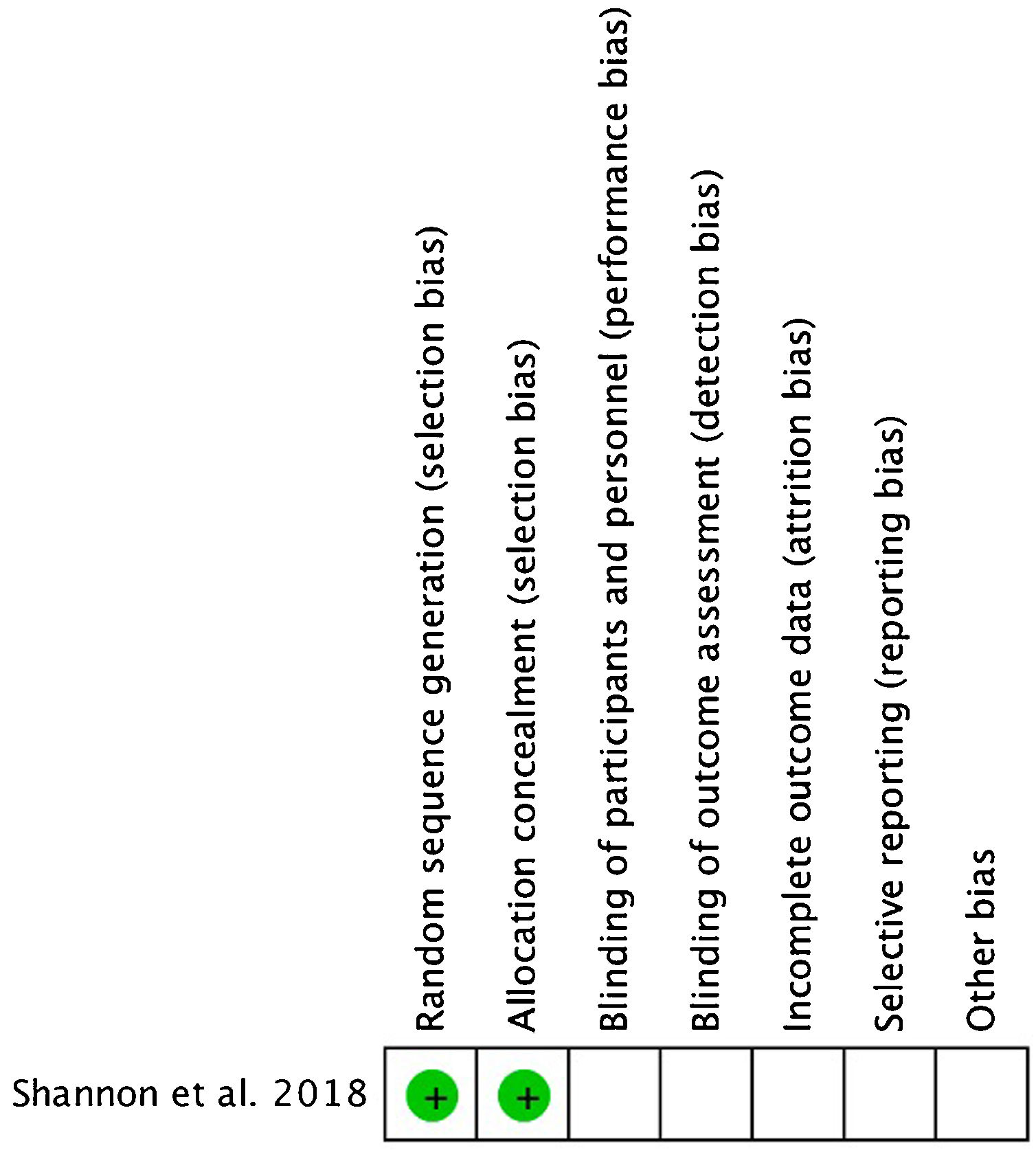
Assessment of risk of bias in included studiesThe methodological quality of the studies was independently assessed by two reviewers using the Newcastle–Ottawa Quality Assessment Scale for Cohort Studies15 (Table 1). The quality of the RCT20 was evaluated in accordance with Review Manager (RevMan) version 5.4 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, 2014) software to assess for the risk of bias.
Newcastle–Ottawa Quality Assessment Scale—cohort studies.
| Study | Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at start of study | Comparability of cohorts on the basis of the design or analysis controlled for confounders | Assessment of the outcome | Was follow-up long enough for outcomes to occur | Adequacy of follow-up of cohorts | Total |
|---|---|---|---|---|---|---|---|---|---|
| Luque-perez et al., 2020 [16] | * | * | * | * | ** | * | * | * | 9 |
| Frisch et al., 2017 [17] | * | * | * | * | * | * | * | * | 8 |
| Galanopoulus et al., 2018 [18] | * | * | * | * | * | * | * | * | 8 |
| Hong et al., 2020 [19] | * | * | * | * | ** | * | * | * | 9 |
| Shannon et al., 2018 [20] | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Raval et al., 2016 [21] | * | * | * | * | ** | * | – | * | 8 |
| Krigbaum et al., 2016 [22] | * | * | * | * | * | * | * | * | 8 |
| Viberg et al., 2021 [23] | * | * | * | * | ** | * | * | * | 9 |
| Guo et al., 2015 [24] | * | * | * | * | * | * | – | * | 7 |
| Li et al., 2015 [25] | * | * | * | * | * | * | – | * | 7 |
| Vaughn et al., 2015 [9] | * | * | * | * | ** | * | * | * | 9 |
| Lindvall et al., 2016 [26] | * | * | * | * | ** | * | – | * | 8 |
NA: not applicable.
The initial search found 353 results, from which duplicates were eliminated, resulting in a total of 340 articles. After reviewing the titles, abstracts and full texts 12 studies met the inclusion criteria and were included in the systematic review and meta-analysis (Fig. 1).
Description of studiesTable 2 shows the characteristics of the included studies. Twelve studies were included: one RCT, two prospective cohort studies and nine retrospective cohort studies. There was a pool of 4171 patients. Mean follow-up time ranged from 1 to 10 years. The age ranged from 70 to 83 years old.
Characteristics of the included studies.
| Study | n | Type of study | Fracture AO/OTA | Device | Manufacturer | Follow-up (years) | Mean age (SD) | ||
|---|---|---|---|---|---|---|---|---|---|
| Short nail | Long nail | ||||||||
| Luque-perez et al., 2020 [16] | 52 | 52 | Retrospective | 31A2 | Gamma3nail | Stryker | 2 | 82.3 (8.1) | 79.7 (9.1) |
| Frisch et al., 2017 [17] | 72 | 97 | Retrospective | 31A2, 31A3 | InterTAN | – | 5 | 72.6 (12.3) | 76.3 (15.2) |
| Galanopoulus et al., 2018 [18] | 25 | 25 | Cohort prospective | 31A2, 31A3 | AffixusOrthofix vero/nail | ZimmerOrthofix | 4 | 81 | 79 |
| Hong et al., 2020 [19] | 44 | 20 | Retrospective | 31A1, 31A2 | PFNA | Synthes | 3 | 80.0 | 79.8 |
| Shannon et al., 2018 [20] | 80 | 88 | Randomized clinical trial | 31A1–31A3 | TFNAGammaAffixus | DepuyStrykerBiomet | 3 | – | – |
| Raval et al., 2016 [21] | 40 | 40 | Retrospective | 31A1–31A3 | PFNA | – | 1 | 77.1 (9.2) | 76.1 (8.7) |
| Krigbaum et al., 2016 [22] | 125 | 137 | Retrospective | 31A1–31A2 | – | – | 10 | – | – |
| Viberg et al., 2021 [23] | 1867 | 378 | Retrospective | 31A1–31A3 | – | – | 5 | – | – |
| Guo et al., 2015 [24] | 102 | 76 | Retrospective | 31A1–31A2 | Gamma3 | Stryker | 1 | 82.7 (9.5) | 78.9 (8.7) |
| Li et al., 2015 [25] | 97 | 59 | Retrospective | 31A1–31A3 | PFNA | Depuy | 1 | 76.8 (6.6) | 74.6 (8.2) |
| Vaughn et al., 2015 [9] | 69 | 196 | Retrospective | 31A1–31A3 | Gamma3 | Stryker | 5 | – | – |
| Lindvall et al., 2016 [26] | 105 | 334 | Cohort prospective | 31A1–31A3 | – | DepuySmith-NephewStryker | 1 | 71.9 | 73.0 |
–: not applicable.
The Newcastle–Ottawa Quality Assessment Scale for Cohort Studies examines participant selection and study design, comparability of groups, and exposure/outcome ascertainment. Based on their score, studies were classified as low quality (0–3 points), moderate quality (4–6), or high quality (7–9) (Table 1). The quality of the RCT20 was evaluated in accordance with Review Manager. The evaluation methods consisted of the following steps: random sequence generation, allocation concealment, blinding, incomplete outcome data, and selective outcome reporting (Fig. 2).
Types of interventionsGroups were short intramedullary nail versus long intramedullary nail. Different types of nails from different manufacturers were included (Table 2). Due to the retrospective basis of the studies, no consideration was given to whether distal fixation was present and this decision in many cases was assessed by the surgeon intraoperatively. Surgery was performed in most cases by a specialist or a fellow surgeon. The surgical position was supine, guided by fluoroscopy.
Effects of interventionsThe reoperation rate was lower in the short nail group than in the long nail group (OR 0.58, 95% CI 0.38–0.88; participants=2595; studies=4; I2=0%) (Fig. 3). The rate of peri-implant fracture was higher in the short nail group (OR 1.77, 95% CI 0.68–4.60; participants=3356; studies=9; I2=42%) but there were not significant differences (Fig. 3). There were no differences in mortality rate or deep/superficial infection (OR 0.91, 95% CI 0.74–1.12; participants=2651; studies=4; I2=0%), (OR 0.74, 95% CI 0.34–1.61; participants=3170; studies=6; I2=0%) (Table 3).
Other outcomes: mortality, infection, and functional outcomes.
| Short nail compared with long nail for intertrochanteric fracture | |
|---|---|
| Outcomes | OR (95% CI) |
| Mortality | (OR 0.91, 95% CI 0.74–1.12; participants=2651; studies=4; I2=0%) |
| Infection | (OR 0.74, 95% CI 0.34–1.61; participants=3170; studies=6; I2=0%) |
| Go non-walk | (OR 0.91, 95% CI 0.38–2.17; participants=168; studies=2; I2=0%) |
| Stop walk indep. | (OR 1.80, 95% CI 0.86–3.79; participants=168; studies=2; I2=75%) |
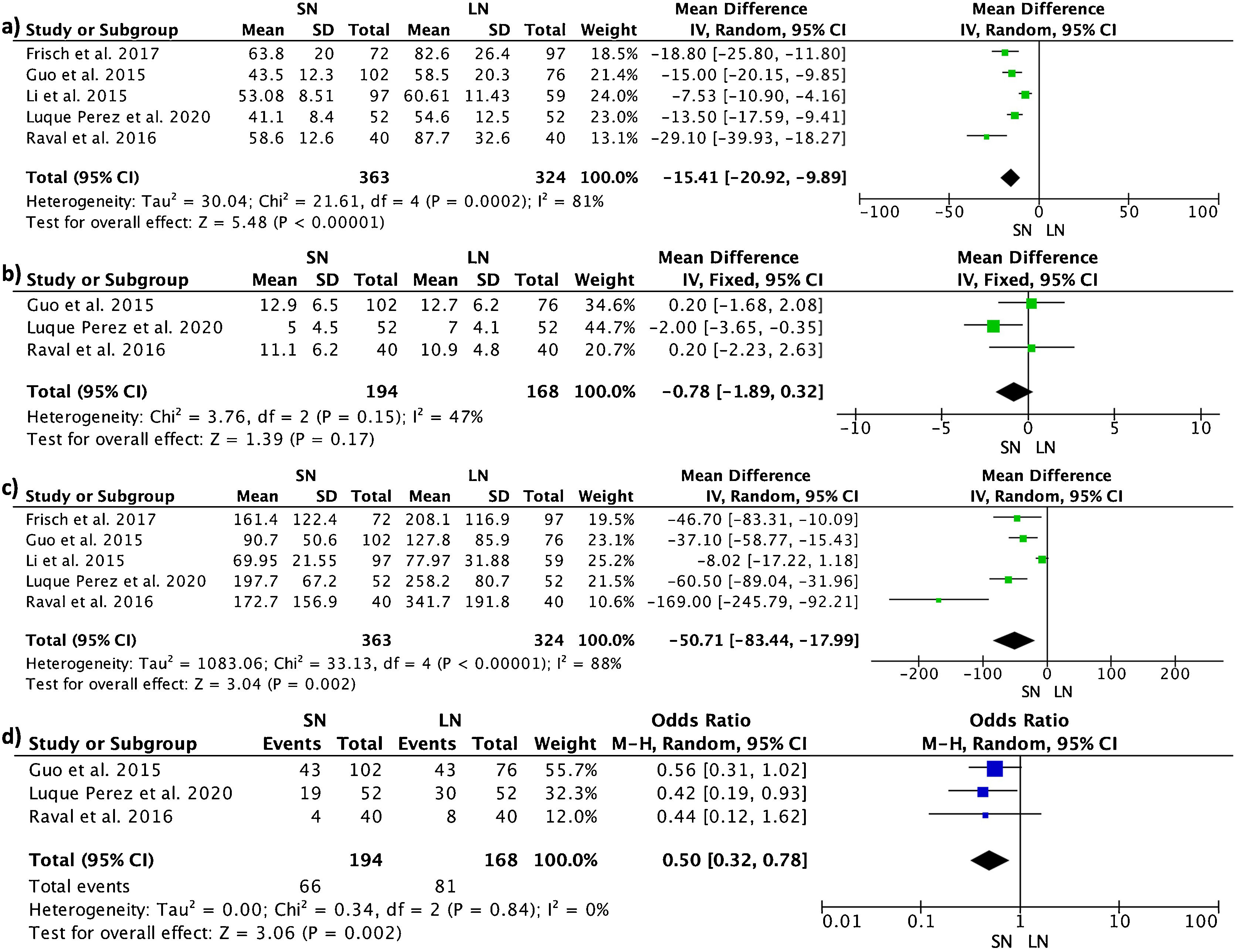
The surgery time was significantly longer in the long nail group (MD −15.41, 95% CI −20.92 to −9.89; participants=687; studies=5; I2=81%), as well as blood loss and number of transfusions (MD −50.71, 95% CI −83.44 to −17.99; participants=687; studies=5; I2=88%) and (OR 0.50, 95% CI 0.32–0.78; participants=362; studies=3; I2=0%). There was no difference in the hospital length of stay (MD −0.78, 95% CI −1.89 to 0.32) (Fig. 4).
There were no significant differences in the number of patients who stopped walking (independent or with assistance) and the number of patients who stopped being independent between the two groups (OR 0.91, 95% CI 0.38–2.17; participants=168; studies=2; I2=0%) (OR 1.80, 95% CI 0.86–3.79) (Table 3).
Sensitivity analysisAfter eliminating the top-weight study from the comparisons in all the outcomes, one of the variables became statistically significant. This outcome was the reoperation rate (Fig. 5).
GRADEThe GRADE (Grading of Recommendations, Assessment, Development and Evaluation) summary of the results of these three comparisons is shown in Table 4. There was moderate certainty for the reoperation variable and low certainty for the peri-implant fracture and mortality.
GRADE assessment of the quality of the evidence and the strength of the recommendations.
| Certainty assessment | № of patients | Effect | Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| № of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Complications | Placebo | Relative (95% CI) | Absolute (95% CI) | ||
| Reoperations | ||||||||||||
| 4 | Observational studies | Not serious | Not serious | Not serious | Not serious | All plausible residual confounding would reduce the demonstrated effect | 82/2037 (4.0%) | 39/558 (7.0%) | OR 0.58 (0.38–0.88) | 28 fewer per 1000 (from 42 fewer to 8 fewer) | Moderate | CRITICAL |
| Peri-implant fracture | ||||||||||||
| 9 | Observational studies | Not serious | Not serious | Not serious | Not serious | None | 31/2403 (1.3%) | 15/953 (1.6%) | OR 1.77 (0.68–4.60) | 12 more per 1000 (from 5 fewer to 53 more) | Low | CRITICAL |
| Mortality | ||||||||||||
| 4 | Observational studies | Not serious | Not serious | Not serious | Not serious | None | 646/2076 (31.1%) | 179/575 (31.1%) | OR 0.91 (0.74–1.12) | 20 fewer per 1000 (from 61 fewer to 25 more) | Low | CRITICAL |
CI: confidence interval; OR: odds ratio.
This meta-analysis compares short nail with long nail for the treatment of intertrochanteric fractures following the AO/OTA 31A1–31A3 classification. It has been observed that the long nail increases surgery time and blood loss during surgery which translates into an increase in the transfusion rate, and a higher rate of reoperation. However, there were no differences in functional outcomes. The results must be taken with caution because the nature of most of the studies was retrospective.
The quality of the evidence was low since most of the included studies were retrospective studies with level III evidence. Nor was it possible to carry out a blinding process for obvious reasons in both surgeons and patients. Relevant data such as mortality and patient functionality in terms of walking, walking with assistance or loss of independence were missing in several studies. In addition, the follow-up in a few studies was low to observe specific adverse events such as peri-implant fracture or infection.
The definitions of deep/superficial infection were different in different studies. This study focused on intertrochanteric fracture according to the AO/OTA type 31A1–31A3 classification.
This study differs from previous studies found to date, where no difference in the reoperation rate was found.10,27 This may be related to the fact that this meta-analysis included a lower number of studies and additional studies were required to increase the sample size and, therefore, to improve accuracy. The higher reoperation rate could be related to the tendency to treat stable fractures with short nails and unstable fractures with long nails. Regarding the peri-implant fracture rate, the long nail showed a lower risk of peri-implant fracture than the short nail without significant differences. This fact is described in the literature and may be explained by the fact that the short nail supports greater stress on the tip of the implant and the long nail involves greater surface area of the femur.28 Also, with the new short nails a lower rate of peri-implant fracture is expected and in some reports there is no difference compared with long nail.29 Nevertheless, there were no significant differences regarding peri-implant fracture.
The mortality rate is an essential outcome as it is conditioned by different factors such as comorbidity, blood loss or number of transfusions. This is particularly critical in elderly patients with multiple comorbidities.30 The studies stratified the results in terms of comorbidities, surgical risk and functionality, with no significant differences.31–33
In terms of functional outcomes, only two studies could be compared. We believe that this point should be included in future works, using the same functionality variable in order to compare more than two studies. There were no significant differences.
The clinical and surgical variables such as blood loss and number of transfusions were higher with long nail. Surgery time was shorter with the short nail; this could lead to improved patient security and operating room efficiency.9,25 Finally, no differences were observed in hospital length of stay. This point was related to costs. The costs could not be analyzed since there were only two articles that included this outcome and one of them did not provide sufficient data to be included in the statistical program.26
Some of the limitations of the included studies were different definitions for some of the variables such as infection, most of the studies were retrospective. No further exploration of statistical heterogeneity with subgroup analysis has been attempted since there were no studies that analyzed only stable fractures, thus limiting our confidence in the validity of the study results. It was also not possible to identify subgroups. As well as the use of different sizes and devices by the different manufacturers.
ConclusionsIn conclusion, the long nail did not present a lower peri-implant fracture; however, the reoperation rate is higher compared to the short nail, however, sensitivity and certainty of this outcome should be considered when interpretation of the data is performed. Blood loss and surgery time was higher in the long nail group. There were no differences in functional outcomes, although, few studies included these outcomes.
Level of evidenceLevel of evidence iii.
Ethics approval and consent to participateThis is a meta-analysis and therefore no ethics committee is required.
Informed consentThis is a meta-analysis, therefore, it does not require an informed consent.
FundingThe authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interestThe author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Nil to report.
Premio Fundación SECOT.