To evaluate the effectiveness and safety of the arthroscopic Bankart repair technique using a single anterior portal in patients with anterior shoulder instability.
Patients and methodsProspective study of 82 patients who underwent arthroscopic Bankart repair using a single anterior portal. Comparison with a historical series of 69 patients treated with two anterior portals. The patients were evaluated by the Rowe scale, and DASH (Disability of the arm, shoulder and hand) and OIS (Oxford Instability Shoulder) questionnaires, range of motion and visual analogue scales for pain and patient satisfaction.
ResultsAfter a mean follow-up of 36 months, there were no significant differences between groups regarding clinical or functional scores, quality of life or patient satisfaction. Surgical time was significantly shorter in the 1-portal group. In group 1-portal there were 2 patients with neurapraxias and 2 re-dislocations, while in group 2-portals were 1 and 2, respectively. The worst functional results were associated with the presence of a type III SLAP lesion.
ConclusionsBoth techniques were satisfactory regarding functional outcomes and complications, except for type-III SLAP lesions. Using only one anterior portal, the surgical time was shorter, and the costs were lower when dispensing with a second cannula and a suture passing instrument.
RESUMEN
Objetivoevaluar la efectividad y seguridad de la técnica artroscópica de Bankart utilizando un solo portal anterior en pacientes con inestabilidad anterior de hombro.
Pacientes y métodosestudio prospectivo de 82 pacientes operados con técnica de Bankart artroscópica de hombro utilizando un solo portal anterior. Comparación con una serie histórica de 69 pacientes tratados con dos portales anteriores. Fueron evaluados mediante la escala de Rowe, y cuestionarios DASH (Disability of the arm, shoulder and hand) y OIS (Oxford Instability Shoulder), arcos de movilidad y escalas analógicas visuales para dolor y satisfacción.
ResultadosTras un seguimiento medio de 36 meses, no había diferencias significativas entre grupos respecto a las valoraciones funcionales, calidad de vida o satisfacción del paciente. El tiempo quirúrgico fue significativamente menor en el grupo de 1-portal. En el grupo 1-portal hubo 2 pacientes con neuroapraxia y 2 re-luxaciones, mientras en el grupo 2-portales fueron 1 y 2, respectivamente. Los peores resultados funcionales se asociaban a la presencia de lesión SLAP tipo-III.
Conclusionesambas técnicas fueron satisfactorias respecto a los resultados funcionales y complicaciones, excepto en la presencia de lesiones SLAP tipo-III. Con la técnica de un portal anterior el tiempo quirúrgico fue más corto, y los costes menores al prescindir de una segunda cánula y de un pasador de hilos.
Traumatic anterior shoulder instability is a condition that is increasingly prevalent in young and active patients, associated most frequently with sport and high levels of activity.1 Many of these patients have a history of chronic instability, with failures of conservative treatment and multiple episodes of recurrent dislocation, resulting in serious deterioration of function. Arthroscopic repair using the Bankart technique has been demonstrated as effective for this condition.2
Numerous portals for arthroscopic shoulder surgery are currently described, and there is debate as to which is optimal.3,4 Most authors use 3 portals as standard for the Bankart technique, one posterior view portal combined with 2 anterior working portals.5 According to traditional studies, the 2 anterior portals are necessary to facilitate capsular repair on the anterior glenoid edge, to assess the anatomy of the anterior glenoid edge in case of bone defects, to better control detachment of the capsulolabral remains up to the point of visualising the muscle fibres of the subscapularis, and to be able to repair associated lesions such as that of the SLAP (superior labrum anterior posterior).6,7 However, the area of the safety triangle is sometimes small and can make it difficult to manipulate 2 anterior cannulas.8 Matsui y Omachi9 described a simplified Bankart repair technique using a single anterior portal. With the use of this technique, other authors8,10 have obtained satisfactory functional outcomes, and consider the shorter surgical time, the reduction in postoperative pain and reduction of costs as advantages.
The hypothesis of this study was that, in patients without previous bone defect, using a single portal would enable easier and faster arthroscopic repair of shoulder instability, achieving functional outcomes comparable to those of the traditional technique of 2 anterior portals.
The aim of this study was to assess the effectiveness and safety of the Bankart arthroscopic technique using a single anterior portal in patients with anterior shoulder instability.
Material and methodsA prospective study was undertaken of consecutive patients with recurrent traumatic anterior shoulder instability treated surgically between 2009 and 2014 by arthroscopic Bankart using a single anterior portal. The study was approved by the hospital’s Clinical Research Ethics Committee (CREC) and required informed consent. The inclusion criteria were at least 2 episodes of dislocation and mature skeleton. The exclusion criteria were posterior or multi-directional instability, rotator cuff tear or severe bone defect greater than 25% (Hill-Sachs or bone Bankart). The control group were patients consecutively treated with the Bankart technique for shoulder instability with 2 anterior portals between 2002 and 2007 identified from the department’s database, and with the same inclusion and exclusion criteria.
For all patients, preoperative diagnosis of instability was made by physical examination with positive apprehension and sulcus tests, and direction of instability established by examination under general anaesthetic. Radiological study and preoperative protocolised magnetic arthro-resonance studies were also performed.
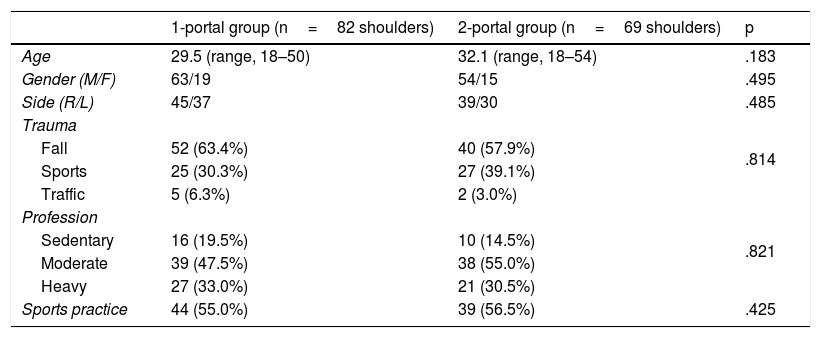
In the study group (1-portal group), the first 6 surgeries were not included because they were considered part of the learning curve. Thus, the following 81 patients were included, of which one was excluded from the study due to psychiatric illness and not having completed the minimum follow-up of 2 years. Therefore, 80 patients were studied, 2 with bilateral lesions (82 shoulders), whose baseline characteristics are shown in Table 1. The mean age was 29.5 (range, 18–50) years and 61 (76.5%) were men. There were 44 patients who practised sport prior to the surgery, 10 of whom professionally. The mean interval between the first dislocation and surgery was 2.7 (range, 1–15) years. There was an average of 7.0 episodes of dislocation (range, 2–20) and 53 (66.2%) patients had suffered at least 5 recurrences, of whom 26 (32.5%) had had up to 10 episodes, and 16 (20.0%) between 12 and 20 episodes. During surgery, SLAP-associated lesions were observed in 7 (8.7%) patients, 4 type II and 3 type III.
Patient characteristics.
| 1-portal group (n=82 shoulders) | 2-portal group (n=69 shoulders) | p | |
|---|---|---|---|
| Age | 29.5 (range, 18–50) | 32.1 (range, 18–54) | .183 |
| Gender (M/F) | 63/19 | 54/15 | .495 |
| Side (R/L) | 45/37 | 39/30 | .485 |
| Trauma | .814 | ||
| Fall | 52 (63.4%) | 40 (57.9%) | |
| Sports | 25 (30.3%) | 27 (39.1%) | |
| Traffic | 5 (6.3%) | 2 (3.0%) | |
| Profession | .821 | ||
| Sedentary | 16 (19.5%) | 10 (14.5%) | |
| Moderate | 39 (47.5%) | 38 (55.0%) | |
| Heavy | 27 (33.0%) | 21 (30.5%) | |
| Sports practice | 44 (55.0%) | 39 (56.5%) | .425 |
R: right; M: male; L: left; F: female.
There were 68 patients included in the control group (2-portals group), one of whom had had bilateral surgery (69 shoulders), these patients’ characteristics are shown in Table 1. During surgery, SLAP-associated lesions were observed in 4 (5.8%) patients, 2 type II and 2 type III. There were no significant differences between the two groups with respect to the baseline characteristics (Table 1).
Surgical protocolAll the patients in both groups were operated by the same surgeon, under ultrasound-guided locoregional interscalene block anaesthesia combined with general anaesthesia. First, the shoulder was explored under anaesthetic to check the direction of the instability. The operation was performed in the lateral decubitus position with a 2.3kg traction system. The arthroscopic Bankart technique was used in all patients.
A standard technique was used in the 2-portals group. First, the posterior view portal was created at about 2cm inferior and 1cm medial to the posterolateral edge of the acromion, checking the glenohumeral joint. The anterior portal, lateral to the coracoid process, was made with an out-in technique using a spinal needle as close as possible to the upper edge of the subscapular tendon, placing a cannula 8.5mm in diameter. The anterosuperior portal was performed with an out-in technique, close to the long portion of the biceps and using a 6.5mm cannula. This portal was used to view the anterior slope of the glenoid and assess the detachment of the anterior capsulolabral structures until the muscle mass of the subscapularis muscle was seen. With the optics in the posterior portal, the anchor was implanted from the anterior portal and the wires were retrieved through the anterosuperior portal. The anchors were placed from inferior to superior, starting at 5 o’clock and ending at 1 o’clock. The XCEL RC (Stryker) anchor system was used, a 3.5mm biodegradable implant with high strength Force Fiber #2. Then, through the anterior portal the capsulolabral structure was crossed with nitinol guidewires that were retrieved through the anterosuperior portal by means of retrieval forceps. A suture end was threaded into the nitinol and from the anterior portal the other end of the nitinol was pulled so that the threaded suture would pass through the capsulolabral structure to be repaired. The other suture line was retrieved through the anterior portal, and the suture knot was made. The average number of anchors in this group was 2.8. In all cases a capsular plication was made, especially at the lowest point as we did not place an anchor at 6 o’clock.
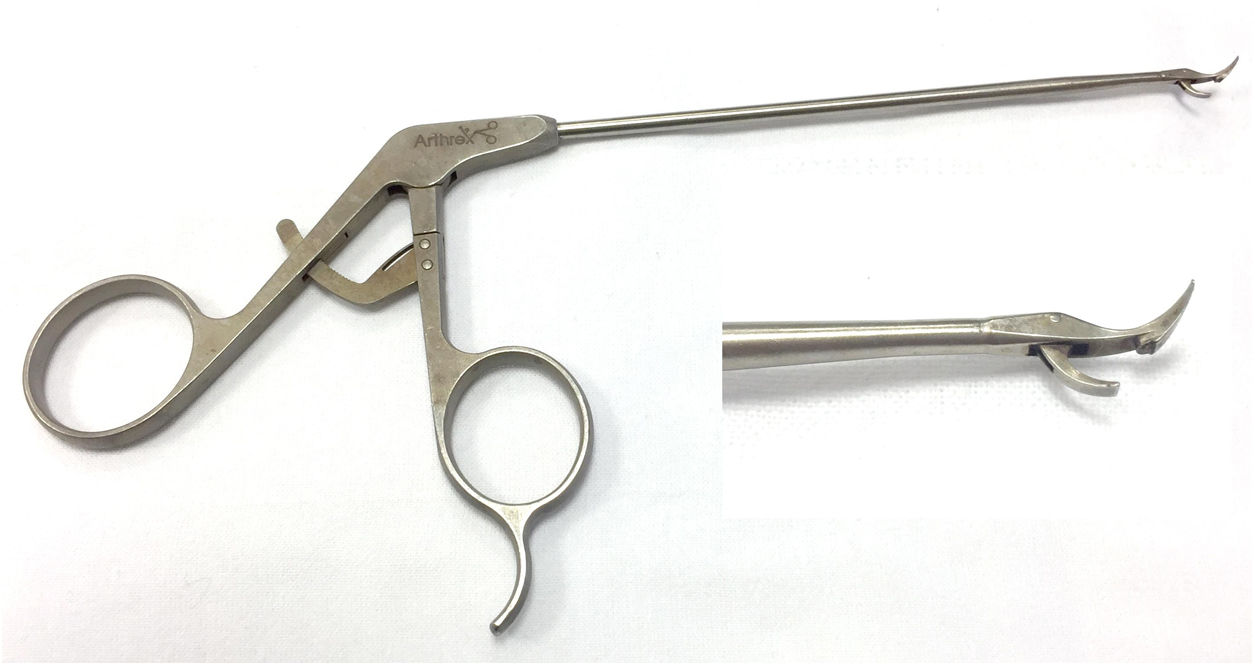
In the 1-portal group, the same posterior view portal was used. From this portal, a systematic check of the glenohumeral joint was made, including the anterior portion of the labrum, the inferior axillary recess, the posterior part of the humeral head to rule out Hill-Sachs injury, and the insertion of the supraspinatus tendon into the trochiter. The tendon of the brachial biceps was also visualised, verifying that it was not dislocated. The anterior portal was made in a similar way to the 2-portals group, except in the case of very bulky shoulders where the structures were not so easily located, in which it was made inside-out so that it was located as close as possible to the upper part of the subscapularis tendon. We placed a cannula of 8.5mm in this portal. Through this cannula we carried out disinsertion of all the debris of the capsule and labrum in the anterior part, and freshening of the anterior bone face of the glenoid using a curet. In this 1-portal group the Arthrex SutureTak® was used with a biodegradable impacted implant of 3mm and high strength wire, Fiberware #1. A mean of 2.9 anchors were used in this group. After placing the anchor on the bony edge of the glena, using a direct suture passer (StabiliHook, Arthrex, Stryker) (Fig. 1) the capsulolabral part was crossed through to the bony edge of the glena. By means of this suture passer, and the pinch-tuck technique, the wire end closest to the soft tissues was extracted. After that a Duncan or hanging type sliding knot was made, as in the 2-portals group.
Follow-up and assessmentIn a protocolised manner, all the patients in both groups underwent preoperative clinical assessment and postoperative assessment at one, 3, 6, 12 and at least 24 months. In the 2-portals group, the clinical, surgical and follow-up documentation was reviewed. Specific assessments of the shoulder were computerised on a database.
The Rowe scale11 was used for functional assessment, also categorised as excellent (90–100 points), good (75–89), fair (51–74) and poor (≤50). Shoulder mobility was measured using a standard goniometer, with the patient in the supine position for flexion, extension and abduction, and in the prone position for rotations. Overall quality of life was assessed with the DASH12 (Disability of the Arm, Shoulder and Hand) questionnaire transformed to a scale of 0–100, where 100 was maximum disability, and specific quality of life for disability in shoulder instability was assessed using the OISS13(Oxford Instability Shoulder score), with scores between 12 for excellent outcome and no difficulty, and 60 for poor outcome with maximum difficulty. Pain and patient satisfaction were assessed using visual analogue scales (VAS), where 0 was poor and 10 excellent. The surgical time was from the beginning of the operation until its completion, excluding the anaesthetic time.
Radiologically, standard anteroposterior, transcapular and axillary projections were performed, together with systematic preoperative magnetic arthroresonance imaging.
X-rays were taken immediately postoperatively. In the absence of complications, no other imaging controls were undertaken.
Statistical analysisA statistical power analysis was performed; calculating the effect size with respect to the postoperative differences of the Rowe scale11 for an alpha of 0.05, an effect size of d=1.81 and a statistical power of 0.84 were obtained, which was appropriate for biomedical studies.
IBM-SPSS v 19.0. was used to analyse the data. The normality of the variables was tested using the Kolmogorov–Smirnov test. Between the groups, the categorical variables were compared with the chi-squared or nonparametric Mantel–Haenszel test, and the continuous variables with the Student’s t or Mann–Whitney test, or analysis of variances if there were more than 2 subgroups. Pre- and postoperative comparison of categorical variables was performed with the McNemar test, and continuous variables with the paired Student’s t-test or the nonparametric Wilcoxon signed rank test. The safety and effectiveness of the surgery was assessed by Kaplan–Meier survival analysis, considering the presence of a complication of any cause or an unsatisfactory outcome the end point. The log-rank test was used to compare survival curves between groups. A p value of less than 0.05 was considered significant in all the tests.
ResultsThe mean postoperative follow-up in the 1-portal group was 36.4 months (range, 24–49) and 26 months (range, 24–29) in the control group. The mean surgery time was 31min (range, 20–41) in the 1-portal group and 42min (range, 31–61) in the 2-portals group, the difference being significant (p=.001).
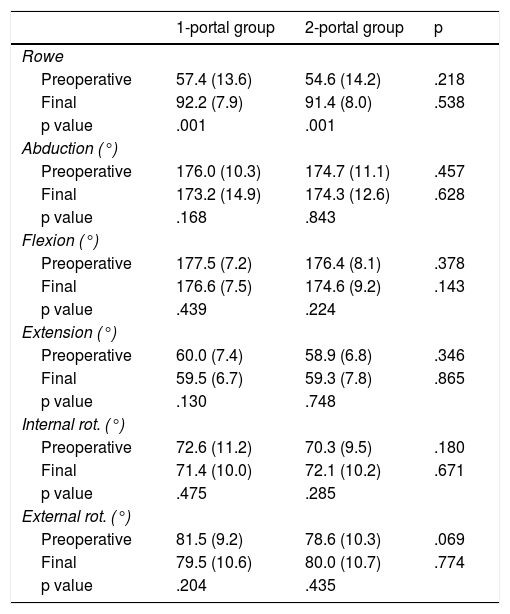
From the preoperative assessment to the final assessment, the Rowe scale improved significantly in both groups, but there was no significant variation in range of motion (Table 2). Comparing both groups, at the end of follow-up (Table 2) there were no significant differences in the Rowe scale or ranges of motion.
Pre- and postoperative objective data of both groups.
| 1-portal group | 2-portal group | p | |
|---|---|---|---|
| Rowe | |||
| Preoperative | 57.4 (13.6) | 54.6 (14.2) | .218 |
| Final | 92.2 (7.9) | 91.4 (8.0) | .538 |
| p value | .001 | .001 | |
| Abduction (°) | |||
| Preoperative | 176.0 (10.3) | 174.7 (11.1) | .457 |
| Final | 173.2 (14.9) | 174.3 (12.6) | .628 |
| p value | .168 | .843 | |
| Flexion (°) | |||
| Preoperative | 177.5 (7.2) | 176.4 (8.1) | .378 |
| Final | 176.6 (7.5) | 174.6 (9.2) | .143 |
| p value | .439 | .224 | |
| Extension (°) | |||
| Preoperative | 60.0 (7.4) | 58.9 (6.8) | .346 |
| Final | 59.5 (6.7) | 59.3 (7.8) | .865 |
| p value | .130 | .748 | |
| Internal rot. (°) | |||
| Preoperative | 72.6 (11.2) | 70.3 (9.5) | .180 |
| Final | 71.4 (10.0) | 72.1 (10.2) | .671 |
| p value | .475 | .285 | |
| External rot. (°) | |||
| Preoperative | 81.5 (9.2) | 78.6 (10.3) | .069 |
| Final | 79.5 (10.6) | 80.0 (10.7) | .774 |
| p value | .204 | .435 | |
Data expressed as means (standard deviation).
In the final assessment of the 1-portal group, in terms of Rowe score there were 67 (83.7%) patients with an excellent outcome, 9 (11.3%) patients with a good outcome and 4 (5.0%) with a fair outcome. Among the latter were the 3 patients with type III SLAP lesion. These 3 patients had no postoperative complications and the fair outcome was due to mobility, with abduction of 120° and rotations of 50°. The fourth patient, a 25-year-old woman with a moderate job, presented postoperative brachial plexus neuroapraxia, resulting in 90° abduction and 50° rotations.
In the 2-portals group there were 59 (85.5%) patients with excellent Rowe results, 8 (11.6%) patients with a good outcome and 2 (2.9%) patients with a fair outcome. Of those with a fair outcome, one patient had a type III SLAP lesion resulting in painful restriction of motion. The other patient, a 51-year-old male, had no complications resulting in reduced motion.
In both groups, all the patients reported no difficulty or loss of strength in their working or sports activities at one year following surgery, including the patients with a fair functional outcome. All the patients returned to their former work activity.
Of the 44 patients in the 1-portal group who practiced sport preoperatively, 38 (86.3%) practiced it again, while 6 (13.7%), all non-professionals, did not return to it. Of the 39 patients in the 2-portals group who practiced sport, 31 (79.5%) practiced it again, all were amateur.
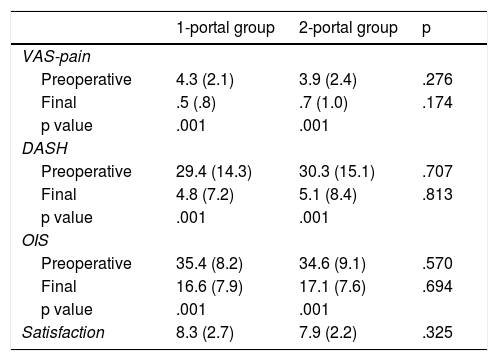
Pain and quality of life (Table 3) improved significantly from the preoperative assessment to the final assessment in both groups. At the end of follow-up there were no significant differences between the two groups.
Pre-and postoperative subjective data of both groups.
| 1-portal group | 2-portal group | p | |
|---|---|---|---|
| VAS-pain | |||
| Preoperative | 4.3 (2.1) | 3.9 (2.4) | .276 |
| Final | .5 (.8) | .7 (1.0) | .174 |
| p value | .001 | .001 | |
| DASH | |||
| Preoperative | 29.4 (14.3) | 30.3 (15.1) | .707 |
| Final | 4.8 (7.2) | 5.1 (8.4) | .813 |
| p value | .001 | .001 | |
| OIS | |||
| Preoperative | 35.4 (8.2) | 34.6 (9.1) | .570 |
| Final | 16.6 (7.9) | 17.1 (7.6) | .694 |
| p value | .001 | .001 | |
| Satisfaction | 8.3 (2.7) | 7.9 (2.2) | .325 |
Data expressed as means (standard deviation).
DASH: Disability of the Arm, Shoulder and Hand; VAS; visual analogue scale; OIS: Oxford Instability Shoulder.
In the 1-portal group the mean satisfaction with the operation was 8.3 (SD 2.7); all the patients reported a score above 7, except for the patient with brachial plexus neuroapraxia, who gave a score of 5. In the 2-portals group the mean satisfaction was 7.9 (SD 2.2), all of at least 7 points. There was no significant difference between the groups (p=.325).
ComplicationsIn the 1-portal group there were 2 (2.5%) patients with neuroapraxias, one of the brachial plexus (cited with a fair clinical outcome) and another of the axillary nerve that recovered at 3 months and resulted in a Rowe score of 100 points. Another 2 (2.5%) patients suffered a redislocation one year following surgery, both traumatic due to falls while skiing and playing football. Both were reoperated using the Bankart arthroscopic technique, and had no more dislocations in the follow-up time, resulting in a Rowe score of 90 and 95, respectively.
In the 2-portals group there was one case of axillary nerve neuroapraxia that recovered at 2 months and resulted in a Rowe score of 96 points. Another 2 (2.9%) patients suffered a redislocation, one spontaneous at 3 months, and the other due to trauma at 14 months. Both were reoperated with the Bankart arthroscopic technique, and there were no further disclocations in the follow-up time, resulting in a Rowe score of 92 and 90, respectively.
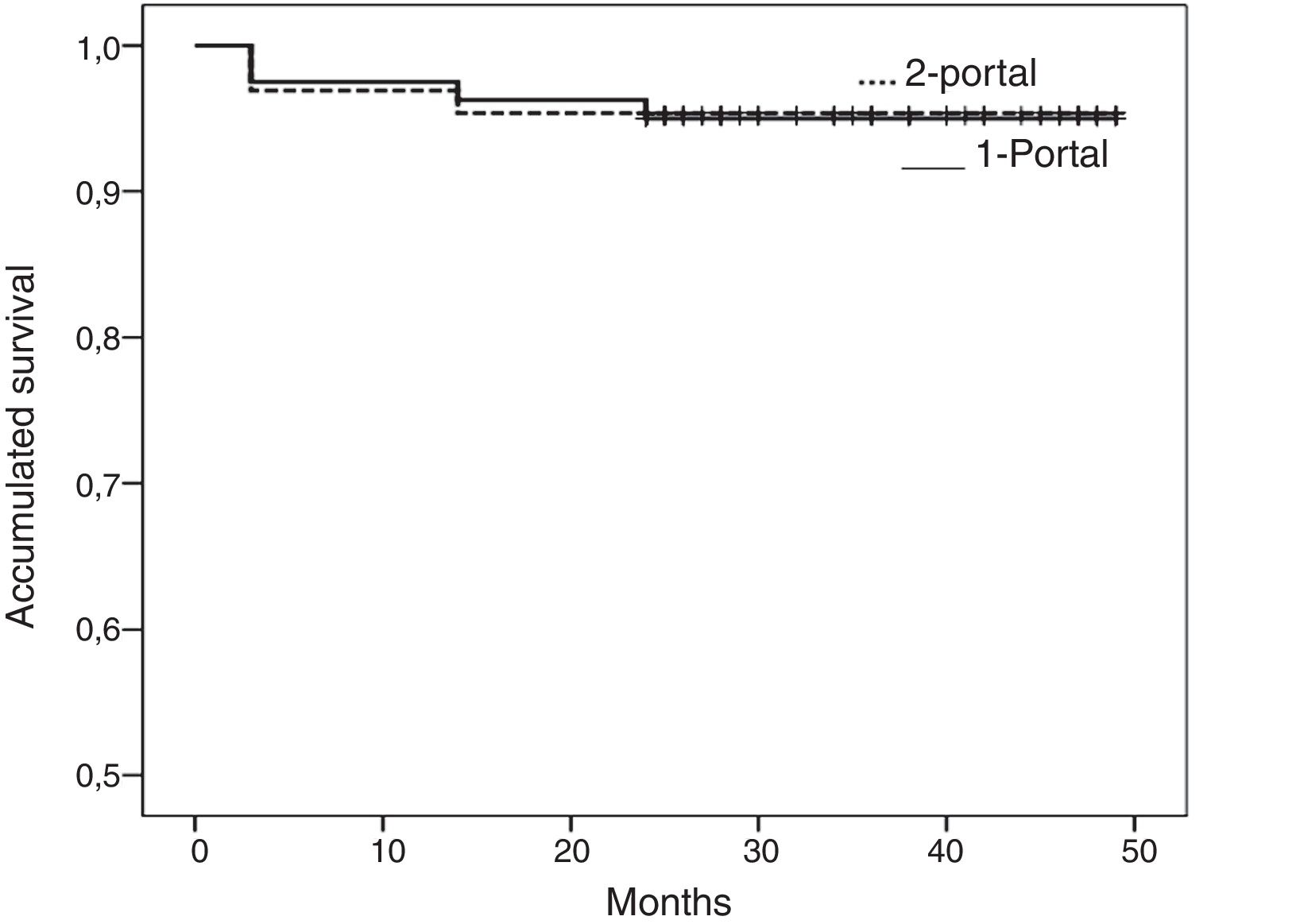
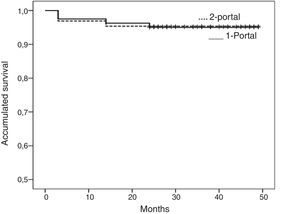
The safety of the technique at 45 months (Fig. 2), considering complications of any cause the end point (neuroapraxia or redislocation), was 95.0% (95% CI, 90.2%–99,8%) in the 1-portal group, and 95.4% (95%CI, 90.3%–100%) in the 2-portal group (p=.919).
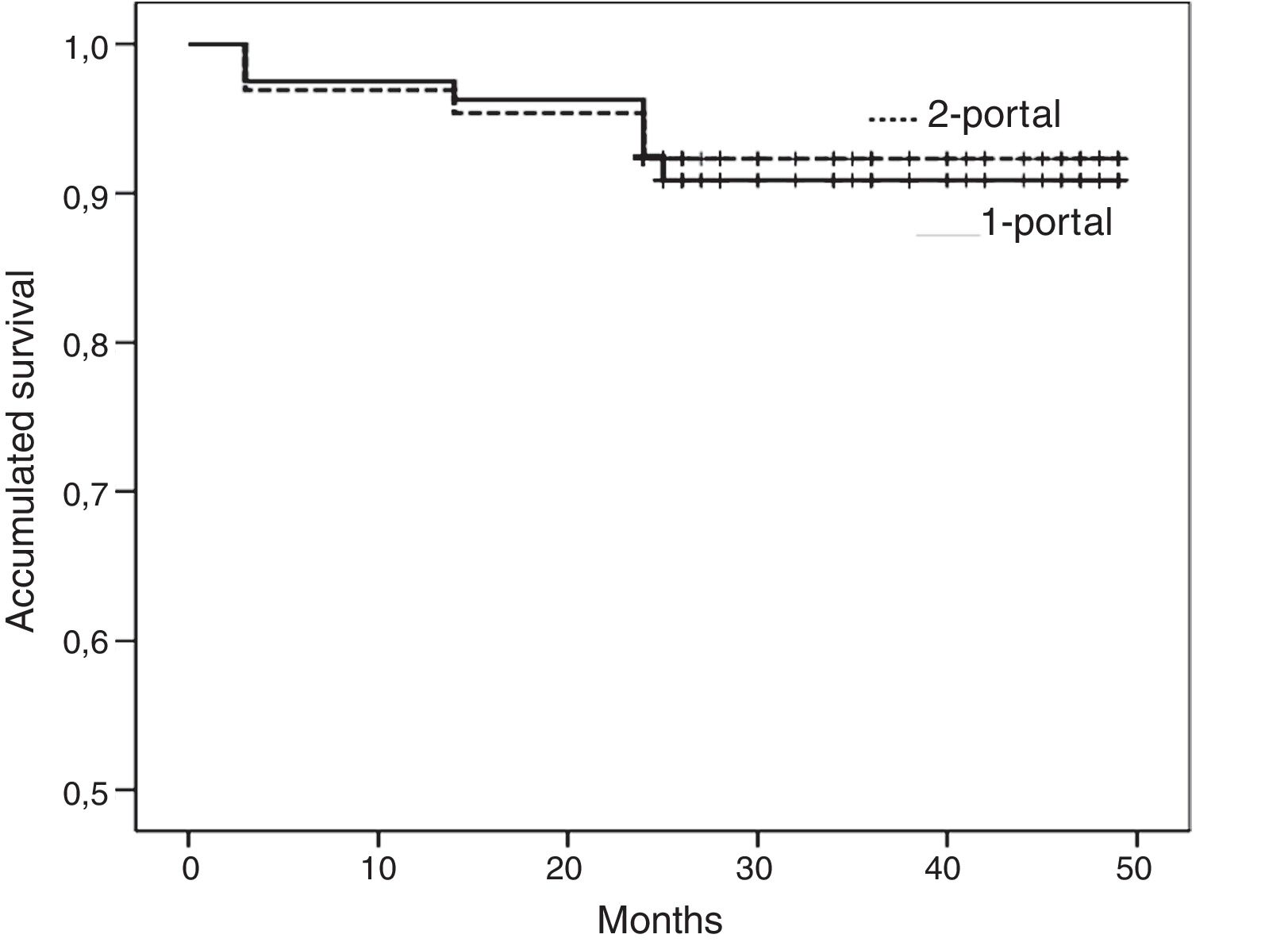
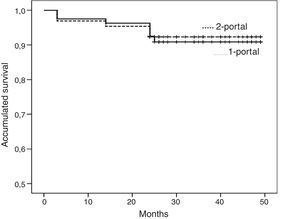
The effectiveness of the surgical technique at 45 months (Fig. 3), considering complications of any cause the end point (neuroapraxia or redislocation) and/or unsatisfactory result (fair or poor Rowe score) was 90.8% (95%CI, 84.3%–97.3%) in the 1-portal group, and 92.3% (95% CI, 85.8%–98.8%) in the 2-portal group (p=.834).
DiscussionThe Bankart arthroscopic technique using bone anchor sutures has been shown to be effective in treating anterior shoulder instability.2 For arthroscopic shoulder surgery, numerous portals have been described depending on the lesion to be repaired, although the most commonly used for the Bankart technique are a posterior portal combined with 2 anterior portals.5
Traditionally, the use of 2 anterior portals has been used to re-anchor the labrum, one for placement of the anchor with suture wire, and the other for retrieving the wires with a suture-passing instrument and knotting. However, in this study a direct passing instrument was used that enabled the suture to be made in the labrum and the sutures to be retrieved for knotting through the same portal. This led to simplification of the technique and faster execution of the surgery. In our opinion, only 2 studies have focussed on the use of a single anterior portal to perform an arthroscopic Bankart repair, both based on the difficulty that is occasionally encountered in placing 2 anterior cannulas.8,10 The 2 studies reported that surgery time was significantly shorter with the use of only one anterior portal.
Both techniques were shown to be equally effective in this study. However, the use of 2 anterior portals implies the use of 2 cannulas in the safety triangle, an area that is sometimes small and in which it is difficult to manipulate the cannulas.8
Although infrequent for experienced arthroscopists, some complications associated with the technique with 2 anterior portals have been described, such as injury to the cuff, the long portion of the biceps or the axillary nerve.14,15 On the other hand, this 2-portal technique has the advantage for less experienced surgeons of better visualisation of joint structures. In this study there were 2 patients in whom a small dilaceration of the long portion of the biceps occurred when creating and positioning the anterosuperior portal, but required no specific treatment.
With regard to the technique using only one anterior portal, we think it simplifies the technique for experienced surgeons with the direct passing instrument. In this study we found that the use of a single anterior portal was a reproducible technique, allowing adequate visualisation of the joint and safe surgical action. Likewise, it allowed the placement of at least 3 anchors and additional anchors in the case of a SLAP lesion. However, it might not be useful in the case of extensive labral lesions or excessively fragile labrum, especially for surgeons less accustomed to using direct passing instruments. In this study, there was one case where an excessively fragile capsule was torn when using this instrument and an attempt was made to make a plication at the lowest point. This made it necessary to reposition an anchor closer to 5 0’clock, and to perform less aggressive capsular retensioning.
The functional outcomes in the 1-portal group were in line with those usually described in the literature after the use of 2 anterior portals,16,17 as well as the rate of return to former activities including sports,18 quality of life and patient satisfaction with the surgery.19 Cicek et al.10 retrospectively compared 49 patients using a single anterior portal and 42 patients using a conventional double anterior portal. The functional outcomes, measured using the Constant and Rowe scales, and the range of motion were similar between the 2 groups. On the other hand, the outcomes of this study were not satisfactory for patients with type III SLAP lesions, regardless of the portals used. In the 2-portals group we thought that the poor outcome was due to a poor surgical indication in not resecting the bucket handle and preferring to make a suture. In those of the 1-portal group we thought that it was due to deficient rehabilitation, since they did not report pain but presented loss of shoulder mobility. While some authors,20 using a double anterior portal, found that this lesion made the intervention difficult and affected mobility of the shoulder; other authors21 found that a SLAP lesion did not affect functional outcomes.
In this study, the rate of redislocation was similar in both groups (2.5% versus 2.9%). Armangil et al.8 used a single anterior portal in 72 patients with a mean age of 24 years and anterior instability of the shoulder. Almost half the patients had Bankart and SLAP lesions. After a follow-up of 49 months, there were 4 redislocations (5.6%). Cicek et al.10 reported redislocations in 2 patients (4.1%) of the group treated with a single portal and one patient (2.4%) in the double anterior portal group. Recent studies,2,16 using 2 anterior portals, report a redislocation rate of 7%. In the study by Antunes et al.2 the rate of young patients was higher than in our study, the time between first dislocation and the arthroscopic repair was longer, and they included various aetiologies, traumatic and non-traumatic. According to some authors, the number of anchors and the presence of severe bone defects are predisposing factors for redislocation,22 and the number of dislocations prior to surgery.23 In this study the rate of redislocation was probably lower because patients with bone defects had been excluded, and there were no cases with multi-directional dislocation.
The limitations of this study are those of a non-randomised comparison, with possible bias in patient selection although there were no significant preoperative differences between the groups. In addition, the size of the groups was relatively small, but the statistical power was sufficient to discriminate differences. Randomised and further follow-up studies would be needed to confirm the results of the present study.
ConclusionBoth techniques were satisfactory with respect to functional outcomes and complications, except in the presence of type III SLAP lesions. With the technique of an anterior portal the surgical time was shorter, and the costs were lower through dispensing with a second cannula and a suture passing instrument.
Level of evidenceLevel of evidence II.
FinancingThis research study has received no specific grants from public sector agencies, the commercial sector or non-profit organisations.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Sebastiá-Forcada E, Martínez-Rico S, Vizcaya-Moreno MF, Lizaur-Utrilla A. Estudio prospectivo de efectividad y seguridad de Bankart artroscópico utilizando solo un portal anterior para pacientes con inestabilidad de hombro anterior. Rev Esp Cir Ortop Traumatol. 2019;63:431–438.