Despite significant advances in medical therapy, particularly biological agents, a significant number of patients still need surgery as an important therapeutic tool in Crohn's disease (CD). The role of a surgeon in the multidisciplinary team in inflammatory bowel disease care is essential. Discussion with gastroenterologists, radiologists and dietitians to proper define the best timing of surgery after optimization and the best surgical strategy that will be used impact in better postoperative outcomes in CD patients. In this review the authors discuss important aspects involved in the surgical strategies of the multidisciplinary management of CD, including preoperative planning and optimization, the definition of the more adequate approach and technique according to the disease location, and adequate prevention of postoperative recurrence. Several aspects including patients’ past and present features are important in making the right decision in the surgical management of CD. Adequate preparation of the nutritional status, correction of anemia, optimization of medical therapy and anatomic mapping of the small bowel and colon with imaging tests are essential for the definition of best timing and type of surgery in abdominal resections in CD patients. This fact demonstrates the specific need for a multidisciplinary team in the management of CD surgical patients.
A pesar de los avances significativos en la terapia médica, particularmente de los agentes biológicos, aún un número significativo de pacientes con enfermedad de Crohn (EC) necesitará de la cirugía como una importante estrategia terapéutica. El papel del coloproctólogo en el equipo multidisciplinario de enfermedad inflamatoria intestinal es fundamental. La discusión con gastroenterólogos, radiólogos y nutriólogos para definir el mejor momento de la cirugía post optimización y la mejor estrategia quirúrgica que se utilizará, impactará en mejores resultados postoperatorios en pacientes con EC. En esta revisión, discutimos importantes aspectos relacionados con las estrategias quirúrgicas del manejo multidisciplinario de la EC, incluyendo el manejo preoperatorio y optimización, la definición del enfoque y la técnica más adecuada de acuerdo a la ubicación de la enfermedad y la prevención más apropiada para el manejo de la recurrencia postoperatoria. Otras variables tales como los antecedentes y las características actuales del paciente, son importantes para tomar la decisión correcta en el tratamiento quirúrgico de la EC. La adecuada preparación del estado nutricional, la corrección de la anemia, la optimización de la terapia médica y la evaluación del intestino delgado y del colon a través de estudios de imágenes son esenciales para definir el mejor momento y el tipo de cirugía en las resecciones intestinales en pacientes con EC. Este hecho muestra la necesidad de un equipo multidisciplinario especializado en el manejo de pacientes quirúrgicos con EC.
Crohn's disease (CD) can be associated with structural damage in the bowel. The natural history of CD is usually constituted by an evolution from inflammatory lesions at the mucosal level to stenosis and consequent perforation, as abscesses and internal or external fistulas1. Unfortunately, in some cases, irreversible damage of an intestinal segment appears at the beginning of the disease course, or even in the presence of optimal medical therapy2.These constitute the most common indications for surgery, despite most dramatic scenarios such as intestinal perforation, toxic megacolon or cancer may be present in the long-term disease course of a CD patient. Actually, in spite of the advances in medical therapy, particularly biological agents, a significant number of patients still need surgery as an important tool in the therapeutic armamentarium3,4 and the available data are controversial regarding reduction in surgery rates after the biologic era5–10.
Chronic evolution and heterogenous biological behavior are associated with different clinical presentations in CD. Choosing the best time for surgery is difficult and surgeons have to deal with different scenarios, from simple stenosis to larger inflammatory masses involving more than one intestinal segment or adjacent structures. All these aspects interfere with the definition of the more adequate surgical approach, post-operative morbidity and long-term outcomes. The basic pillars of surgical therapy in CD are identification of risk factors associated with complications; performing economic intestinal resections; bowel preserving surgery (strictureplasties whenever possible); adequate preoperative optimization and different surgical options according to the location and phenotype of the disease.
The aim of this review is to discuss important aspects involved in the surgical strategies of the multidisciplinary management of CD, including preoperative planning and optimization, definition of the more adequate approach and surgical technique according to disease location, and adequate prevention of postoperative recurrence.
2PREOPERATIVE PLANNING2.1A IMAGING METHODSAdequate identification of affected intestinal segments is crucial for preoperative planning in abdominal CD, particularly with minimally invasive techniques including single-port, laparoscopic or robotic surgery. Three modalities of tests are currently available with adequate correlation with intra- operative findings: ultrasonography (US), MRE (magnetic ressonance enterography) or CTE (computed tomography enterography). All these types of imaging modalities are able to identify disease complications such as stenosis, abscesses, internal or external fistulas and even active inflammation at different layers of the bowel11,12.These findings are important for adequate differentiation between fibrotic or inflammatory stenosis and are useful for planning the extension of intestinal resection or for better definition of proper intestinal segments which can be suitable to strictureplasties.
US is a less expensive method, with no exposure to radiation. The examination, usually aiming evaluation of the small bowel and colon, is usually fast and well tolerated, with good correlation to CTE or MRE findings in different studies, in expert hands13,14. It allows adequate identification of bowel wall thickness, presence of abscesses, and precise definition of primary and secondary segments in fistulas. However, it is operator dependent and review of imaging findings can be challenging, as it is a dynamic test.
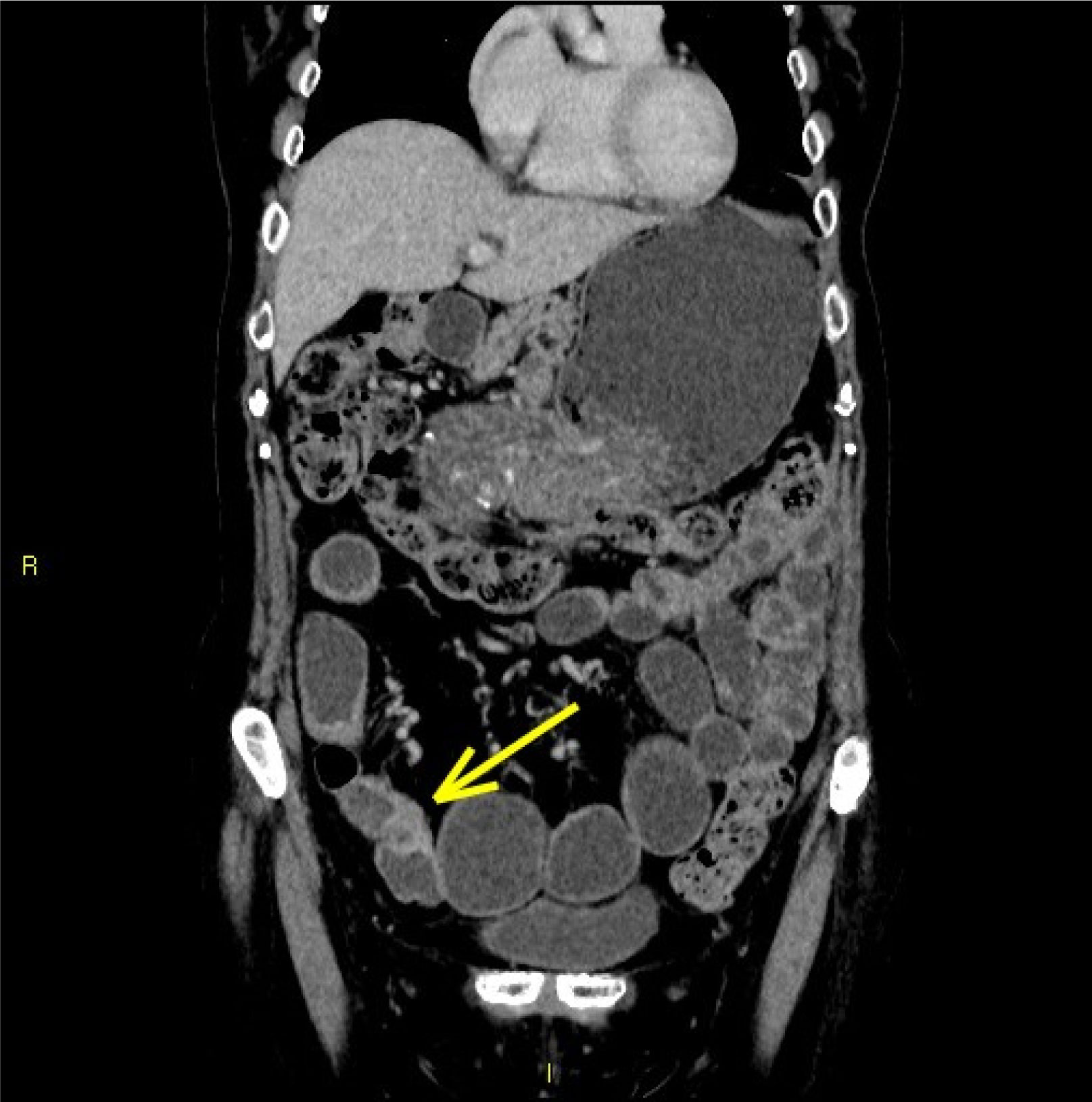
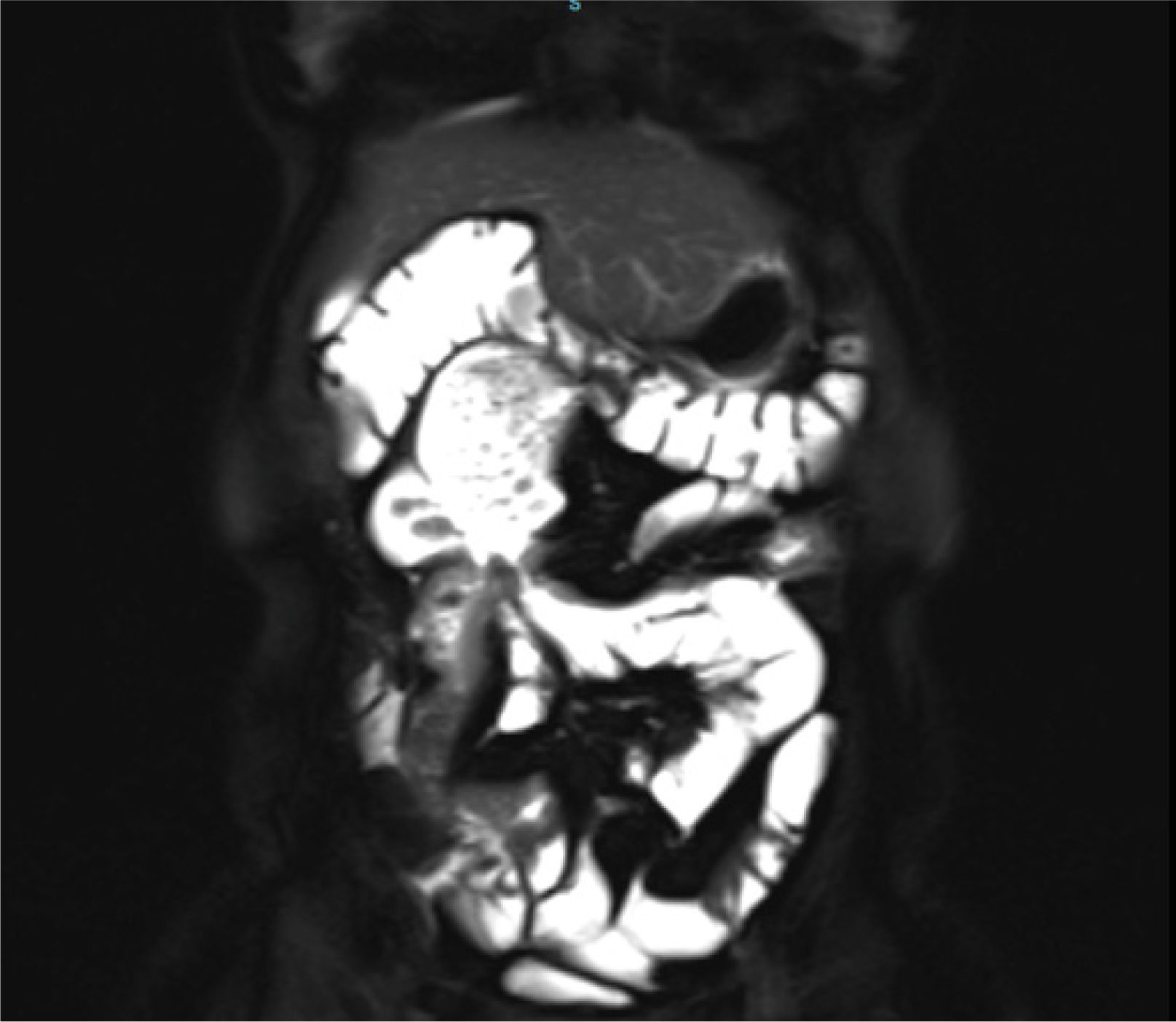
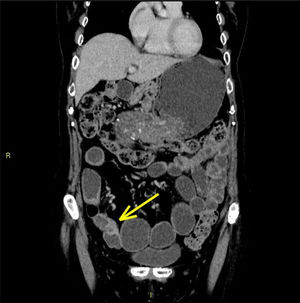
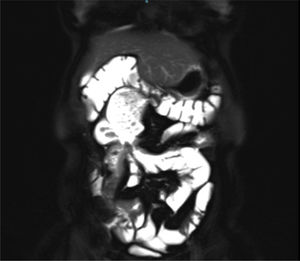
MRE (figure 1) and CTE (figure 2) have similar sensitivity for differentiation between inflammatory or fibrotic stenosis and are able to identify fistulous tracks or even specific features in retroperitoneal spaces or within pelvis15,16. Both methods require specific protocols and oral fluid intake for intestinal distension (usually laxatives). MRE has a big advantage over CTE, as there is no radiation exposure. However, the test usually demands longer periods inside imaging equipment, what can cause discomfort to some patients, secondary to claustrophobic sensation. Regarding preoperative evaluation, particularly with laparoscopic or robotic approaches, which can sometimes lead to difficulties in intraoperative evaluation of the whole extension of small bowel, MRE and CTE must be considered as the methods of choice. They are associated to better correlation with the intraoperative findings, since US has limitations regarding the view of the small intestine as a whole.
Currently, no adequate surgical indication can be done without preoperative adequate imaging mapping. For that reason, a close relation between the surgeon and radiologist is essential for adequate surgical planning and constitute one of the most important aspects of the multidisciplinary team in inflammatory bowel disease units over the globe.
2.2B. PREOPERATIVE NUTRITIONAL EVALUATION AND OPTIMIZATIONMalnutrition is frequent in CD patients secondary to insufficient dietary intake, malabsorption and systemic inflammation which can cause catabolism and reduced protein synthesis. Particularly in patients who are candidates to major abdominal surgery, all these three aspects may be present in association. For example, a patient with ileal involvement with poor therapeutic response frequently can be present with stenosis and active luminal inflammation. Poor nutritional status, evidenced by weight loss greater than 10% of body weight, serum albumin lower than 3g/dl and a BMI lower than 18,5kg/m2 are associated with worse postoperative outcomes in CD17,21. Hypoalbuminemia is strongly associated with worse postoperative outcomes and preoperative nutrition treatment can reduce overall complications and the need for stomas18,22.
Exclusive enteral nutrition (EEN) is an effective bridge to better timing of elective surgery for malnourished adults with CD. In patients with phlegmons or other semi-urgent surgical indications, preoperative optimization with EEN helps patients in two ways: reduction of the inflammatory burden and correction of associated malnutrition24–26. EEN is cheaper than parenteral nutrition (PN) and avoids central catheter complications. A retrospective study showed a clear benefit with EEN 3 months prior to surgery, with less intraoperative septic conditions and better surgical outcomes27. Some studies reported that the use of preoperative total parenteral nutrition was also associated with lower post-operative morbidity, when the enteral route could not be used28,29.
Thus, nutritional supplementation has been associated with a positive impact and better postoperative outcomes in major abdominal surgery in CD, and it is recommended even if the surgical procedure needs to be postponed. It must be considered that the best route or supplemental duration necessary to be employed are not yet well determined in the literature and need to be defined in an individualized basis in the multidisciplinary team, together with gastroenterologists and dietitians.
2.3C. PREOPERATIVE MEDICAL THERAPYMost of CD patients who undergo surgery have a previous history of medical treatment failure and most of them are under treatment with immunosuppressive drugs or biological agents. Thus, the impact of perioperative medical therapy needs to be considered regarding its effect in postoperative outcomes. It is well established that steroids have a negative impact and increase the risk of infectious and overall postoperative complications30. Tzivanakis et al. showed that for ileocolic resections, the use of corticosteroids in patients with abdominal abscesses is associated with dehiscences in up to 40% of the cases, and surgeons must consider the need for intestinal stomas in these situations31. In this study, previous steroids (OR 2.67, 95% CI 1.0-7.2) and preoperative abscesses (OR 3.4, 95% CI 1.2-9.8) were identified as independent predictors of anastomotic complications. In the absence of both steroids and intra-abdominal abscess, the risk of anastomotic complications was only 6%, which increased to 14% if either risk factor was present. When both risk factors were present, complication rates reached 40%. There is scarce data regarding the postoperative impact of preoperative use of immunomodulators such as azathioprine, 6-mercaptopurine or methotrexate, but the majority of the studies demonstrate that this class of drugs can be safely used in the perioperative period, and do not increase morbidity32.
The impact of preoperative use of biological therapy in major abdominal surgery in CD patients remains controversial. Nowadays, many patients who undergo surgery are previously using biological therapy and concerns regarding septic and anastomotic complications are still present. The use of anti-TNF (tumor necrosis factor) agents has been associated with septic complications according to a meta-analysis33.Another multicentric study suggested that the preoperative use of anti-TNF agents can be associated with higher anastomotic leak rates after ileocolic resections34. Several studies did not find a negative association between biologics and worse postoperative outcomes, and current data are controversial probably due to methodological discrepancies35–37.
Few prospective studies were published over this topic. Lau et al. showed that there may be an association between higher serum levels of infliximab and overall postoperative complications in CD patients, but not in ulcerative colitis38.More prospective studies with other biological agents, such as vedolizumab and ustekinumab are also warranted.
2.4D. THROMBOEMBOLISM PROPHYLAXISInflammatory bowel diseases are associated with greater risk of thromboembolic events (TEE), mostly in patients with high inflammatory burden, and during hospital admissions with or without an associated surgical procedure, with a prevalence as high as 39% in necropsies39,40. Imbrizi et al. identified the occurrence of 15.1% of venous thrombosis in hospitalized CD patients and the authors described that low serum levels of albumin were a strong predictor of this occurrence41.
Postoperative CD patients have even a greater risk for thromboembolic events. Since specific conditions associated with surgery such as positioning on the operating table, dehydration, long-standing surgery, thrombophilia and steroid use predispose to these events42. Adequate prophylaxis with pneumatic intermittent compression in the lower limbs during hospital stay and the use of low molecular weight heparin must be employed until 4 weeks after discharge in specific cases. The ECCO (European Crohn's and Colitis Organisation) guidelines CD state that a combination of mechanical and pharmacological thrombosis prophylaxis should be considered in CD patients requiring surgery, and extended for 4 weeks in all IBD patients32.
3SMALL BOWEL CD: STRICTUREPLASTY VERSUS SEGMENTAL RESECTIONPatients with CD have an increased risk of multiple operations and prevention of intestinal failure is one of the main goals of surgical therapy. In small bowel location, bowel preserving surgical techniques are largely employed with good results and low morbidity. Since stenosis is the most frequent indication for surgery, strictureplasties constitute a good option for cases with multiple involved segments or previous surgical resections43.
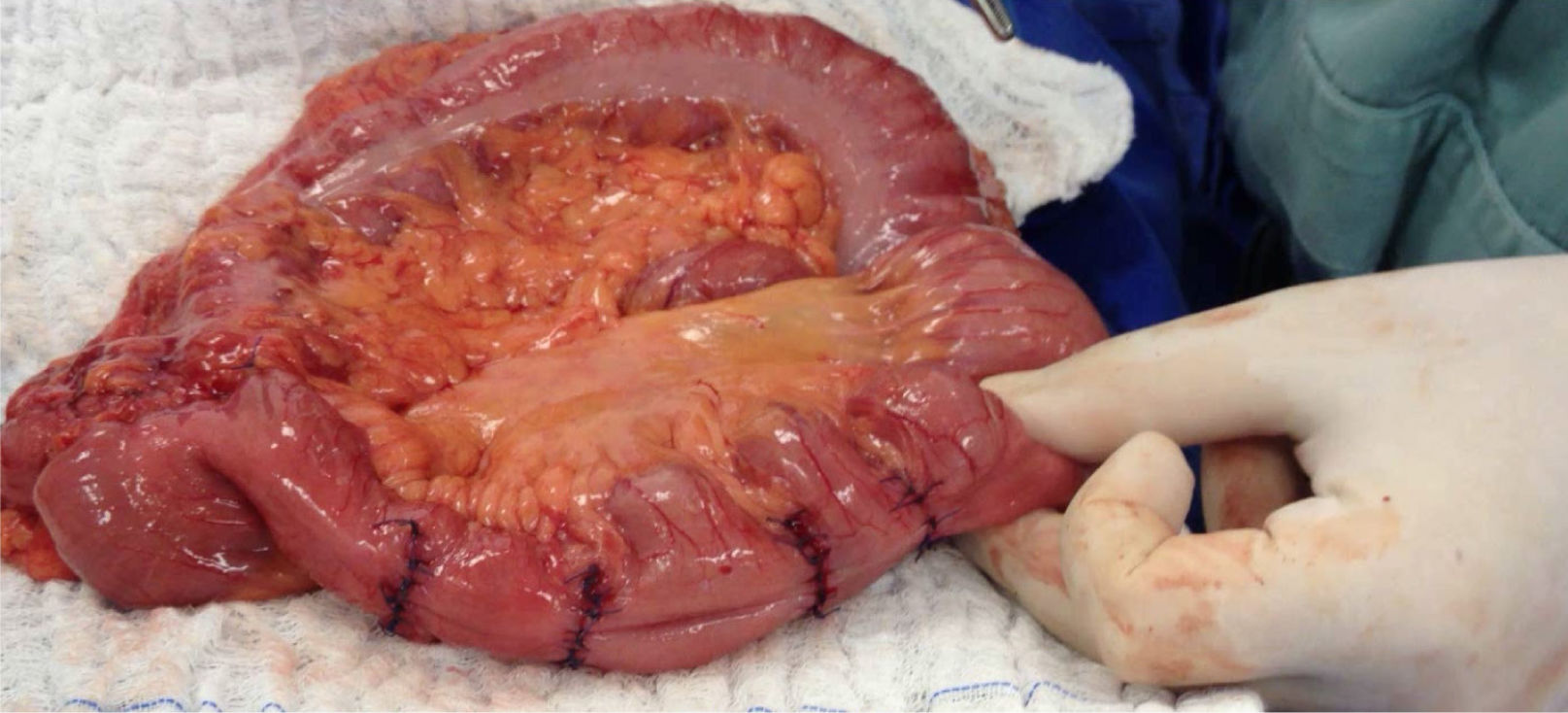
There are multiple options of types of strictureplasties, according to the number and extension of the stenosis. The Heineke-Mikulicz technique is the most used procedure, with a clear indication for short and multiple stenosis (figure 3). It is performed by opening the stenosis longitudinally and closing the defect transversely, increasing the diameter of the affected bowel. This is a safe technique, and despite performed sometimes in inflamed tissue, leak rates are low. The Finney technique may be an option for longer stenosis, but in the authorś personal experience is often associated with recurrence and stenosis at the mesenteric junction of the bowel segments, leading in some cases to dilatation, bacterial overgrowth, functional motility problems and diarrhea. Stenosis which are associated to internal or external fistulas constitute an absolute contraindication for bowel preserving surgery with strictureplasties, due to higher risk of anastomotic dehiscence. More recently, longer strictureplasties as the Michelassi procedure or the ileocecal side-to-side technique were described. These strategies have a special role in patients with multiple previous resections, avoiding short bowel syndrome. The results in experienced centers are comparable with other strictureplasties, and the decision of their application in clinical practice needs to be individualized in a multidisciplinary manner44,45.
As the most common location of CD is the terminal ileum and ileocecal junction, ileocolonic resection is the most common abdominal surgical procedure performed. Intrinsic difficulties regarding the friable mesentery need to be taken into account in this operation. After resection, anastomotic techniques do not appear to affect the postoperative outcome with similar results comparing end-to-end versus side-to-side ileocolonic anastomosis46. Nevertheless, anti-peristaltic side-to-side anastomosis (functional end-to-end) makes the evaluation of the neoterminal ileum difficult in future colonoscopies to evaluate endoscopic recurrence, and for this reason the authors recommend avoidance of this technique. Isoperistaltic side-to-side anastomosis is the preferred technique and can be performed with open surgery or by the laparoscopic approach (intra or extracorporeally).
It is known that different variations in surgical procedures do not affect recurrence. Recently, Coffey et al. described a technical aspect probably associated with lower recurrence rates. The authors demonstrated lower surgical recurrence with the extension of the ileocolic resection with the corresponding mesentery. The possible explanation for these findings is that the excision of the mesentery removes lymphoid tissue, diminishing the local influx of inflammatory cells towards the bowel layers. Future studies comparing mesenteric preservation or excision are warranted in the IBD field47.
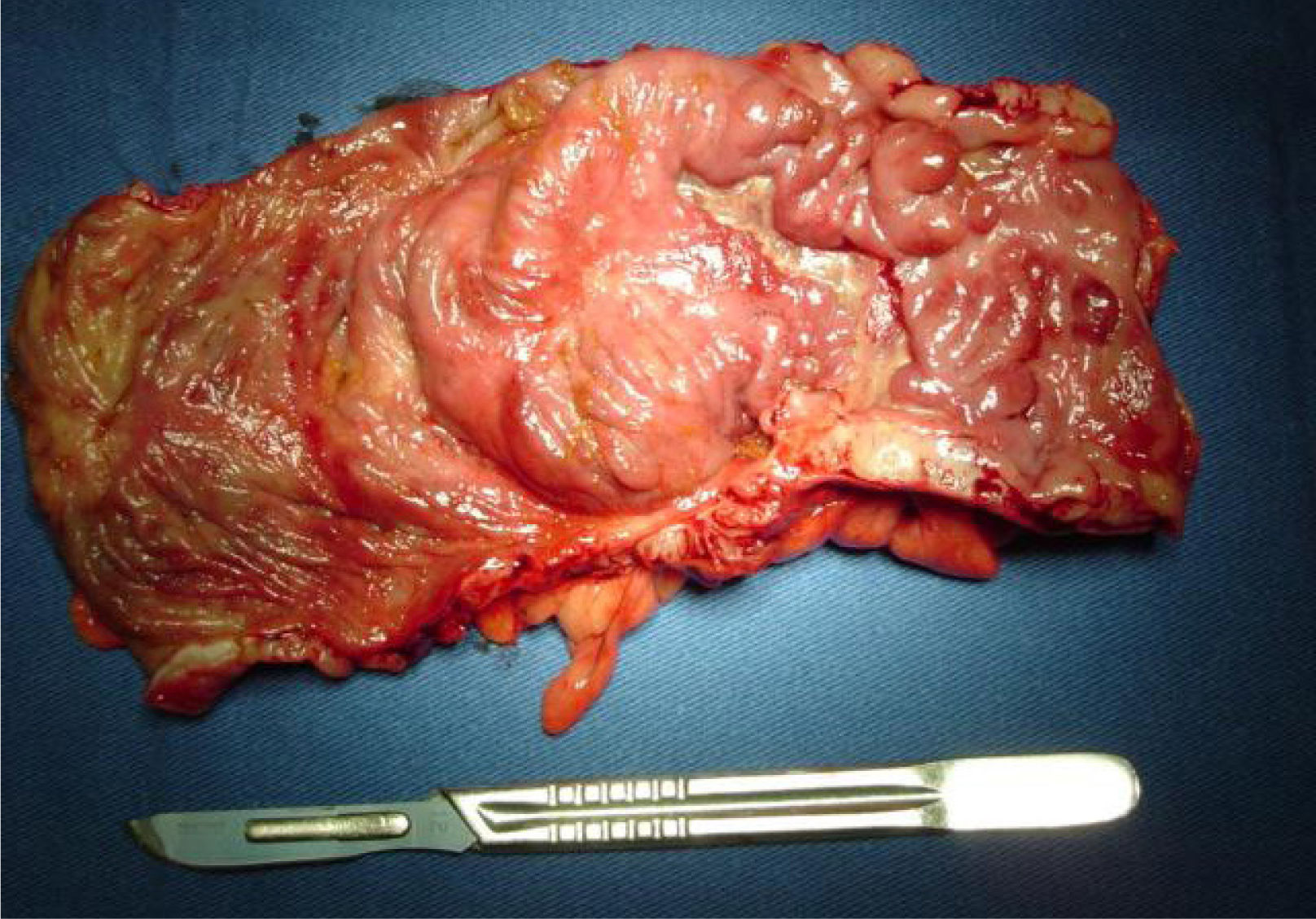
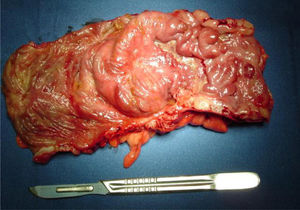
4COLONIC CD: SEGMENTAL VERSUS TOTAL COLECTOMYColonic involvement represents a challenging location for the surgical management of CD. Usually, toxic megacolon, associated cancer, dysplasia or major bleeding are indications for total colectomy, despite being rare situations seen in clinical practice. Segmental resections are usually indicated when one segment of the colon is affected (figure 4). They are less technically demanding but are associated with higher recurrence rates and must be considered in cases with associated small bowel involvement or perianal disease. In patients with multiple affected colonic segments, a total colectomy is indicated when there is no perianal disease and the rectum is spared, in association with an ileorectal anastomosis. Patients with rectal involvement and perianal disease can be candidates for a total proctocolectomy and a permanent ileostomy. A meta-analysis demonstrated similar results with total or segmental colectomy in terms of complications. Recurrence rates seem to be higher in segmental resections, despite better functional results. Most of the studies comparing segmental versus total colectomies were performed before the overspread use of biological therapy. If the use of biologics increased the number of segmental resections, this still needs to be proved32,48.
5LAPAROSCOPIC SURGERY IN CDThe laparoscopic approach in CD is associated with all the advantages of laparoscopy, as better cosmesis, reduced surgical trauma, more rapid recovery and shorter hospital stay. With advances in surgical technique and equipment, laparoscopy remains the gold standard approach in abdominal surgery for CD (figure 5). Even in patients with previous operations or penetrating phenotype, laparoscopic resections are feasible and associated with good results. The more experienced the center is, the lower the conversion rates will be49,50. Despite several advantages, the use of laparoscopic techniques is not associated to differences in terms of postoperative endoscopic recurrence51.
Some characteristics from CD may not be favorable for laparoscopic procedures in less experienced hands, as previous abdominal surgeries, incisional hernias, involvement of multiple segments or the penetrating phenotype. However, when feasible, it allows adequate inspection of the abdominal cavity, less morbidity and lower stoma rates34. This makes the laparoscopic approach the best option for most CD patients.
6PREVENTION OF POSTOPERATIVE RECURRENCE IN CDEndoscopic findings after ileocolic resection are good predictors of CD recurrence and precede clinical symptoms52. Before the introduction of more effective therapeutic regimens, endoscopic recurrence rates were described to be as high as 90% with a high prevalence of the need for reoperation in the long-term53,54. There are clear limitations with the use of conventional therapy in prevention of endoscopic recurrence in CD. Hanauer et al. showed no differences in prevention of postoperative recurrence when comparing mesalazine, 6-mercaptopurine or placebo55. A large multicentric study showed benefits with 6-maercaptopurine only in smokers, and the role of thiopurines in preventing recurrence is questionable, despite some published evidence56.
Anti TNF agents are considered to be more effective than conventional therapy in prevention of postoperative recurrence in CD and their use in postoperative period has the potential benefit of a better disease control. Biologic therapy appears to be more efficient in prevention of endoscopic recurrence as compared to conventional therapy in two prospective trials despite short follow-up and low number of patients57,58. A systematic review with meta-analysis also demonstrated the higher efficacy of anti-TNF agents in preventing endoscopic recurrence59. The PREVENT trial was the largest prospective study to date to compare recurrence between patients with infliximab and conventional therapy with infusions of placebo. Despite not achieving the primary endpoint (clinical recurrence), the rates of endoscopic recurrence after 76 weeks were lower in the infliximab group as compared to placebo60.
The choice for optimal therapeutic regimen after surgery must take into account many aspects of the disease such as: the presence of residual disease after ileocolic resection, the use of anti TNF agents before surgery and the presence of different risk factors for recurrence such as smoking and perianal disease. Kotze et al., suggested an individual approach considering the heterogeneity of the presentations and various aspects associated with high or low risk including patient's characteristics, phenotype and histological findings. The choice of the best treatment needs to be individualized and tailored in a case-by-case analysis61.
7FINAL MESSAGESAs seen in this descriptive review, several aspects including patients’ past and present features are important in making the right decision in the surgical management of CD. Adequate preparation of the nutritional status, optimization of medical therapy and anatomic mapping of the small bowel and colon with imaging tests are essential for the best timing of surgery in abdominal resections in CD patients. This fact demonstrates the specific need for a multidisciplinary team in the management of these patients, what impacts the postoperative outcomes with better results.
Adequate surgical technique is important, but does not represent everything in achieving success in major abdominal surgery in CD. Some aspects as the correction of anemia and adequate prevention of thromboembolic events are usually neglected, and need to be emphasized in the multidisciplinary approach that these patients need.
The journey of a surgical CD patient initiates in the gastroenterologist's clinics, passes through the operation itself, postoperative period and does not have an end. As the disease does not have a cure, many efforts in preserving bowel and avoiding intestinal failure and optimization strategies aiming prevention of recurrence are needed. Each patient needs to be seen as a different one, and the therapeutic strategies need to be individualized. The role of the surgeon in a multidisciplinary IBD team is essential for adequate patient care.
8Author's DisclousureClaudio Coy has no disclosures.
Paulo Kotze is a speaker and consultant for Abbvie, Janssen, Takeda and Pfizer.