Total Skin Electron Beam Therapy (TSEBT) is a technique used in the treatment of superficial skin diseases, such as cutaneous lymphomas. Although it has demonstrated its effectiveness through several clinical studies of the advanced stages of mycosis fungoides, it is not available in most cancer centers in Mexico, because it requires large electron fields in order to cover the entire body.
ObjectiveIn order to obtain large electron fields for TSEBT, conventional treatment distances are not sufficient. This has led to the need for an electron beam with special features and calibration at a distance of 500cm or more, as well as the need to create a treatment protocol to develop the TSEBT programs in Mexico.
Materials and methodsThe ELEKTA SYNERGY Linear Accelerator was selected with a 6 MeV energy at a Source Skin Distance (SSD) of 500cm, in high dose rate mode (1,000 MU=100Gy), using a cone of 40×40cm2 and the gantry angled to 90°, obtaining a large electron field of 200×100cm2 useful area. Routine calibration was performed at a Zref=1.40cm and an SSD of 100cm with a 40×40cm2 cone using a plane-parallel ionization chamber and electrometer (Scandotronix Wellhofer model PPC05 FOCUS) and a water phantom. The same procedure for the absolute dose rate determination was also performed in treatment conditions (500cm). For the beam characterization in terms of Percentage Depth Dose (PDD) and beam profiles, Radiochromic Gafchromic® EBT2 film (RCF) was used, after being calibrated for electrons in a solid water phantom (Scanditronix Wellhöfer) at a 1.4cm depth and Source Axis Distance (SAD) of 100cm and 500cm, in order to acquire the equation relating the dose response with optical density. PDD was obtained at 0, 1, 1.2, 1.4, 1.5, 2, 3, 4, 5, 6, 7, 8 and 9cm depths in the phantom. Spatial dose distribution was obtained by placing 3×3cm2 samples of RCF on an acrylic screen situated in front of the patient (for the purpose of obtaining maximum absorbed dose on the skin). Lastly, a treatment protocol was proposed.
ResultsAn effective maximum dose depth (Zref) for electrons of 1.4±0.05cm was obtained according to the relative spatial dose distribution and the percentage depth dose for a SSD of 500±0.5cm, over an area of 200×100cm2. Horizontal and vertical beam profiles were plotted, showing a horizontal symmetry of ±0.35%, horizontal flatness of ±3.62%, vertical symmetry of ±2.1%, and vertical flatness of ±14.2%.
ConclusionsThe resulting horizontal and vertical profiles enabled the electron beam symmetry and flatness to be assessed. PDD was analyzed up to a 9±0.05cm, establishing the electron depth penetration to ensure treatment of the skin surface.
La terapia total de piel con haz de electrones (TSEBT) es una técnica usada en el tratamiento de enfermedades superficiales de piel tales como linfomas cutáneos. Aunque su efectividad ha sido demostrada a través de varios estudios clínicos en estadios avanzados de la micosis fungoide, no es una técnica disponible en muchos centros de cáncer en México debido a que se requieren campos grandes de electrones para cubrir un cuerpo entero.
ObjetivoPara obtener campos grandes de electrones para TSEBT, las distancias convencionales de tratamiento no son suficientes. Esto trae la necesidad de una caracterización y calibración especial del haz de electrones a distancias de 500cm o más y la necesidad de crear un protocolo de tratamiento para TSEBT en nuestro país.
Materiales y métodosPara la puesta en marcha de esta técnica fue seleccionado el acelerador lineal ELEKTA SYNERGY, con una energía de 6 MeV a una distancia fuente-superficie (SSD) de 500cm, en modo de alta tasa de dosis (1,000 UM = 100Gy), usando un cono aplicador de 40 × 40cm2 y el ángulo de gantry de 90°, obteniendo un campo grande de electrones de 200 × 100cm2 (área útil). La calibración de rutina fue realizada a una profundidad de referencia (Zref) de 1.4cm a una SSD de 100cm y un cono aplicador de 40 × 40cm2 usando una cámara de ionización de placas plano-paralelas y un electrómetro (Scandotronix Wellhofer modelo PPC05 FOCUS) y un maniquí de agua. El mismo procedimiento fue realizado para determinar la tasa de dosis absoluta en condiciones de tratamiento (500cm). Para la caracterización del haz de electrones en términos de porcentaje de dosis a profundidad (PDD) y perfiles de dosis, se utilizó Película Radiocrómica Gafchromic EBT2 (PRC), después de ser calibrada para electrones en un maniquí de agua sólida (Scandotronix Wellhofer) a un Zref = 1.4cm de profundidad a una Distancia Fuente Isocentro SAD de 100cm y de 500cm, para obtener la ecuación de la dosis en respuesta de la densidad óptica. La PDD fue obtenida a 0, 1, 1.2, 1.4, 1.5, 2, 3, 4, 5, 6, 7, 8 y 9cm de profundidad en el maniquí. La distribución espacial de dosis fue obtenida colocando muestras de PRC de 3 × 3cm2 sobre la pantalla de acrílico que será situada enfrente del paciente (para así obtener la dosis absorbida máxima en piel). Por último, fue propuesto un protocolo de tratamiento.
ResultadosLa profundidad de dosis máxima (Zref) para electrones fue de 1.4 ± 0.05cm, de acuerdo con la distribución de dosis espacial relativa y el porcentaje de dosis en profundidad para una SSD de 500 ± 0.5cm, sobre un área de 200 × 100cm2. Se graficaron los perfiles del haz tanto horizontal como vertical, mostrando una simetría horizontal de ±0.35%, aplanado horizontal de ±3.62%, simetría vertical de ±2.1% y aplanado vertical de ±14.2%.
ConclusionesLos resultados de los perfiles horizontal y vertical permiten evaluar la simetría y aplanado del haz de electrones. El PDD fue analizado hasta 9 ± 0.05cm, estableciendo la profundidad de penetración de los electrones, asegurando un tratamiento superficial a la piel.
Cutaneous T-cell lymphoma represents a complex array of disorders with different clinical courses and therapeutic considerations. Mycosis fungoides which affects the skin in flat patches, thin plaques, or tumors is the most common form of cutaneous T- cell lymphoma1; consequently, more is understood about its diagnosis, treatment and prognosis. The chronicity of the disease results in many patients being treat with multiple therapies in their lifetime, including skin directed therapies, such as ultraviolet light, topical and radiation. Total skin electron beam therapy (TSEBT) involves treating the entire skin surface using electron beams. The low – energy electrons generated by a linear accelerator penetrate only the skin, sparing deeper tissues and organs, ensuring a safe treatment. It has complete response rate of 80–97%. It can be employed as initial therapy in the presence of thick lesions for presenting greater therapeutic effect than topical chemotherapy and phototherapy.
For this technique, large electron fields are required. The objective of this project is to determine the dosimetric parameters, include them in the planning system in order to develop a treatment protocol for mycosis fungoides.
Materials and methodsReviewing the literature there are different methods of obtaining the very large fields needed for electron beam irradiation of the total skin. Several recommendations are made regarding the types of dosimetric measurements that should be performed prior to initiating such irradiation procedures. One widely used technique for TSEBT, which involves six dual fields, known at the Stanford protocol.
According to the IAEA TRS 398 Calibration Protocol2, a ELEKTA SYNERGY Linear accelerator was calibrated, at a Zref=1.40cm and a SSD of 100cm with a 40×40cm2 field size using a plane-parallel ionisation chamber and electrometer (Scanditronix Wellhofer model PPC05 FOCUS), and a water phantom. A 6 MeV energy was used at a high dose rate of one Monitor Unit (MU) equivalent to 10 cGy.
Radiocromic film (RCF) develops itself when exposed to ionizing radiation due to the polymerization process that takes place on its surface. It is made from polydiacetylene and it is basically composed by hydrogen, carbon, nitrogen, oxygen, lithium, chlorine and sodium. Its effective atomic number is very similar to the one of water. Radiation causes an increase in the number of polymers formed, which causes a film's optical density to increase. It has many advantages therefore it is used widely for medical purposes, including its high spatial resolution, two dimensional dosimetry, minimal thickness and permanent registry. The RCF opacity can be quantified by a light transmission factor and its measure is the optical density (OD). This characteristic can be measured by a spectrophotometer or a flatbed scanner. It is defined by the equation:
Where, I0 is the intensity of light incident on a film, I is the intensity transmitted through the film irradiated.
Radiochromic film handling and processingThe commercial Gafchromic EBT2 RCF (measuring 20.3×25.4cm2) was handled according to the manufacturer and the AAPM Task Group 55 recommendations3. It was cut down to segments measuring each 3×3cm2 with a 48hours interval between slicing and the first irradiation in order to avoid any disturbance of its components due to mechanical damage caused by the guillotine. Another 48hours period was considered after irradiation to scan film segments to allow the polymerization process to finish. The film was protected from further irradiation or light exposure and stored under controlled humidity and temperature conditions.
An EPSON EXPRESSION 10000 XL scanners with EPSON SCAN software were used to digitalize the film before and after irradiation. In order to reach stable temperature conditions, the scanner was turned on one hour before use and during scanning each piece was laid at the center of the scanner to avoid uneven lighting. The film edges were covered with a black bind to avoid modifications due to light dispersion.
The film orientation was identified by a mark in the right upper corner during the entire process. Each piece endured four scans to reduce scanner or operator interference and a mean was calculated between the four images obtained. RGB format (red, green and blue) was used for digitalization with 75 points per inch spatial resolution (dpi) and 48 bits of color depth (16 bits per channel). Images were saved in Tagged Image File Format (TIFF) and processed with ImageJ software. Information from the red channel was extracted of the RCF, where the active components express their maximum response.
We determined the regions of interest (ROI) with the ImageJ software. The size of a ROI was determined by the conversion 1 pixel =0.08455mm due to image resolution (Fig. 1).
Analyzing the information from the irradiated and non-irradiated films using the histogram function of the program, we obtained the intensity (I) and the standard deviation (SD). It is recommended the SD did not surpass 3% intensity (Fig. 2)3. Finally, RCF response is obtained using equation 1.
Radiocromic film calibrationIn order to determine the absorbed dose in response to the netOD of the RCF, obtaining the net optical density of the following equation:
Where, ODexp is the optical density of the film exposed to radiation, ODunexp is the optical density of the film not exposed to radiation.
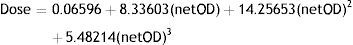
Measures were performed in a 30×30×30cm3 solid water phantom (SCANDITRONIX WELLHOFER model TYPE SP34). The dose at which the film was irradiated cover a range of 0-5Gy each irradiation was of .5Gy. For each value of absorbed dose considered in the calibration curve we used four 3×3cm2 films in order to reduce the statistical uncertainty. Each piece of film was placed at a depth of 1.4cm in solid water which is regarded as the reference depth (Zref) of 6 MeV electrons, with a SSD of 100cm and with a field size of 10×10cm2. Films were then scanned and the images obtained were processed with the ImageJ software, using a ROI of 1×1cm2, obtaining the corresponding optical densities and SD. We plotted the dose – response calibration curve, and a third-degree polynomial adjustment was made to the calibration curve, obtaining the following equation:
Absorbed dose distribution at 500 cmAccording to the AAPM Task Group 55 recommendations RCF of 3×3cm2 were obtained and were adhered to the acrylic screen in such a manner that they would cover a human body surface (screen acrylic dimensions 200×100cm2). The RCF adhered to the screen acrylic were irradiated at a SSD of 500cm to a 1,000 MU with a 40×40cm2 SAD field, with a gantry angle of 90° and a collimator angle of 270°.
Percentage depth doseThe graphic of Percentage Depth Dose was obtained by placing a solid water phantom of 30cm3 to SAD and SSD of 500cm, setting specific distances at which the RCF of 3×3cm2 were placed (0, 1, 1.2, 1.4, 1.5, 2, 3, 4, 5, 6, 7, 8, 9) this was performed under 2 forms; with acrylic screen and acrylic screen without.
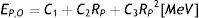
Beam energyThe beam incident on the output window of Linac can be characterized by a distribution of maximum energy called linac's energy. The distribution of beam energy in the surface treatment (phantom surface) is characterized by its maximun or most probable energy Ep,o. The following relationship is used for obtain the most probable energy in the phantom surface Ep,o, in MeV, the range practical, Rp in centimeters of water, it is defined like the depth of the point where the to the descending linear portion of the curve (at the point of inflection) intersects the extrapolated background (bremsstrahlung).
For water, C1=0.22 MeV, C2=1.98 MeV cm−1, and C3=0.0025 MeV cm−2
Results and discussionRadiocromic film calibration to electronsCalibration curve of radiochromic film to electrons is in Figure 3 which shows the behavior of electrons in their relationship dose-netOD and the equation obtained (3). The dose obtained to 500cm SAD with the RCF is verified with ionization chamber plane-parallel resulting in a percentage difference of ± 2% for this reason the RCF can be considered as an optimum dosimeter for electrons.
Absorbed dose distribution and percentage depth dose at 500cmthe absorbed dose distribution at SSD 500cm in an area such as to cover a robust body 200×100cm2 is presented in Figure 4 which shows some heterogeneity in the distribution of absorbed dose at the surface of the acrylic screen according to the symmetry and flatness beam, which will be used like good distribution for TSEBT according to the results of symmetry and flatness of other authors.(Fig. 5)
The percentage depth dose is presented in Figure 6 which compares the PDD with and without acrylic screen, obtained beam's central axis until a depth of 9cm, in this comparison it can assess that acrylic screen is useful to obtain the maximum dose of electrons at 0.4cm depth.
Symmetry and flatnessThe symmetry and flatness of large field at 500cm was calculated following the AAPM recommendations4 (Figs. 7 and 8).
The symmetry and flatness horizontal and vertical of electron large field was calculated from the dose distribution data. The symmetry of 40×40cm2 field at 500cm was: horizontal ±0.35% and vertical ±2.1%, the flatness obtained was: horizontal ±3.62% and vertical ±14.2%. Taking into account the experience of other groups which have reported that at 500cm a vertical uniformity ±8% and horizontal is an achievable purpose to a electrons large field in TSEBT5,6. However, in order to achieve good beam uniformity in the treatment plane (0.4cm depth), the dose uniformity on the patient's surface cannot be better than ±15%, due to the variable SSD, self-shielding and differences in curvatures5,6.
Beam energyThe most probable energy in the phantom surface Epo obtained was 4.4 MeV according to the Rp of 2.1cm such that the acrylic screen working to degrade the energy of 6 MeV to 4.4 MeV while the x-ray contamination by bremmstrahlung interactions was approximately of 5% to 7%.
Treatment protocolSelection of patients- -
Clinical stage: I, II, ECOG: 0-1, KPS>70 7,8.
- -
Hematological profile and blood chemistry within normal parameters.
- -
Pre-treatment with low doses of steroids (prednisone, 25mg daily), antiemetic.
- -
Total body irradiation at 6 positions.
- -
1cm scattering screen.
- -
6 MeV e-.
- -
1Gy/fraction, 4 fractions/week resting Wednesday, Saturday and Sunday to avoid acute skin toxicity (temporary nail loss, anidrosis, epistaxis and parotitis).
- -
Duration of treatment: 9 weeks.
- -
Total absorbed dose: 36Gy.
- -
Place shielding eyes, nails and genitals.
- -
The shield is fabricated from 1.5mm lead is being personalized for each patient by the different anatomical dimensions, is adhered by means of transport (adhesive plaster for clinical use).
- -
Place the PRC in the patient's anatomy (vertex, face, neck, chest, abdomen, back, arms, buttocks, groin, legs, warm, feet, soles) between 2 and 3 RCF 2×2cm2 by anatomical thus making an in vivo dosimetry and perform quality control of the absorbed dose and the dose found in anatomical areas with greater curvature.
- -
Move the patient in a wheelchair to the acrylic screen to prevent any loss of shielding or dosimetry material.
- -
Place the patient as close (stuck) in the acrylic screen anterior which would be the first of the 6 positions according to the Stanford technique.
- -
Throughout the placement time to explain to patients the duration of treatment per day, and how complicated it because of the anatomical positions which will be in the treatment room.
- -
Collect and store the radiochromic films.
- -
The next day, reading radiochromic films, to confirm the absorbed dose delivered so we can proceed with corrections or boost dose when the patient arrives for their next session.
- -
The depth at which 80% of the administered dose is absorbed should not be less than 4mm, to ensure that the epidermis and dermis are within the region of high dose.
- -
At a depth of 20mm the absorbed dose should not exceed 20%, to minimize damage to organs at risk.
- -
Boost irradiation on soles and top of the head (27Gy, 15 fractions of 1.8Gy each).
- -
Other body regions receiving D<80% of the prescribed dose should receive adjuvant treatment, in this case, the technique for each field can vary according to the depth of skin infiltration of the disease. For example, if it is desired to irradiate only the skin surface, complementary fields with lower e- energies of 3-6 MeV can be used.
- -
The total absorbed dose of bremsstrahlung X-ray contamination should not be greater than 0.7Gy.
- -
When there is lymph node involvement, higher electron energies (6-12 MeV) are required.
For patients with advanced stage disease (IVA, IVB), with visceral involvement, total body irradiation with photons should be considered.
- -
For quality control and verification of the treatment dose for body regions receiving less than 80% of the prescribed dose, RCF should be used.
Dosimetry of a large electron field discloses the information necessary to treat the whole body of a patient such as the dose distribution to well know the absorbed dose at the surface of the patient's body, the percentage depth dose to know the depth at which the electrons delivered their maximum dose (0.4cm) and thus assuring the irradiation only to level cutaneous. Absorbed dose distribution at 500cm presents symmetry and flatness within limits reported by other authors and is considered acceptable for a treatment of Total Skin Electron Beam Therapy. The acrylic screen with thickness of 1cm is an effective degrader that allows the electrons deposit their maximum dose to a 0.4cm skin depth. Dosimetric characterization of large field electron allowed to perform a treatment protocol in agreement with the EORTC recommendations9,10.
FundingThis project received financing from the Universidad Autónoma del Estado de México (UAEM) and the Consejo Mexiquense de Ciencia y Tecnología (COMECYT) through scholarships awarded.
Conflict of interestThe authors have no conflicts of interest to declare.
The authors wish to thank the institutions supporting this project: The American British Cowdray Medical Center, Universidad Autónoma del Estado de México (UAEM) and Hospital General de Mexico “Dr. Eduardo Liceaga”.