We aimed to evaluate the characteristics of patients with incidental kidney tumors detected in the pathological examination performed after simple nephrectomy due to a non-functioning kidney.
Patients and methodsThe pathology results of nephrectomy specimens from patients who underwent simple nephrectomy with the diagnosis of non-functioning kidney between January 2012 and March 2021 were retrospectively analyzed. Data regarding demographic information, imaging methods, and clinical and histopathological features of the patients were collected. The number of patients with incidental renal tumors was determined.
ResultsA total of 163 patients with nonfunctioning kidneys who underwent simple nephrectomy between January 2012 and March 2021 were included in the study. Sixty-nine (42.3%) patients were male and 94 (57.7%) patients were female. The most common complaint was flank pain (60.7%). The cause of the nonfunctioning kidney was urinary stones in 116 (71.2%) patients and ureteropelvic/ureterovesical junction stenosis in 21 (10.1%) patients. Incidental renal tumors were detected in 21 (12.9%) patients. Papillary adenoma was the most common renal tumor and was detected in 11 patients. Four patients had renal cell carcinoma and 4 patients had urothelial cell carcinoma (UCC). Three of the patients with UCC had high grade invasive UCC with squamous differentiation and 1 patient had low grade papillary UCC.
ConclusionIn non-functioning kidneys, kidney tumors may be overlooked due to radiological and clinical diagnostic difficulties. Therefore, careful macroscopic and microscopic histopathological evaluation is necessary to detect incidental renal tumors.
Nuestro objetivo fue evaluar las características de los pacientes con tumores renales incidentales detectados en el examen patológico realizado tras nefrectomía simple por riñón no funcionante.
Pacientes y métodosSe analizaron retrospectivamente los resultados anatomopatológicos de las muestras de nefrectomía de pacientes sometidos a nefrectomía simple con diagnóstico de riñón no funcionante entre enero de 2012 y marzo de 2021. Se recopilaron datos sobre información demográfica, métodos de imagen y características clínicas e histopatológicas de los pacientes. Se determinó el número de pacientes con tumores renales incidentales.
ResultadosSe incluyeron en el estudio un total de 163 pacientes con riñones no funcionantes sometidos a nefrectomía simple entre enero de 2012 y marzo de 2021. Sesenta y nueve (42,3%) pacientes eran hombres y 94 (57,7%) pacientes eran mujeres. La queja más común fue el dolor en el flanco (60,7%). La causa del riñón no funcional fueron cálculos urinarios en 116 (71,2%) pacientes y estenosis de la unión ureteropélvica/ureterovesical en 21 (10,1%) pacientes. Se detectaron tumores renales incidentales en 21 (12,9%) pacientes. El adenoma papilar fue el tumor renal más común y se detectó en 11 pacientes. Cuatro pacientes tenían carcinoma de células renales y 4 pacientes tenían carcinoma de células uroteliales (CCU). Tres de los pacientes con ccu tenían CCU invasivo de alto grado con diferenciación escamosa y 1 paciente tenía ccu papilar de bajo grado.
ConclusiónEn riñones no funcionantes, los tumores renales pueden pasar desapercibidos debido a dificultades de diagnóstico clínico y radiológico. Por lo tanto, es necesaria una evaluación histopatológica macroscópica y microscópica cuidadosa para detectar tumores renales incidentales.
The non-functioning kidney is diagnosed based on clinical and radiological findings. Several criteria are utilized to define non-functional kidneys, including paper-thin renal parenchyma (renal parenchymal thickness<5mm) on urinary ultrasound or computed tomography, non-visualization of collecting duct system on intravenous pyelography (IVP), an exhibition of less than 10% renal function in dimercaptosuccinic acid scan (DMSA) and a glomerular filtration rate of <10mL/min/1.73m2 in the affected kidney determined by nuclear renography1. In the etiology of non-functioning kidneys, there are many causes such as adult polycystic kidney disease, acquired cystic kidney disease, unsuccessful transplantation, urolithiasis, chronic pyelonephritis and end-stage kidney disease due to other causes (diabetes, hypertension, etc.)2.
Surgical intervention is not always necessary for a non-functioning kidney. A simple nephrectomy is usually performed in symptomatic patients with chronic infection, pyelonephritis, or obstruction. Despite its name, a simple nephrectomy can be challenging due to widespread inflammation and scar tissue, potentially making it more difficult than radical nephrectomy. The advancement of minimally invasive surgical techniques has introduced simple laparoscopic nephrectomy as a viable alternative to open nephrectomy3. Histopathological examination of non-functioning kidneys reveals various findings depending on the underlying etiology. These may include inflammation, glomerular sclerosis, tubular atrophy, thyroidization, nephrocalcinosis, chronic pyelonephritis, xanthogranulomatous pyelonephritis (XP), dysplastic tubules, and cystic structures1,2.
There are several case reports in the literature about incidentally detected tumors of non-functioning kidneys4,5. The preoperative diagnosis of renal lesions in non-functioning kidneys with conditions such as chronic pyelonephritis, XP, and obstructing renal stones can be challenging using imaging modalities. In such cases, the diagnosis is often made through pathological examination. However, only a limited number of studies that investigate incidentally detected renal tumors following a simple nephrectomy exist.
The objective of this study was to assess the characteristics of patients who had incidental kidney tumors identified during pathological examination following a simple nephrectomy for a non-functioning kidney. Additionally, we conducted a retrospective review of the histopathological features of these patients and documented the common findings.
Material and methodsPatient dataPatients who underwent simple nephrectomy with the diagnosis of a non-functioning kidney between January 2012 and March 2021 were included in the study. The pathology reports of all the cases were reviewed, and the histopathological features and the histological types of the cases with kidney tumors were documented. Patients with a significant renal function (split renal function>15%) or a suspicious lesion diagnosed preoperatively with computed tomography (CT) or magnetic resonance imaging (MRI) and patients<18 years old were excluded from the study.
The diagnosis of a non-functioning kidney in this study was established using DMSA. Those with split renal function less than 10% were considered non-functioning. In patients with a split renal function between 10-15%, if there was a diffuse decrease in the renal parenchymal thickness (<5mm), diffuse inflammation and scarring on CT or MRI, the kidney was considered non-functioning and simple nephrectomy was performed. This retrospective study was approved by the Medical Ethics Committee of our University (Approval No: 2021-7228).
Statistical analysisDescriptive statistics were used to summarize the data, and the frequencies with percentages were reported for categorical variables. SPSS (IBM Corp. Released 2019. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp) software was used for data analysis.
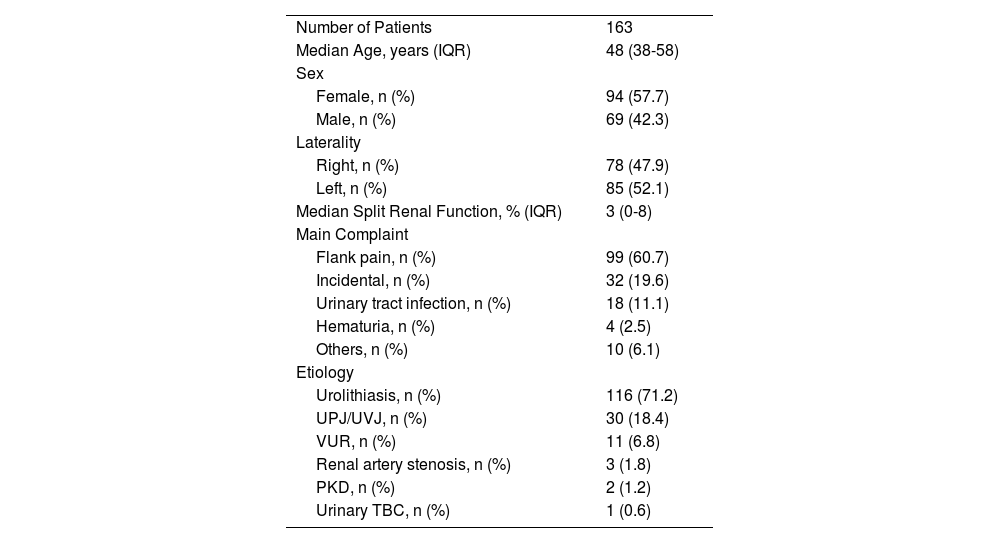
ResultsA total of 163 patients with non-functioning kidneys who underwent simple nephrectomy between January 2012 and March 2021 were included in the study. Demographic data and clinical features are given in Table 1Table 1. The median age of the patients was 48 (38-58) years. Sixty-nine (42.3%) patients were male and 94 (57.7%) patients were female. The most common complaint was flank pain and it was reported by 99 (60.7%) patients. Non-functioning kidneys were incidentally detected in 32 (19.6%) patients. Recurrent urinary tract infections and hematuria were reported by 18 (11.1%) and 4 (2.5%) patients, respectively. The other 10 patients had various complaints like abdominal swelling, urinary incontinence, nausea, and vomiting.
Demographic data and clinical features.
| Number of Patients | 163 |
| Median Age, years (IQR) | 48 (38-58) |
| Sex | |
| Female, n (%) | 94 (57.7) |
| Male, n (%) | 69 (42.3) |
| Laterality | |
| Right, n (%) | 78 (47.9) |
| Left, n (%) | 85 (52.1) |
| Median Split Renal Function, % (IQR) | 3 (0-8) |
| Main Complaint | |
| Flank pain, n (%) | 99 (60.7) |
| Incidental, n (%) | 32 (19.6) |
| Urinary tract infection, n (%) | 18 (11.1) |
| Hematuria, n (%) | 4 (2.5) |
| Others, n (%) | 10 (6.1) |
| Etiology | |
| Urolithiasis, n (%) | 116 (71.2) |
| UPJ/UVJ, n (%) | 30 (18.4) |
| VUR, n (%) | 11 (6.8) |
| Renal artery stenosis, n (%) | 3 (1.8) |
| PKD, n (%) | 2 (1.2) |
| Urinary TBC, n (%) | 1 (0.6) |
IQR: Interquartile range, UPJ: Ureteropelvic Junction, UVJ: Ureterovesical Junction, VUR: Vesicoureteral Reflux, PKD: Polycystic Kidney Disease, TBC: Tuberculosis.
The main cause of non-functioning kidneys was urinary stones, affecting 116 (71.2%) patients, followed by ureteropelvic/ureterovesical junction (UPJ/UVJ) stenosis in 30 (18.4%) cases and vesicoureteral reflux (VUR) in 11 (6.8%) patients.
All patients underwent urinary ultrasonography preoperatively. Additionally, 100 patients had non-contrast CT, 45 patients had contrast-enhanced CT, 8 patients had CT-urography, 1 patient had a non-contrast MRI, 4 patients had contrast-enhanced MRI, 2 patients had MRI-urography and 3 patients had intravenous pyelography (IVP) before the operation.
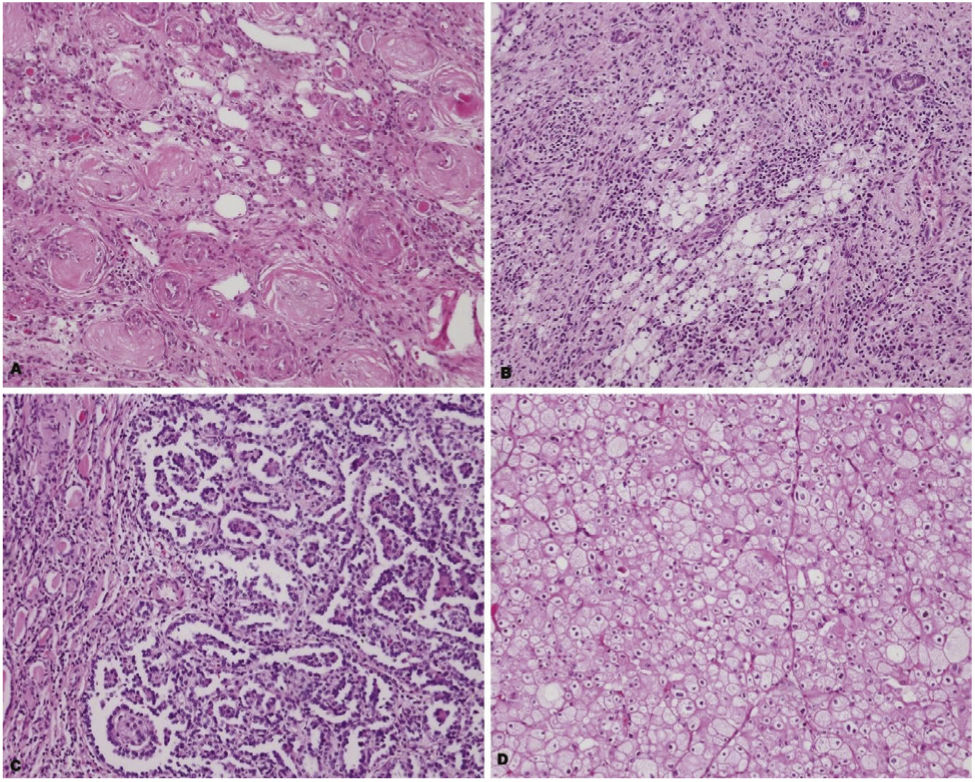
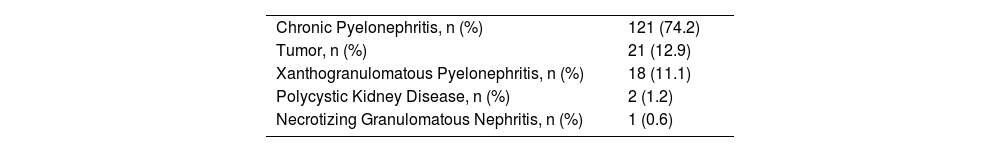
After pathological examination of nephrectomy specimens, chronic pyelonephritis was detected in 121 (74.2%) patients, tumors in 21 (12.9%) patients, XP in 18 (11.1%) patients, polycystic kidneys in 2 (1.2%) patients and necrotizing granulomatous pyelonephritis was detected in 1 (0.6%) patient (Figure 1Figure 1, Table 2Table 2).
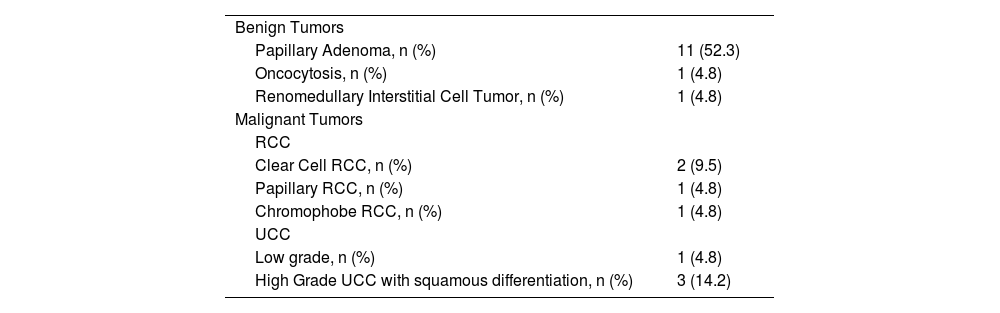
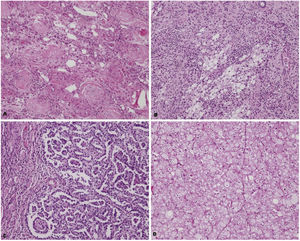
Of the tumors detected histopathologically, 13 (61.9%) were benign and 8 (38.1%) were malignant (Table 3Table 3). In patients with tumors, 20 patients had chronic pyelonephritis and one patient had xanthogranulomatous pyelonephritis. The most commonly observed benign tumor was papillary adenoma. Four patients were diagnosed with renal cell carcinoma (RCC), and another four patients with urothelial cell carcinoma (UCC). Among the UCC cases, three had high-grade invasive UCC with squamous differentiation, and one had low-grade papillary UCC (Table 3). The median tumor size of the malignant tumors was 8.25 (4.5-9.5) cm. In patients with malignant tumors (n=8), the most common preoperative complaint was flank pain and it was reported by 4 patients (50%). One (12.5%) patient had hematuria and 3 (37.5%) patients had no complaints. Further details regarding the characteristics of patients with malignant tumors are shown in Table 4Table 4.
Classification of tumors (n=21).
| Benign Tumors | |
| Papillary Adenoma, n (%) | 11 (52.3) |
| Oncocytosis, n (%) | 1 (4.8) |
| Renomedullary Interstitial Cell Tumor, n (%) | 1 (4.8) |
| Malignant Tumors | |
| RCC | |
| Clear Cell RCC, n (%) | 2 (9.5) |
| Papillary RCC, n (%) | 1 (4.8) |
| Chromophobe RCC, n (%) | 1 (4.8) |
| UCC | |
| Low grade, n (%) | 1 (4.8) |
| High Grade UCC with squamous differentiation, n (%) | 3 (14.2) |
RCC: Renal Cell Cancer; UCC: Urothelial Cell Carcinoma.
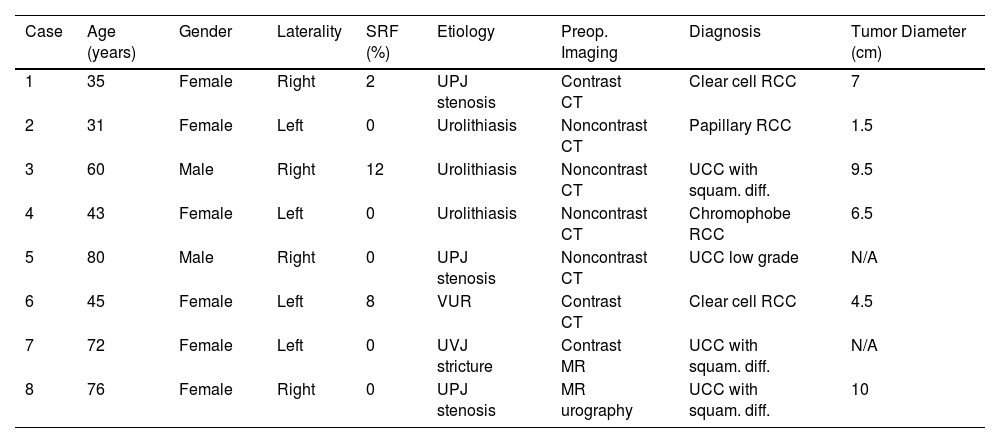
Characteristics of the patients with malignant tumors (n=8).
| Case | Age (years) | Gender | Laterality | SRF (%) | Etiology | Preop. Imaging | Diagnosis | Tumor Diameter (cm) |
|---|---|---|---|---|---|---|---|---|
| 1 | 35 | Female | Right | 2 | UPJ stenosis | Contrast CT | Clear cell RCC | 7 |
| 2 | 31 | Female | Left | 0 | Urolithiasis | Noncontrast CT | Papillary RCC | 1.5 |
| 3 | 60 | Male | Right | 12 | Urolithiasis | Noncontrast CT | UCC with squam. diff. | 9.5 |
| 4 | 43 | Female | Left | 0 | Urolithiasis | Noncontrast CT | Chromophobe RCC | 6.5 |
| 5 | 80 | Male | Right | 0 | UPJ stenosis | Noncontrast CT | UCC low grade | N/A |
| 6 | 45 | Female | Left | 8 | VUR | Contrast CT | Clear cell RCC | 4.5 |
| 7 | 72 | Female | Left | 0 | UVJ stricture | Contrast MR | UCC with squam. diff. | N/A |
| 8 | 76 | Female | Right | 0 | UPJ stenosis | MR urography | UCC with squam. diff. | 10 |
SRF: Split renal function, Preop: Preoperative, RCC: Renal Cell Cancer, TCC: Transitional Cell Cancer, squam.: Squamous, diff.: Differentiation.
Thanks to the advances in radiological imaging methods, the diagnosis of kidney tumors has become easier with imaging modalities like ultrasonography, CT, or MRI in individuals with normally functioning kidneys. However, renal tumors can be missed in patients with non-functioning kidneys especially in those with severe inflammation, scarring, and urolithiasis. These situations may obscure the presence of a malignant tumor. Simple nephrectomy is the surgical removal of the kidney through Gerota's fascia and is performed in patients with benign diseases of the kidney. Radical nephrectomy is the removal of the kidney with Gerota's fascia and is performed in malignant diseases of the kidney6.
Although it is rare, a kidney tumor may be detected after pathological examination of the specimen in patients who underwent simple nephrectomy. There is limited data available in the literature regarding this topic. Zengin et al. conducted a study involving 97 patients who underwent simple nephrectomy for non-functioning kidneys caused by urolithiasis and reported that in 9 (9.3%) patients, a malignant tumor was detected in pathological examination1. This rate is almost twice the rate of what we detected. Among these 9 patients, 3 had UCC, 3 had RCC (1 sarcomatoid, 1 papillary, and 1 clear cell), 2 had squamous cell cancer (SCC) and 1 patient had both RCC and UCC. In their series, the most common pathological diagnosis, similar to our study, was chronic pyelonephritis (in 79 patients), followed by XP in 9 patients. They also reported that papillary adenoma was detected in 2 patients with chronic pyelonephritis. The rate of papillary adenoma in our series was higher. They made no comment about the type of preoperative imaging method they used1. Lin et al. evaluated the incidence of RCC in non-functioning kidneys in their study2. They analyzed 311 nephrectomy specimens obtained from 279 patients with non-functioning kidneys. They found that 73 (23.5%) nephrectomy specimens had RCC and most of these cases had acquired cystic kidney disease or end-stage renal disease. Clear cell RCC was the most common subtype followed by papillary RCC. However, the type of nephrectomy (simple or radical) was not specified in their study, and it included patients who had a preoperative diagnosis of RCC. Additionally, the study did not provide information on other types of renal tumors apart from RCC. Angerri et al. performed simple laparoscopic nephrectomy on 96 patients with urolithiasis and split renal function<15%3. They detected SCC in 1 (1.04%) patient. In our study, we detected renal tumors in 21 (12.9%) patients and 8 (4.9%) were malignant in the whole group. The number of patients who developed a non-functioning kidney due to urolithiasis was 116; in 3 (2.6%) of these patients, malignant tumors were detected through histopathological evaluation. This rate is lower than the value reported by Zengin et al. In the study conducted by Yeh et al., 47 patients with non-functioning kidneys due to urolithiasis who underwent nephrectomy were evaluated7. They detected renal tumors in 24 patients. In 7 of these patients, tumors were detected preoperatively therefore the detection rate of incidental tumors was 36.2%. This is still a very high rate. They speculated that the inadequacy of USG, IVP and retrograde pyelography in detecting malignant lesions may have led to this result and they recommended performing an MRI before the operation in these patients. It is worth noting that the study by Yeh et al. is from 2007, and advancements in imaging techniques and protocols have since been made. These advancements may have improved the detection of malignancies in non-functioning kidneys.
The median tumor size of the malignant tumors in our study was 8.25cm (4.5-9.5cm), which is a significant size. Despite this size, there are several reasons why these tumors cannot be detected in preoperative evaluations. Especially in cases with underlying stone disease and recurrent urinary infections, inflammatory and fibrotic changes in the kidney parenchyma may prevent the detection of the tumor. In cases with UPJ/UVJ stenosis, severe hydronephrosis of the kidney may mask cystic lesions. In our study, 4 (50%) of the patients with malignant lesions were evaluated with non-contrast CT before the operation. Non-contrast CT is mainly used for the evaluation of urinary stone disease and it is insufficient for malignancy evaluation. Two patients with malignant lesions were evaluated with contrast-enhanced CT, 1 patient was evaluated with contrast-enhanced MRI, and 1 patient was evaluated with MRI urography. Different radiological imaging methods were used during the evaluation of these patients with nonfunctioning kidneys depending on the underlying condition. Some of the patients were admitted to emergency service with acute complaints such as flank pain and fever so CT was the preferred imaging method. For patients with normal kidney function contrast-enhanced CT was performed. In patients with a GFR<60, we do not use contrast-enhanced CT in our institute so these patients were evaluated with non-contrast CT. Also in patients with coexisting kidney stones non-contrast CT was used. In patients with UPJ or UVJ obstruction, MRI or CT urography was used depending on the GFR value. In cases with solid renal masses, the most important factor for differentiating malignant lesions from benign ones is the presence of contrast enhancement8. We believe that contrast-enhanced imaging should be recommended to all patients with non-functioning kidneys before simple nephrectomy to minimize the risk of not diagnosing a malignancy. However, it should be kept in mind that even with contrast-enhanced CT and MRI, a concomitant malignant tumor may not be detected in these patients, since the blood flow to the kidney may be impaired in non-functioning kidneys. If a contrast-enhanced examination cannot be performed for any reason (kidney failure, allergy, etc.), a non-contrast MRI should be preferred instead of a non-contrast CT.
Zengin et al. and Lin et al. did not provide information about the preoperative complaints of the patients. However, Yeh et al. reported that the most common preoperative complaints were flank pain and gross hematuria. In the case series of Jain et al., all patients presented with flank pain. The presenting complaint may also be related to the etiology of the non-functioning kidney (urolithiasis, ureteropelvic junction stenosis). There is no specific symptom that is associated with a specific tumor and malignant tumors can be detected in patients without any complaints.
SCC of the kidney is a rare renal neoplasm and it constitutes about 0.8% of renal malignancies9. Most of the information on renal SCC is obtained from case reports10–12. It is believed that renal SCC is closely related to kidney stones, chronic infection, and inflammation13. Jain et al. reported a case series of 4 patients with renal SCC who had staghorn calculi and non-functioning kidneys4. In three of these cases, the diagnosis was established by postoperative pathological examination; there was no evidence of malignancy on preoperative radiological evaluation. Since SCC metastases to the kidney may also occur, it is essential to show the transition from squamous metaplasia areas to the tumor to support the primary diagnosis. In our study, we did not have a case with a diagnosis of squamous cell carcinoma after a simple nephrectomy. However, we had a urothelial carcinoma case with an extensive squamous differentiation in a patient with urolithiasis and 2 cases of UCC with squamous differentiation in patients with ureteropelvic/ureterovesical junction stenosis.
There is no specific follow-up protocol defined for patients with malignant tumors detected after simple nephrectomy. We considered these patients at high risk for recurrence or metastasis and followed them closely, similar to patients who underwent radical nephrectomy, with frequent contrast-enhanced CT or MRI.
A papillary adenoma is an unencapsulated small-sized tumor with papillary or tubular architecture and low nuclear grade14. They are associated with papillary RCC and the most important distinguishing factor is their size (≤15mm)15. Due to their small size, they are not usually detected by imaging methods and are most commonly found incidentally in nephrectomy specimens. Caliò et al. reported the incidence of papillary adenoma as 19% in their autopsy study16. This incidence increased to 25% in cases>40 years old. Wang et al. evaluated 542 consecutive nephrectomy specimens and detected papillary adenomas in 38 (7%) patients17.
Papillary adenoma was the most common incidental tumoral lesion in our series (6.7%), a rate similar to that reported by Wang et al. The high incidence of papillary adenoma in the study by Caliò et al. may be attributed to the fact that it was an autopsy study16.
The most common histopathological diagnoses in nephrectomies performed for non-functioning kidneys are chronic pyelonephritis, XP, polycystic kidney, and granulomatous pyelonephritis3,18,19. In our study, chronic pyelonephritis was found in 71.1% and XP in 9.6%, which is consistent with the literature. Tuberculosis is a granulomatous disease and it is more commonly observed in developing and low-income countries20. Tuberculosis may affect the entire urinary system and the kidneys are the most frequently affected urogenital organs21,22. We also had a diagnosis of granulomatous pyelonephritis in one of our cases, and the case was being followed up for tuberculosis.
LimitationsThis study has several limitations. It is a retrospective study with a limited number of patients. The radiological imaging methods were reviewed by different radiologists which might affect the preoperative diagnosis of suspicious lesions.
ConclusionIn non-functioning kidneys, tumors may be overlooked due to radiological and clinical diagnostic difficulties. The possibility of detecting a tumor in histopathological examination after simple nephrectomy is low and most of these tumors are benign. However, rarely, malignant lesions like RCC and UCC can be missed preoperatively by imaging methods in some patients with non-functioning kidneys and detected after the pathological examination. Therefore, the possible presence of a concomitant tumor should be considered when evaluating non-functioning kidneys, and macroscopic and microscopic examinations should be done carefully.
Funding sourcesAuthors have not received any funding for this research.
Conflicts of interestAll authors declare that they have no conflicts of interest.
Ethical approvalThe study was approved by the Ethics Committee of Bezmialem Vakif University with the approval number (2021-7228).
Author ContributionsStudy conception and design: GÇ, BCT, NŞ. Acquisition of data: GÇ, BCT, HT, AI and PY. Analysis and interpretation of data: GÇ, OT. Drafting of the manuscript: GÇ, OT Critical revision: GÇ, PY, NŞ, HT.