Our aim was to assess our TIP urethroplasty results in adults with local anaesthesia.
Materials and methodsMedical records of adult patients who underwent TIP urethroplasty due to distal hypospadias in our clinic between April 2006 and May 2013 were reviewed. Patient's age, external urethral location, preoperative calibration size of urethra, primary or secondary or more, circumsized or uncircumsized conditions were recorded. The records were categorized as circumcised–uncircumcised, urethral stent calibration 16Fr and above or 14Fr and below, primer or seconder and above, special group or the others. SPSS 16.0 were used for statistical assessment and chi-square test was used to determine success. p<0.05 was considered to show statistical significance.
Results51 patients underwent distal hipospadias repair under local anaesthesia in our clinic between April 2006 and May 2013. Mean age was 21.3. 24 patients had coronal, 26 patients had subcoronal, 1 patient had glanuler hypospadias. 40 patients were primary, 7 secondary, 4 tertiary. 38 patients were circumsized. 13 patients were uncircumsized. Mean preoperative calibration was 14.8Fr, mean urethral stent calibre was 15, 1Fr, mean stent duration time was 5.9 day. Suprapubic catheter was used for drainage at 48 patients. 22(52.3%) were successful, 20(47.6%) were unsuccessful of 42 patients with follow up. 13 patients that had fistula underwent fistula repair after 3 months later under local anaesthesia. 2 patients had stricture and they underwent meatotomy and dilatation. On one patient, second TIP urethoplasty operation was performed because the first operation was unsuccessful. Operation was very successful and it upgraded our over all success to 90.4%. An optimal group as primary, uncircumcised, 16Fr neourethra was formed and were compared with the other groups. Success rate between optimal group and others was not different statistically.
ConclusionOur success rate was similar to literature. This survey reveals that distal hypospadias repair can be performed under local anaesthesia.
Nuestro objetivo fue evaluar los resultados obtenidos para la uretroplastia mediante incisión y tubularización de la placa uretral (TIP) con anestesia local en adultos.
Materiales y métodosSe revisó el historial clínico de los adultos que se sometiedon a una uretroplastia TIP debido a hipospadias distales entre abril del 2006 y mayo del 2013. Se catalogaron los parámetros de edad, ubicación externa de la uretra, calibración uretral preoperatoria, primario o secundario o más, circuncisión o no. Los valores se clasificaron como circuncidado-no circuncidado, calibración del stent uretral de 16 Fr o mayor o 14 Fr o menor, primario o secundario o más, grupo especial o el resto. Para valorar el éxito, el análisis estadístico se realizó con el sistema SPSS 16.0 y la prueba de la χ2. Los resultados p<0,05 no se consideraron significativos.
ResultadosSe intervino a 51 pacientes para reparación de hipospadias con anestesia local entre abril del 2006 y mayo del 2013. La media de edad fue de 21,3. Las hipospadias fueron coronales en 24 pacientes, subcoronales en 26 y granulares en uno. 40 pacientes fueron de tipo primario, 7 de tipo secundario y 4 de tipo terciario. 38 pacientes estaban circuncidados, 13 no lo estaban. La calibración media preoperatoria fue de 14,8 Fr, la calibración meadia del stent uretral due de 15,1 Fr, la duración media del stent fue de 5,9 días. Se utilizó una sonda suprapúbica para drenaje en 48 pacientes. De los 42 pacientes que acudieron a seguimiento, 22 (52,3%) consiguieron un resultado satisfactorio y 20 (47,6%) fueron casos fallidos. 13 pacientes que presentaron una fístula se sometieron a la reparación de la misma con anestesia local tres meses después. 2 pacientes presentaron estenosis y se sometieron a una meatotomía y dilatación. Uno de los pacientes precisó una segunda uretroplastia TIP debido a que la primera operación fue fallida. Esta segunda intervención fue muy satisfactoria y aumentó el nivel de éxito hasta el 90,4%. Se formó un grupo óptimo formado por pacientes primarios, no circuncidados, 16 Fr neouretra para compararlo con el resto de grupos. Estadísticamente no se apreciaron cambios entre el grupo óptimo y el resto de grupos.
ConclusiónNuestro nivel de éxito fue similar al de la literatura. Esta encuesta revela que la reparación de hipospadias distales puede realizarse con anestesia local.
Hypospadias is proximally located urethral meatus on the ventral surface of the penis that is a result of incomplete tubularization during embryonic age. Hypospadias is a common congenital anomaly occurring 3.2 per 1000 live births.1 Hypospadias should be corrected by surgery during an optimum age between 6 and 18 months.2 TIP urethroplasty is described by Snodgrass in 19943 and it became very popular due to its good cosmetic and functional outcomes. In some developing countries it is not rare to see men with primary hypospadias in urology clinics and these patients will need hypospadias repair in adulthood ages. Hypospadias repair made under general and regional anaesthesia in literature.4 Penile blocks can be used to provide intraoperative and postoperative analgesia in patients undergoing hypospadias repair.5 Local anaesthesia can also effectively be used for penile surgery in adults.6 In this study, we assessed our TIP urethroplasty results in adults with local anaesthesia.
Materials and methodsInstitutional ethical committee approval was taken before assessment. Medical records of adult patients who underwent TIP urethroplasty due to distal hypospadias in our clinic between April 2006 and May 2013 were reviewed.
Penile chordee was assessed with photographs taken by patients during erection; consequently patients with chordee were excluded from study. Patient's age, external urethral location, preoperative urethral calibration results, hypospadias status (primary/redo) and the penis circumsized or not were noted.
10ml of 2% prilocaine for local anaesthesia was used and initially dorsal penileblock was performed. Circular infiltration was also performed as Malkoc et al.6 did at the adult circumcision. Tourniquet was used to prevent bleeding during surgery for not more than 20min. The tubularization was made with TIP urethroplasty as described by Snodgrass.3 In 48 patients, nelaton catheter (size range 14–18Fr) was placed into the urethra.
Suprapubic catheter (cystofix) was used for urinary drainage in every patient. Mean catheter stay duration was 5.9 days (day range 4–7). Dartos fleb for second layer above the neourethra was placed. In every patient, antibiotics were used until catheter removal. Patients got urinated 1 day after catheter extraction and they were assessed 1 day and 1 month after the extraction. In the case of presence fistula after, TIP urethroplasty patients underwent fistula repair three to six months after the first operation. In the case of meatal stricture, the patients underwent meatotomy and dilatation after the operation.
The parameters were divided into groups as circumsized or not circumsized, urethral stent diameter <14Fr and >16Fr and primary or redo hypospadias. SPSS 16.0 were used for statistical assessment and chi-square test was used to determine success. p<0.05 was considered to show statistical significance.
ResultsFifty-one patients underwent distal hypospadias repair under local anaesthesia in our clinic between April 2006 and May 2013. Mean age was 21.3 (age range 20–28 years). 24 patients had coronal, 25 patients had subcoronal, 1 patient had glanular and 1 patient had distal penile hypospadias. Forty patients were primary and the others were having redo hypospadias. Of the patients, 38 were circumsized and the others (13) were not.
Mean preoperativeurethral calibration was 14.8 Fr (size range 6–24), mean urethral stent diameter was 15, 1Fr (size range 14–18). The mean stent duration time was 5.9 days (range 4–7). Suprapubic catheter was used for drainage in 48 patients. The other 3 cases had urethral catheter.
The success rate was 52.3% (22 patients) and 47.6% of the cases were unsuccessful due to the fistula, stricture or slough. Thirteen of the patients who had fistula underwent fistula repair after 6 months later under local anaesthesia. One of the patients required a secondary fistula repair. Two of the patients had urethral meatal stenosis and they underwent meatotomy and urethral dilatation. In one patient, secondary TIP urethoplasty needed because the first operation was unsuccessful.
After the surgical corrections (inc. Fistula repair), our total success rate was 90.4% (38/42 cases).
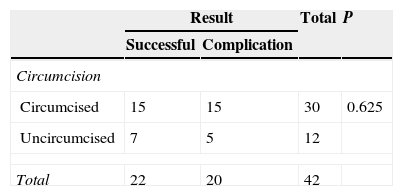
Half of the patients who were circumsized have had successful hypospadias repair, but the other 50% did not. On the other hand, 5/12 uncircumsized cases had complications (41%) (Table 1).
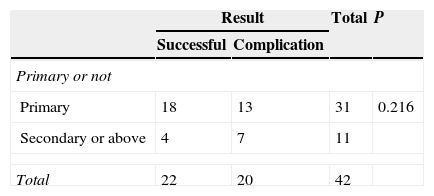
Eighteen (58%) of the 31 patients with primary hypospadias were having successful outcomes whereas the other 13(41.9%) were unsuccessful. Four (36.3%) of 11 redo hypospadias were successful and 7(63.8%) were not. Success rate between them were not statistically significant (p=0.219) (Table 2). The differences between the two rates were not statistically significant.
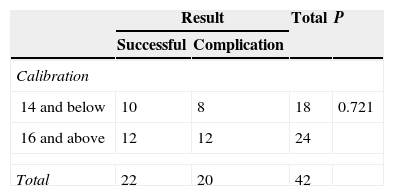
The patients whose neourethra were done around 14Fr or smaller stents were having 55.5% success rate. Only the half of the cases who had 16Fr or bigger stents did not need further treatment. Difference between the two groups was not statistically significant (p=0.721) (Table 3).
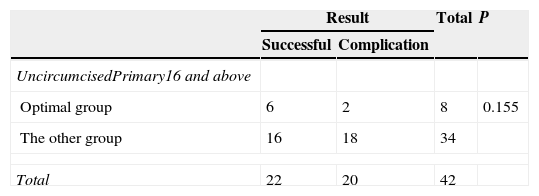
The patients with primary hypospadias, uncircumcised penis and with >16Fr stents during the surgery composed the optimal group. A total of 8 patients were having these criteria. The success rate in this group was 75% (6/8 cases). The other patients out of this group were having 47% success rate. The other 18 cases (53%) needed secondary (or tertiary) treatments. The difference between the success rate of the optimal and the other group were not statistically significant (p=0.155) (Table 4). In the optimal group after two fistula repair, the success rate was reached to100%.
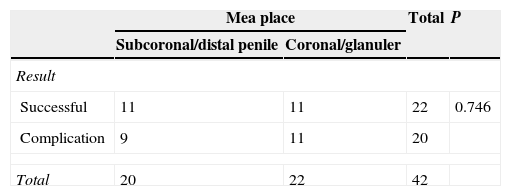
When the whole patients were divided into two groups according to their meatal placements, patients with subcorronal meatus composed the first and the others with coronal and glanular meatus formed the second group. The success rate was not different between groups and were 55% (11/20) and 50% (11/22), respectively (p=0.746) (Table 5).
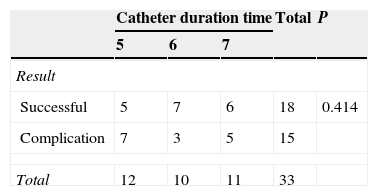
If the patients were divided into three groups by their catheter duration time (group1: 5 days, groups 2: 6 days, and group 3: 7 days) the success rates of the groups were 41.6% (5/12 cases), 70% (7/10 cases), and 54.6% (6/11 cases), respectively. There were no statistically significant differences between the groups’ success rates (p=0.414) (Table 6).
DiscussionThe main target of hypospadias repair is well-functioning urethra and aesthetic appearance of penis. Adult hypospadias repair is not as successful as childhood.7 Because infection risk is higher and nocturnal erections have negative effects on the outcome. Hensle et al.8 reported 88.1% success rate in 42 patients. Senkul et al.7 reported 89.6% overall success rate in 88 patients after the fistula repairing surgery. Adayener and Akyol9 reported 88% overall success rate in 97 patients.
Hypospadias repair made under general and regional anaesthesia in literature.4 Penile surgeries can also be done under local anaesthesia.6 10ml of 2% prilocaine for local anaesthesia was used and initially dorsal penileblock was performed. Circular infiltration was also performed as Malkoc et al.6 did at the adult circumcision. In this way we show that this surgery can be done under local anaesthesia. None of the patients needed general or regional anaesthesia.
Circumcision is not suggested to patients with hypospadias because the possible additional tissue needs. It is regarded that hypospadias repair success rate decreases in circumcised patients. There was no patients statistically difference between the two groups according to our findings; circumcision does not affect the complication rate. Also Rashed and Gholizade10 studied 30 circumcised and 30 uncircumcised with hypospadias and did not find any difference between them. This is also relevant to our findings.
Despite the fact that secondary patients have more complications than primary patients there was no statistically difference in our study. Also El-Sherbiny et al.11 assessed 133 patients about complication rate at primary and secondary patients. There were no statistically differences between them.
Fistula risk increases due to distal stricture, therefore catheter diameter is important to prevent stricture. Our patients were categorized into two groups as 14Fr and below, 16Fr and above. Any statistical difference was found finally.
An optimal group was formed as uncircumcised, primary, 16Fr catheter. When this group was compared with others there were no statistically difference. Although optimal group's success was 75% fistula was observed on two unsuccessful surgery and patients underwent fistula repair after 3 months. The results were considerably successful.
Complication rates of proximal and midpenil hypospadias repair are higher then distal hypospadias repair.12 Our patients group had distal hypospadias. Patients were divided into two groups as proximal (subcoronal and distal penile) and distal (coronal and glanuler), there was not statistically difference. This is why our patients all had distal hypospadias actually.
There was no statistically difference according to catheter duration time. The catheter can be placed between 5 and 7 days.
The overall success rate increased to 90.4% after second intervention. This is compatible with the surgeries under general anaesthesia in the literature. Second interventions were also made under local anaesthesia. It increases the success rate in first surgery to choose the patients as primary, uncircumcised and 16Fr calibre urethra.
There are various penile surgeries under local anaesthesia in the literature. Chien et al.13 performed penile plication under local anaesthesia with 95% success rates. Hsu et al.14 did penile implantation with crural block. Also Malkoc et al.4 did adult circumsizion under local anaesthesia. We also showed that penile surgeries can be done under local anaesthesia with a success rate as general anaesthesia.
Our study is retrospective and the number of the patients is low. These are the limitations of our study. Because of the low count of the patients there was not statistically difference between the groups.
ConclusionAlthough success rate of adult hypospadias repair is low due to infection and nocturnal erections and also it is reported nearly 90% success rate in the literature. This success rate was achieved under local anaesthesia in our study. This survey reveals that distal hypospadias repair can be performed under local anaesthesia.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare no conflict of interest.