Our aim was to evaluate and share our urethrocutaneus fistula repair results in adult patients who had been operated for hypospadias in their childhood.
Material and methodsThe data of totally 48 patients who had been treated for urethrocutaneous fistula after hypospadias surgery in our department from May 2008 to January 2015 analyzed retrospectively. Patients’ age at fistula repair, age at first hypospadias surgery, fistula size, localization and number, distal urethral obstruction status and surgical outcomes of fistula repairs were recorded. All patients were controlled three months after the repair for surgical outcomes.
ResultsFistula repair performed in 45 patients. Mean age was 21.46 (20–26). Nineteen patients (42.2%) underwent first hypospadias surgery under the age of 7 years; 8 patients (17.7%) between 7 and 15 years, 18 patients between 15 and 20 years. Tubularized incised plate urethroplasty (TIPU) was performed in 40 patients (88.9%), extragenital tissue was used in 5 patients (11.1%). Twenty two patients (48.9%) had 1 or 2 operations, 17 patients (37.8%) had 3–5 operations and 6 patients (13.3%) had 6 or more operations. Thirteen (28.9%) coronal, 24 (53.3%) subcoronal, 6 (13.3%) penile and 2 (4.4%) penoscrotal fistulas were observed. While a single fistula was observed in 35 patients, multiple fistulas were seen in 10 patients. A fistula diameter les than 5mm was detected in 37 patients, and larger than 5mm in 8 patients. Fistula recurrence was observed in 3 patients at follow-up examinations carried out at 3 months postoperatively. The number of operations was more than 5, the fistula diameter was larger than 5mm and the fistulas were coronal in all three recurrent fistulas.
ConclusionAccording to our results fistula size, previous surgery and well-vascularised, one or two layer tissue were the important factors in the success of fistula repair after hypospadias surgery.
Nuestro objetivo fue evaluar los resultados de la reparación de la fístula uretrocutánea en pacientes adultos que habían sido operados por hipospadias en su infancia.
Materiales y métodosLos datos de los pacientes que habían sido tratados por fístula uretrocutánea después de la cirugía de hipospadias en nuestro departamento de mayo de 2008 a enero de 2015 analizaron retrospectivamente. Se registraron la edad de los pacientes en la reparación de la fístula, la edad en la primera cirugía de hipospadias, el tamaño de la fístula, la localización y el número, el estado distal de obstrucción uretral y los resultados quirúrgicos de las reparaciones de fístulas. Todos los pacientes fueron controlados tres meses después de la reparación de los resultados quirúrgicos.
ResultadosReparación de la fístula realizada en 45 pacientes. La edad media fue 21.46 (20-26). Diecinueve pacientes (42,2%) fueron sometidos a una primera cirugía de hipospadias menor de 7 años de edad; 8 pacientes (17,7%) entre 7 y 15 edades, 18 pacientes entre 15 y 20 años. Veintidós pacientes (48,9%) tenían una o dos operaciones, 17 pacientes (37,8%) tenían 3-5 operaciones y 6 pacientes (13,3%) tenían 6 o más operaciones. Se observaron 13 (28,9%) coronas, 24 (53,3%) subcoronales, 6 (13,3%) pene y 2 (4,4%) fístulas penoscótalas. Mientras que la fístula aislada observada en 35 pacientes, se observaron múltiples fístulas en 10 pacientes. Se detectó diámetro de la fístula menor de 5mm en 37 pacientes, mayor de 5mm en 8 pacientes. La recurrencia de la fístula se observó en 3 pacientes en los exámenes de control. El número de cirugías fue superior a 5, el diámetro de la fístula fue mayor de 5mm y las fístulas se encontraban en el nivel coronal en las tres fístulas recurrentes.
ConclusiónDe acuerdo con los resultados de la fístula tamaño, las cirugías anteriores y bien vascularizada de una o dos capas de tejido fueron los factores importantes en el éxito de la reparación de la fístula después de la cirugía hipospadias.
Hypospadias is one of the most common congenital anomaly of the penis, effecting one boy per 200 live male births and also the incidence is increasing.1,2 The only option to treat hypospadias is surgical correction. Additionally there is no gold standard technique for this anatomical defect.3 Urethrocutaneous fistula is one of the most common and frequently seen complication after hypospadias surgery with the recurrence rates ranging from 0 to 27% in contemporary series.4,5 This complication mostly requires reoperation.6 Several factors such as distal urethral obstruction, wound infection, use of inappropriate suture materials and poorly vascularized skin flaps for the neourethra can cause urethrocutaneous fistulas. The frequency of fistula formation has decreased as a result of surgeon experience, improvement in operative technique, use of appropriate suture materials and instruments, and coverage of the neourethra with well-vascularized tissue.7,8 A variety of surgical techniques have been described and it is accepted that no single technique is suitable or effective for all patients with fistula.9
In the present study, our aim was to evaluate and share our fistula repair results in adult patients, who had been operated for hypospadias in their childhood.
Material and methodsMedical records of 48 patients who had been treated for urethrocutaneous fistula after hypospadias surgery in our department from May 2008 to January 2015 analyzed retrospectively. Patients’ age at fistula repair, age at first hypospadias surgery, fistula size, localization and number, distal urethral obstruction status and surgical outcomes of fistula repairs were recorded.
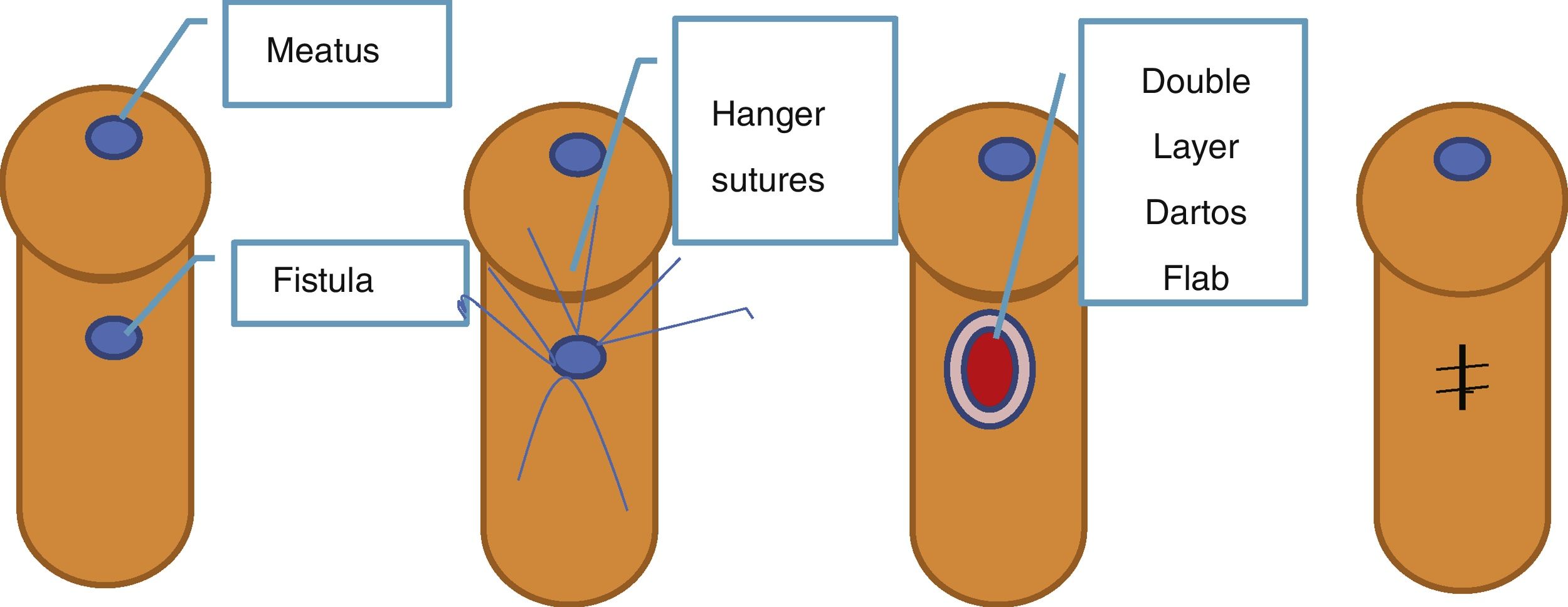
Surgical technique for fistula repair: The fistula repair procedures were performed under local anesthesia with circumferentially penile block by using prilocaine in all patients. Distal part of urethra from fistula to meatus was checked with 16 French (Fr) urethral catheter to exclude any obstruction and if there was, dilatation or meatus incision was performed initially. Then serum saline was given under pressure with nelaton catheter through external meatus to urethra to confirm the exact number and localization of fistulas. Four hanger sutures were applied to edges of fistula then incision was made circumferentially at the border of fistula. Additionally a vertical incision that the fistula locate in the middle was made. Fistula tract was dissected and excised from the connection point with urethra. Two dartos flap were prepared from both side of vertical incision in proximally located fistulas. If fistulas located at corona then flaps were brought from proximal vertical area of the lesion. After inserting a foley catheter with suitable caliber the urethral defect occurred after removal of fistula tract was sutured with 6/0 absorbable material continuously. Then the suture line was covered with two dartos flaps as two layers. After skin closure with 4/0 absorbable material an elastic bandage was applied for 2 days and foley catheter was kept at least 3 days. All patients were controlled three months after the repair for surgical outcomes (Fig. 1).
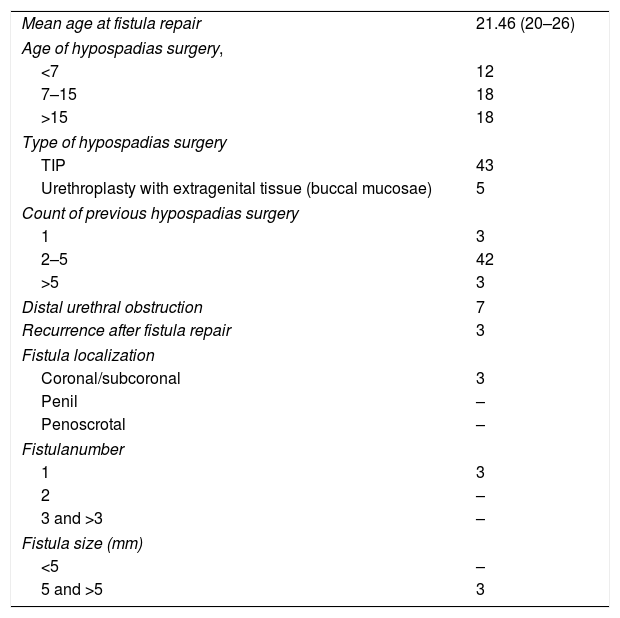
ResultsFistula repair performed in 45 patients, whose mean age was 21.46 (20–26). Nineteen patients (42.2%) underwent first hypospadias surgery younger than 7 year of age; 8 patients (17.7%) had first operation between 7 and 15 ages, 18 patients’ first hypospadias operation between 15 and 20 ages. While tabularized incised plate urethroplasty (TIPU) performed in 40 patients (88.9%), extra genital tissue was used in 5 patients (%11.1). Twenty two patients (48.9%) had 1 or 2 operations, 17 patients (37.8%) had 3–5 operations and 6 patients (13.3%) had 6 or more operations. When the patients were assessed for fistula levels, 13 (28.9%) coronal, 24 (53.3%) subcoronal, 6 (13.3%) penile, and 2 (4.4%) penoscrotal fistulas were observed. While single fistula observed in 35 patients, multiple fistulas were seen in 10 patients. Fistula diameter was detected smaller than 5mm in 37 patients, larger than 5mm in 8 patients. Fistula recurrence was observed in 3 patients in the control examinations carried out at 3 months postoperatively. The number of surgeries was more than 5, fistula diameter was larger than 5mm and fistulas were in the coronal level in all three recurrent fistulas (Table 1).
Data of patients.
| Mean age at fistula repair | 21.46 (20–26) |
| Age of hypospadias surgery, | |
| <7 | 12 |
| 7–15 | 18 |
| >15 | 18 |
| Type of hypospadias surgery | |
| TIP | 43 |
| Urethroplasty with extragenital tissue (buccal mucosae) | 5 |
| Count of previous hypospadias surgery | |
| 1 | 3 |
| 2–5 | 42 |
| >5 | 3 |
| Distal urethral obstruction | 7 |
| Recurrence after fistula repair | 3 |
| Fistula localization | |
| Coronal/subcoronal | 3 |
| Penil | – |
| Penoscrotal | – |
| Fistulanumber | |
| 1 | 3 |
| 2 | – |
| 3 and >3 | – |
| Fistula size (mm) | |
| <5 | – |
| 5 and >5 | 3 |
Tissue ischemia and infection risk has come to the fore for urethral fistula formation following hypospadias repair. It is important to use proper prophylactic antibiotics in preventing fistula formation, use broad-based flaps not to be fed poorly and urethral diversion was kept in time to allow wound healing.10 The success of the fistula repair depends on fistula location and number of previous surgery.11,12 There are restricted number of study determined fistula size. Huang et al. did not find any effect of the fistula size.13 However, in our study, fistula recurrences were seen in patients with larger fistula size.
Especially success rates are lower in coronal and granular sulcus located fistulas because of inadequacy of surrounding tissues and mobilization problems.14 All recurrent fistulas were located in coronal level in our patients.
Urethral covering is advised to minimize the fistula formation by harvesting a flap from scrotal fascia, preputial skin, dorsal or ventral subcutaneous tissue.15–17 Also double dartos flaps are better preventing fistula formation.18 In our patients we used two or three layer dartos flaps to prevent fistula formation. Thus, we achieved the reduction of recurrence. Our technique for fistula repair with two layer dartos flaps seems to be the main current treatment of this pathology.
ConclusionAccording to our results, by observation of the patients, fistula size, previous surgeries and well-vascularized one or two layer tissue were the important factors in the success of fistula repair after hypospadias surgery.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestNone declared.