Blastomycosis is a subacute or chronic deep mycosis caused by a dimorphic fungus called Blastomyces dermatitidis, which generally produces a pulmonary form of the disease and, to a lesser extent, extra-pulmonary forms such as cutaneous, osteoarticular and genitourinary, among others. Cutaneous blastomycosis is the second clinical presentation in frequency. It is considered as primary when it begins by inoculation of the fungus due to traumas, and secondary when the lung fails to contain the infection.
Case-reportWe present the case of a 57 year-old male who had a 5 year-history of an irregularly shaped verrucous infiltrative plaque related to and insect bite and posterior trauma due to the manipulation of the lesion. B. dermatitidis was identified using direct examination, stains, isolation in culture media, histopathology, and molecular studies. An antifungal susceptibility test was performed using method M38-A2 (CLSI). Clinical and mycological cure was achieved with itraconazole.
ConclusionsThis cutaneous blastomycosis case acquired in the United States (Indianapolis) is rather interesting and looks quite similar to other mycoses such as coccidioidomycosis or sporotrichosis. The presented case shows one of the multiple issues concerning migration between neighboring countries.
La blastomicosis es una micosis profunda, subaguda o crónica, causada por el hongo dimorfo Blastomyces dermatitidis, que generalmente produce una enfermedad pulmonar y, en menor proporción, formas extrapulmonares (cutánea, osteoarticular y genitourinaria). La blastomicosis cutánea es la segunda forma clínica más observada; es de tipo primario cuando se presenta por la inoculación del hongo a través de traumatismos, y de tipo secundario cuando se disemina a partir de un foco pulmonar.
Caso clínicoSe presenta el caso de un varón de 57años con blastomicosis cutánea verrugosa de 5años de evolución, relacionada con la picadura de un insecto, que empeora con la manipulación de la lesión. El caso fue confirmado por la identificación de B.dermatitidis en exámenes directos, tinciones, aislamiento en medios de cultivo habituales, análisis histopatológico y estudios moleculares. Se realizó una prueba de sensibilidad antifúngica por el método M38-A2 (CLSI). La curación clínica y micológica se logró con itraconazol oral.
ConclusionesEste caso de blastomicosis cutánea adquirida en Estados Unidos (Indianápolis) es de gran interés y resulta similar a los de otras micosis, como la coccidioidomicosis y la esporotricosis. Este caso refleja uno de los múltiples factores relacionados con la migración entre países cercanos.
Blastomycosis is a chronic or subacute deep mycosis caused by a dimorphic fungus called Blastomyces dermatitidis, which generally produces pulmonary disease and, to a lesser extent, extra-pulmonary forms as cutaneous, osteoarticular and genitourinary profiles, among others.12,17,19,22 Blastomycosis is predominantly a mycosis of Canada and United States of America (USA); it is endemic in midwestern states of Canada, around the Great Lakes, and especially in southern and southeastern states of USA.2,19,21 In Mexico the disease has never been reported as autochthonous; there are only five cases reported, two of them related to immigration to the United States.9,13,18,20,23
Cutaneous blastomycosis is the most common extra-pulmonary form of the disease; it constitutes 40–80% of all the cases and can be classified as primary or secondary. Herein, we present a case of cutaneous blastomycosis in a Mexican immigrant, acquired at the USA endemic area.3,12,21
Clinical caseA 57 year-old male farmer presented with a 5 year-history of a 10cm×8cm verrucous plaque, covered with meliceric crusts and scales with a fistulae located in the right axillary region that apparently began after an insect bite and manipulation of the area. The patient referred that the skin lesion developed approximately 15 days after the initial injury (Fig. 1). He had a history of immigration through several states of the USA during 4 years, including Arizona, Wisconsin, Illinois, Ohio and Indianapolis. In the latter, he worked in the production and handling of organic compost as fertilizer.
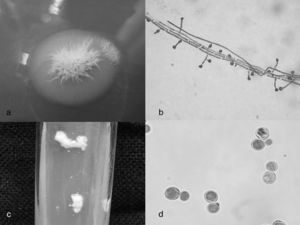
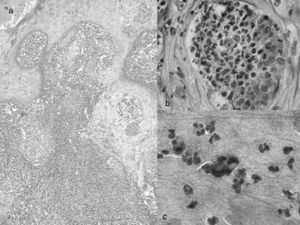
The patient did not seek for treatment until he returned to Mexico, where he was examined at the dermatology service, and the first clinical impression suggested a cutaneous coccidioidomycosis or cutaneous tuberculosis. Thorax X-ray was negative for pleuro-pulmonary and bone disease, and fistulography was also negative. Bronchoalveolar lavage, direct examination of the sputum, cultures and bacilloscopy searching for Mycobacteria were negative. Intradermal reactions for PPD, sporotrichin and coccidioidin were negative. Direct examination (KOH 10%), Giemsa and Papanicolaou stains showed mono-budding yeasts, and culture in Sabouraud dextrose agar (25 days, 28°C) developed a whitish-gray and slow growing colony, microscopically with abundant septated mycelia and multiple sessile pyriform conidia of 4–6μm, some of them emerging from short conidiophores (with ramifications, resembling “L” letter) (Fig. 2); thermal dimorphism was proved. Skin biopsy reported a tuberculoid granuloma, surrounding a few mono-budding yeasts with a thick and refractive wall (Fig. 3). The study by means of PCR of ITS1 and ITS4 regions, and the D1-D2 dominion rendered the Ajellomyces dermatitidis (teleomorph of B. dermatitidis) species identity. Antifungal susceptibility test of the isolated B. dermatitidis strain (1245-10), carried out with the method M38-A2 from the CLSI, yielded the following minimum inhibitory concentration (MIC) values: amphotericin B 0.125μg/ml (reference interval 1–2μg/ml); itraconazole 0.250μg/ml (ref. 0.06–0.5μg/ml); voriconazole 0.125μg/ml (ref. 0.015–0.125μg/ml) and posaconazole 0.125μg/ml (ref. 0.06–0.25μg/ml).10 Reference intervals are the MIC ranges for Paecilomyces variotii ATCC MYA-3630 reference strain. Based on the susceptibility test results and according to the cost-benefit balance, itraconazole 200mg/day was prescribed, and prednisone 0.5mg/kg/day was administered only for 30 days (in order to prevent fibrosis). Later on itraconazole was increased to 300mg/day for 3 months, and a reduction scheme was installed afterwards. The total time of therapy was 8 months. The patient achieved clinical and mycological cure. After two years of follow up there is no evidence of disease activity (Fig. 1).
(a) Blastomyces dermatitidis, filamentous culture in Sabouraud dextrose agar 28°C, 25 days; (b) Sessile microconidia and microconidia emerging from short conidiophores (“lollipop-like”); (c) B. dermatitidis, yeast culture in Sabouraud dextrose agar, 37°C, 5 days; (d) yeasts with thick base.
Blastomycosis, also called Gilchrist's disease or Chicago's disease, is a typical deep or systemic mycosis that primarily affects the lung. However, secondary extrapulmonary involvement can be seen, being the cutaneous cases the most common ones.17,19
It is difficult to establish if the case presented here constitutes a primary or a secondary cutaneous case. We considered it as primary cutaneous blastomycosis because of the patient history of trauma in the axillary region when working at Indianapolis (fertilizer), which is the suspected place where the disease began, and due to the lack of pulmonary involvement. However, the chronicity of the process makes it doubtful.
There are only few primary cutaneous cases of blastomycosis reported in the literature, although they may be underestimated due to the possibility of its spontaneous cure, something that happens in the sporotrichosis.4,11,12 Cases usually begin with fungal inoculation into the skin due to a traumatism. After an incubation period of 2–3 weeks, a chancre accompanied with lymphangitis and lymphadenitis develops. The principal clinical manifestation is a verrucous, nodular or papular lesion; only few patients show ulcers or pustular lesions. 3,6–8,16,18,19 In our case, the patient mentioned a previous insect bite and manipulation in the site where the lesion developed, so that could be the entrance pathway. Despite its long history, the lesion had a slow progression, approximately 10cm2 in 5 years. The initial diagnosis was coccidioidomycosis because the majority of Mexican immigrants cross the USA border through the desert areas of the borderline (California, Arizona).3 Nonetheless, the patient lived for long periods of time in endemic areas of blastomycosis. This case constitutes an example of those imported diseases as a result of migration, practically not reported in Mexico, brought from the outside. The prognosis of the primary cutaneous cases is good, and dissemination occurs only when the patient is immunosuppresed.2,14,16 The histopathology showed a typical granulomatous-tuberculoid like reaction, with few mono-budding yeasts with thick wall, observed with hematoxylin–eosin stain, but more evident with PAS stain.12,14,21,23, We obtained a classic strain of B. dermatitidis, confirmed also as A. dermatitidis by molecular biology techniques (PCR of regions ITS1, and ITS4, dominium D1-D2); this technique brings a specificity and sensitivity nearby 100%.1,12,15,21
According to the Clinical Practice Guidelines for the management of blastomycosis,5 itraconazole is the drug of choice for the non-complicated primary cutaneous cases of blastomycosis, with a dosage of 100–300mg/day, obtaining a good response in three months in average. In our case, the patient responded well to the treatment with itraconazole at 300mg/day, and it is important to emphasize the combined treatment with prednisone (intermediate dose), which prevented fibrosis and retraction of the axillary area. For secondary cutaneous cases the recommended dosage is 400mg/day. The lowest MIC for our B. dermatitidis strain was obtained with voriconazole and posaconazole10; however, we decided to start with itraconazole due to its low cost.10,12,19,21
We consider this is a case of interest of cutaneous blastomycosis acquired in the United States (Indianapolis), but diagnosed and treated in Mexico City, where the disease practically does not exist, reflecting one of the multiple issues related to the migration phenomena between our closest countries.
Funding sourcesNone.
Conflict of interestThe authors declare that there are no conflicts of interest.