A 21-year-old patient attended the Orthodontics Clinic of the Division of Postgraduate Studies and Research at the Faculty of Dentistry, UNAM. The main reason for consultation was a crossbite. Upon facial assessment, in the frontal view, a dolichofacial face, a positive smile, hypertonic chin, thick lips, matching dental and facial midlines and lip incompetence were observed. Intraorally she presented mild dental crowding, dental rotations, matching dental midlines, square-shaped arches, bilateral class III molar and canine relationship, posterior cross bite on the left side and an edge to edge bite. Model analysis showed an upper tooth-bone discrepancy of -2mm and in the lower arch, -3.5mm. Overbite was 0mm and overjet, 0mm.
Paciente de 21 años de edad, se presenta a la División de Estudios de Postgrado e Investigación de la Facultad de Odontología de la UNAM. El motivo principal de la consulta es la mordida cruzada. A la revisión clínica extraoral, en la vista frontal se observa una cara dolicofacial, sonrisa positiva, hipertonicidad del mentón, labios gruesos, línea media facial coincide con línea media dental e incompetencia labial. Intraoralmente presenta apiñamiento dental leve, rotaciones dentales, líneas medias dentales coincidentes, arcadas cuadradas y relación molar clase III y canina bilateral, mordida cruzada posterior del lado izquierdo, mordida borde a borde. El análisis de modelos mostró una discrepancia óseo-dentaria superior de (-2mm) e inferior de (-3.5mm). Sobremordida vertical de 0mm y horizontal de 0mm.
Approximately 4 per cent of the population has a dentofacial deformity that requires surgicalorthodontic treatment for its correction. The most common indications for surgical treatment are severe skeletal class IIs and IIIs and skeletal vertical discrepancies, in patients who are no longer in growth.1 Skeletal class III patients are a large proportion of those who are seeking orthodonticsurgical treatment.2 Proffit et al reported that from those patients with orthodontic-surgical treatment, 20% have a mandibular excess, 17% have maxillary hypoplasia and 10% have both. Patients with skeletal class III are more likely to seek a clinical evaluation than skeletal class II patients.3 The majority of people with class III malocclusions have dentoalveolar and skeletal problems and only the minority of cases may be treated only with orthodontics. However patients with severe skeletal class III discrepancies, are often treated with maxillary, mandibular or bimaxillary orthognathic surgery in combination with orthodontic treatment.4 Few studies have examined the factors that influence the choice between conventional orthodontic treatment and orthodontic -surgical treatment. Kerr et al reported that patients with angles ANB of less than -4° and mandibular incisors with inclinations less than 83°, are more likely to have orthodontic-surgical treatment that conventional orthodontic treatment.5
A more recent study concluded that surgical patients could be distinguished from the non-surgical ones based on the WITTS appraisal, the relationship of Maxillary/MandibularLength, the Goniac angle and the Sella-Nasion distance.6 The circumpuberal growth is complete or almost complete in patients with ages around 15 years for girls and 17 years for boys. Although some mandibular growth may occur until the age of 20, in an investigation with more than 300 orthodontists they reported that the earliest ages to start orthognathic surgery treatment, were: 14.9 years for girls and 16.5 years for boys.7,8 Treatment for an adult patient with skeletal class III malocclusion requires dentoalveolar decompensation and combined procedures of orthodontics and surgery, with the purpose of achieving a normal occlusion and improve facial aesthetics.9–12 One of the main objectives of the pre-surgical orthodontic phase is to correct incisor inclinations or bring them within the alveolar bone to allow a maximum surgical correction.13,14 The main objectives of the Orthodontic-surgical treatment are: to normalize the facial profile, correct within a range of normal values the main dentoskeletal parameters and ensure proper occlusion and function.15 When planning a conventional treatment with orthognathic surgery, anteroposterior discrepancies are corrected by maxillae advancement or retrusion along the existing occlusal plane.
When a vertical change of the maxilla is required, the mandible will rotate forward and upwards; as a consequence of this rotation, the mandibular plane angle will be altered. When changes of the occlusal plane are required for aesthetic considerations, the maxilla and the mandible should rotate together according to the newly defined occlusal plane.16 Reykene et al established that when a patient needs a change of the occlusal plane of more than 2°, the situation is significant to be considered as a case of intentional rotation, in a clockwise or counter clockwise direction. This design of treatment is also known as an alteration of the occlusal plane or rotation of the maxillomandibular complex and is indicated frequently in patients who have a low mandibular plane angle (hypodivergent) or a high one (hyperdivergent).17 A clockwise rotation of the maxillomandibular complex, used in the case of patients with hypodivergent growth pattern provides good exposure of the maxillary incisors, an excellent smile arch curvature and the patient's facial balance improves.18
The aim of the article is to present a treatment alternative through orthodontics and orthognathic surgery for a skeletal class III patient due to prognathism.
CASE REPORTA clinical case of a female patient of 21 years is hereby presented, who attended the Orthodontics clinic at the division of Postgraduate Studies and Research of the National Autonomous University of Mexico, with the following reason for consultation: «I have a cross bite». She was considered an apparently healthy patient.
Clinical assessment:
- a)
Frontal aesthetic analysis
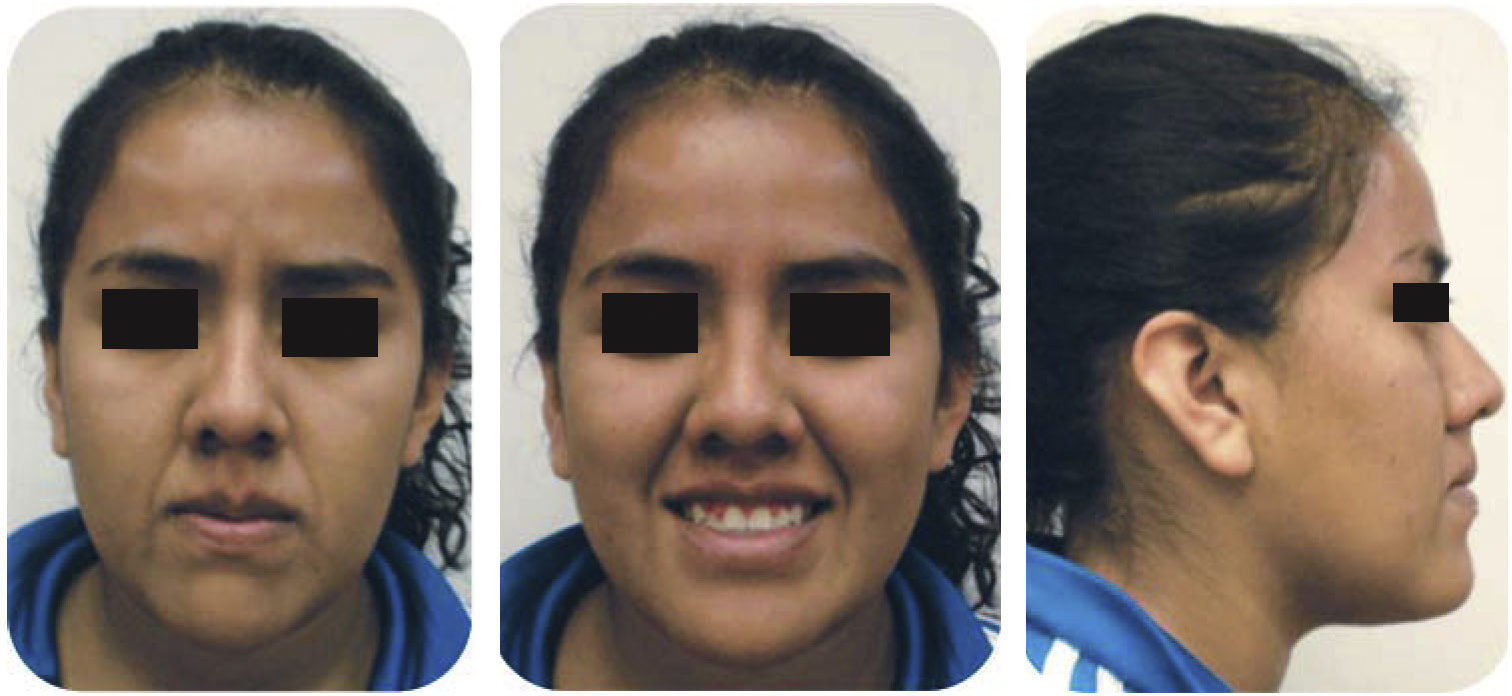
Patient with an oval face, dolichofacial and a positive smile with a 100% display of the clinical crowns. Lower third increased in relation to the middle third; she presented mild facial asymmetry, deficiency of projection of the middle third, chin muscles hypertonicity, thick lips; the facial midline coincided with dental midline and lip incompetence.
- b)
Profile analysis
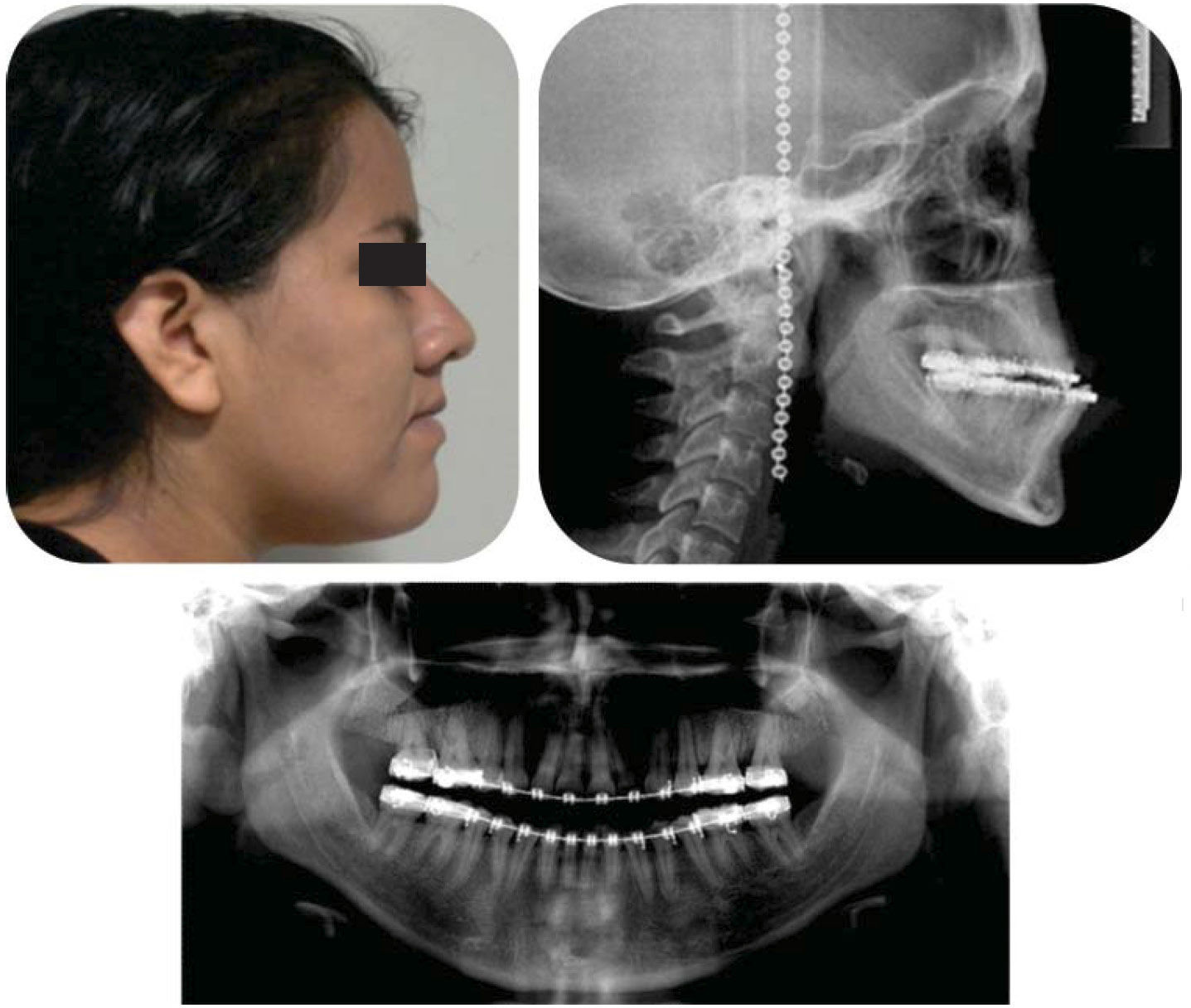
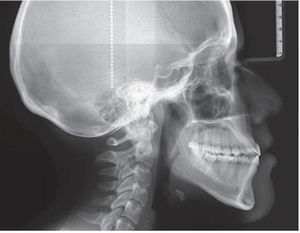
She presented a concave profile, straight nose, lower procheilia, straight nasolabial angle, lip competence and a positive labial step (Figure 1).
- c)
Intraoral characteristics
The patient presented 32 teeth, with mild crowding, rotations, coincident dental midlines, squared arches, class III molar and canine relationships, posterior cross bite on the left side and an edge to edge bite.
Model analysis showed an upper discrepancy of -2mm and in the lower arch, -3.5mm. Overbite was 0mm and overjet, 0mm (Figure 2).
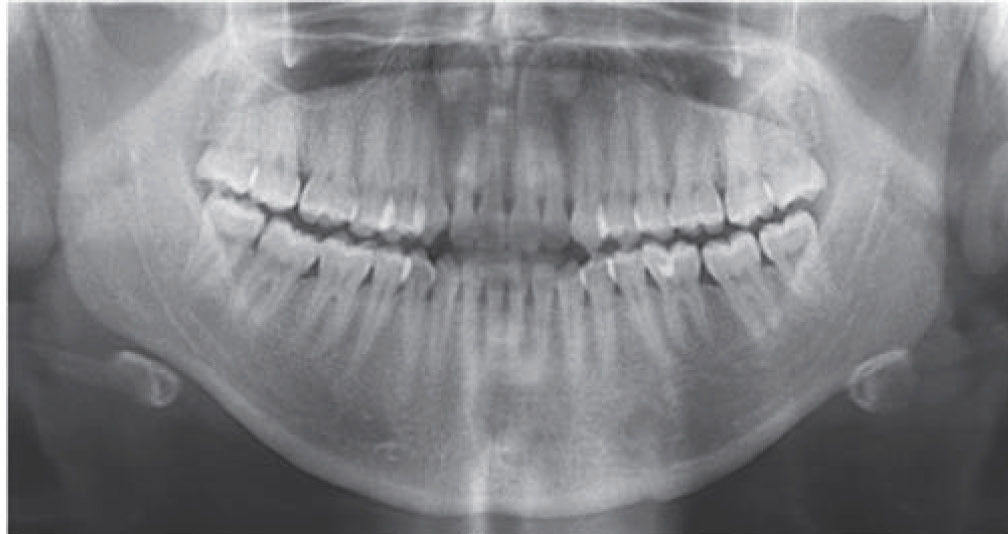
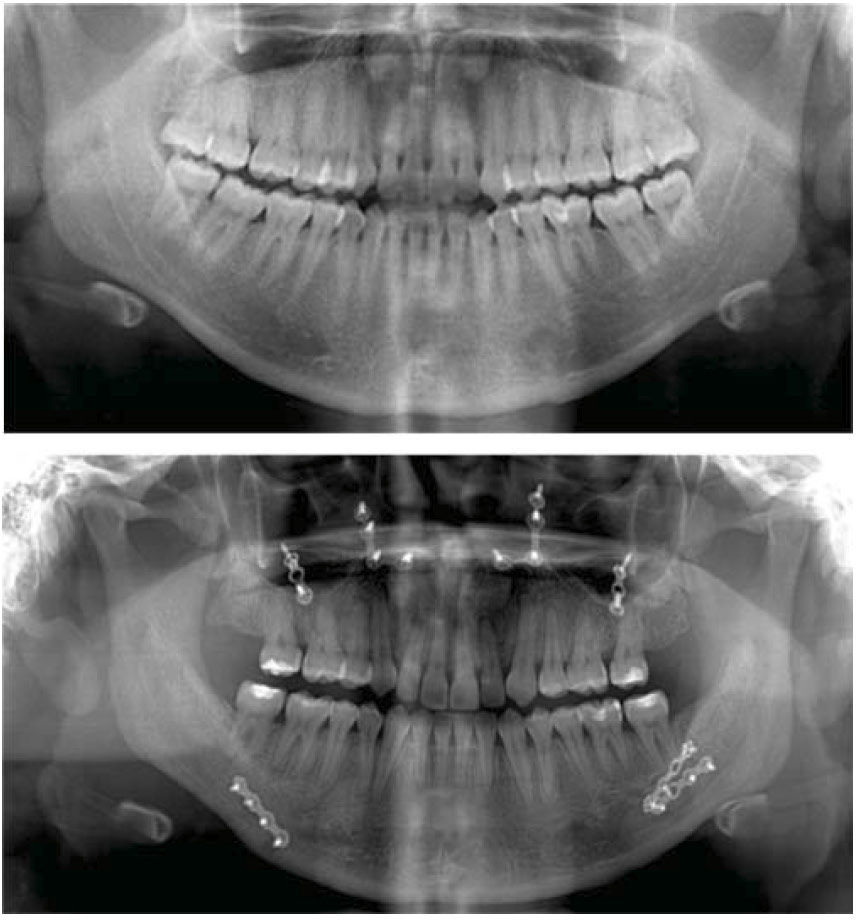
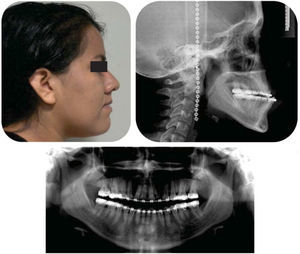
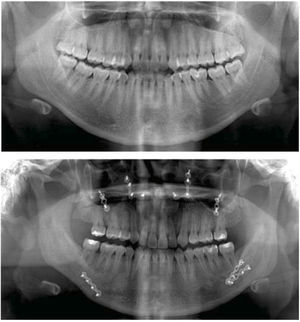
OrthopantomographyIn the orthopantomography it was observed the presence of the 32 permanent teeth, good crown-root ratio (1:2), goodbone level, asymmetry of the mandibular ramus and no sign of TMJ disease (Figure 3).
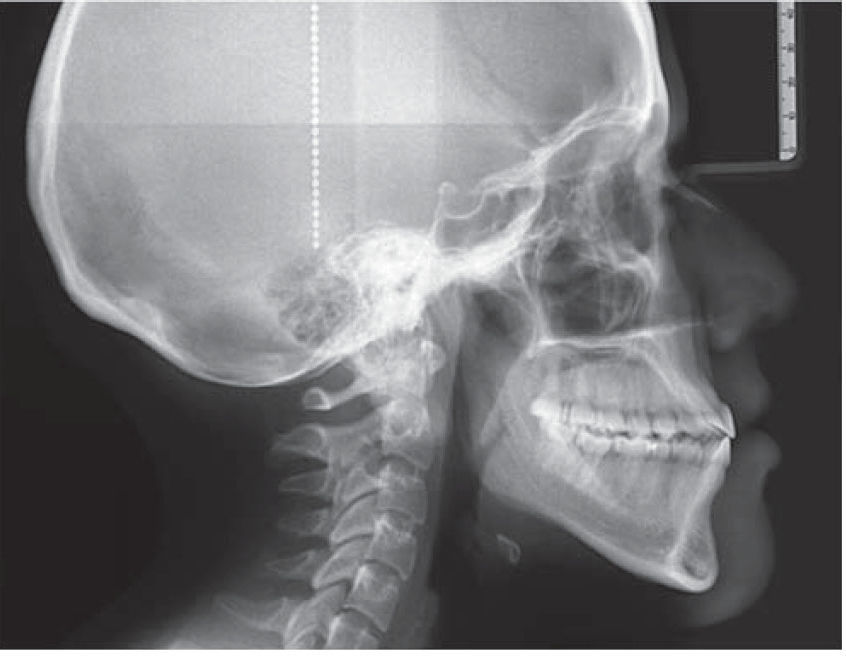
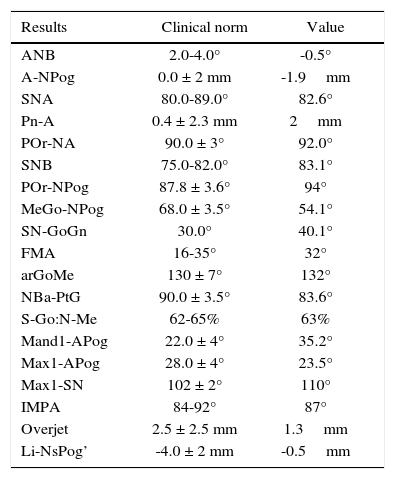
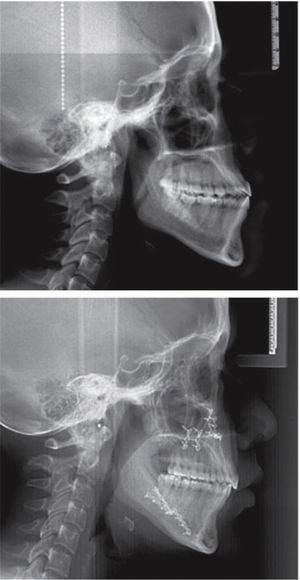
Cephalometric analysisThe cephalometric analysis revealeda skeletal class III due to prognathism, mandibular hyperdivergence posterior cross bite, upper incisor proclination, lower incisor retroclination and dentoalveolar biprotrusion (Figure 4andTable I).
Initial cephalometric values.
| Results | Clinical norm | Value |
|---|---|---|
| ANB | 2.0-4.0° | -0.5° |
| A-NPog | 0.0 ± 2 mm | -1.9mm |
| SNA | 80.0-89.0° | 82.6° |
| Pn-A | 0.4 ± 2.3 mm | 2mm |
| POr-NA | 90.0 ± 3° | 92.0° |
| SNB | 75.0-82.0° | 83.1° |
| POr-NPog | 87.8 ± 3.6° | 94° |
| MeGo-NPog | 68.0 ± 3.5° | 54.1° |
| SN-GoGn | 30.0° | 40.1° |
| FMA | 16-35° | 32° |
| arGoMe | 130 ± 7° | 132° |
| NBa-PtG | 90.0 ± 3.5° | 83.6° |
| S-Go:N-Me | 62-65% | 63% |
| Mand1-APog | 22.0 ± 4° | 35.2° |
| Max1-APog | 28.0 ± 4° | 23.5° |
| Max1-SN | 102 ± 2° | 110° |
| IMPA | 84-92° | 87° |
| Overjet | 2.5 ± 2.5 mm | 1.3mm |
| Li-NsPog’ | -4.0 ± 2 mm | -0.5mm |
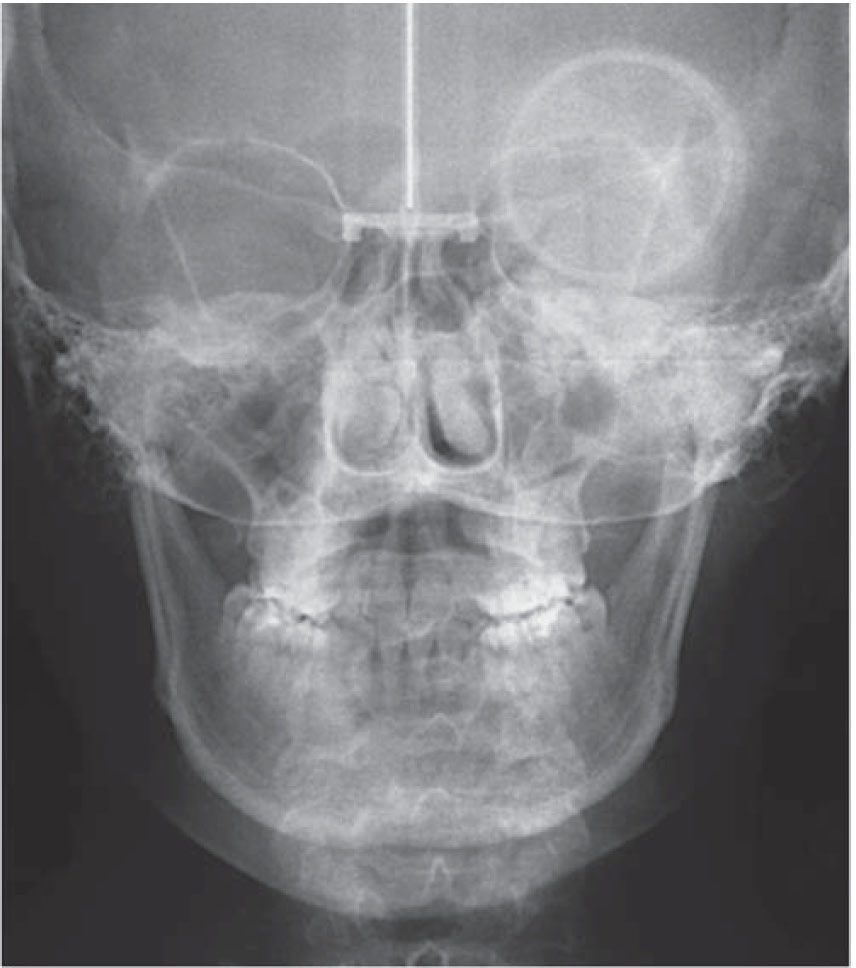
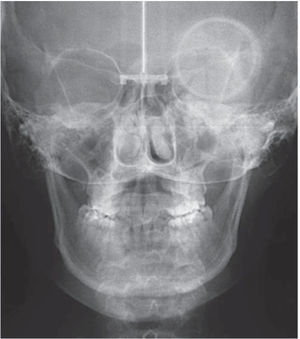
Ricketts posteroanterior cephalometry showed a mild maxillary collapse (Figure 5).
Treatment alternativesTreatment goals consisted in: correcting prognathism, improving the profile and the lip position, decrease the lower facial third, correct the crowding, dental rotations and crossbite; obtain molar class II and canine class I, correct the axial axis of the upper and lower incisors, reduce the dental biprotrusion, match dental midlines, improve the overbite overjet; improve arch form and achieve skeletal class I.
After establishing the diagnosis and treatment objectives, the Department of Orthodontics conducted an interconsultation with the Department of Maxillofacial Surgery, in order to perform together a surgical treatment plan.
Therefore it was suggested to the patient the removal of the third molars and first upper premolars with the aim of correcting the upper incisor proclination. Subsequently an orthodontic-surgical treatment would be performed which consisted of three phases: I. presurgical orthodontic phase: 0.022” slot Roth appliances were placed in April 2013, with anarch wire sequence suitable for the problem that the patient presented. Afterwards, surgical phase II was begun in September 2014: Lefort 1 osteotomy, maxillary advancement of 3mm and a 1mm anterior impaction; vertical osteotomies of the mandibular ramus, 3mm mandibular retrusion; and phase 3: postsurgical orthodontics, where the case was detailed, correcting muscle patterns and occlusal settlement.
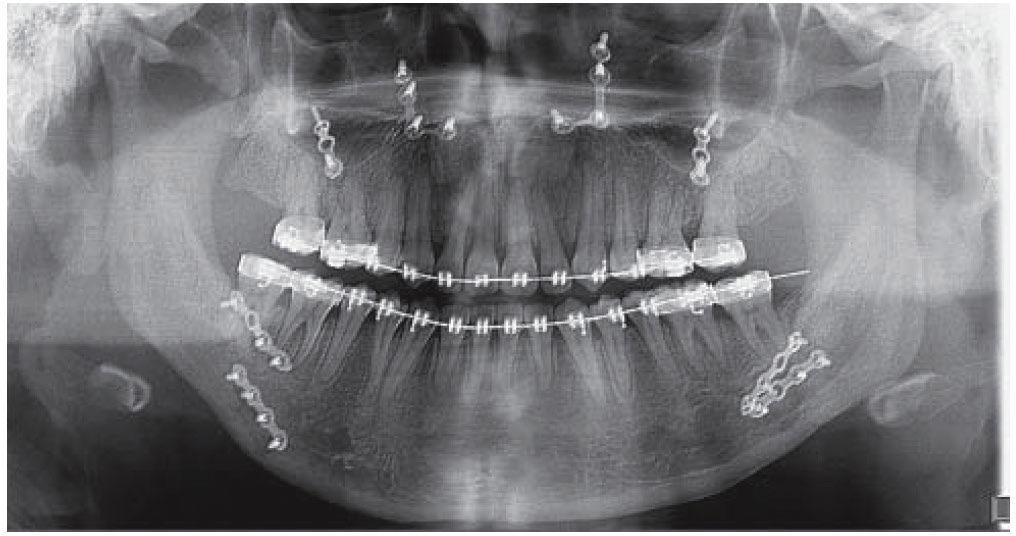
Treatment progressSubsequent to the removal of the third molars and upper first premolars, it was proceeded to the placement of fixed appliances Roth slot 0.022” x 0.025” to begin phase I, starting with 0.014” NiTi arch wires in both arches to begin with the alignment and leveling (Figure 6).
Treatment continued with the first phase, aligning and leveling, using 0.016” NiTi round arch wires, and subsequently torsion movements were begun to express with 0.016” x 0.016” square arch wires and 0.016” x 0.022” NiTi, 0.017” x 0.025” NiTi and 0.019” x 0.025” NiTi rectangular ones. A month after, 0.019” x 0.025” DKHL stainless steel arch wires were used to begin space closure in the upper arch (Figure 7).
The objective of the pre-surgical orthodontics is to decompensate the inclinations of the dental axis.
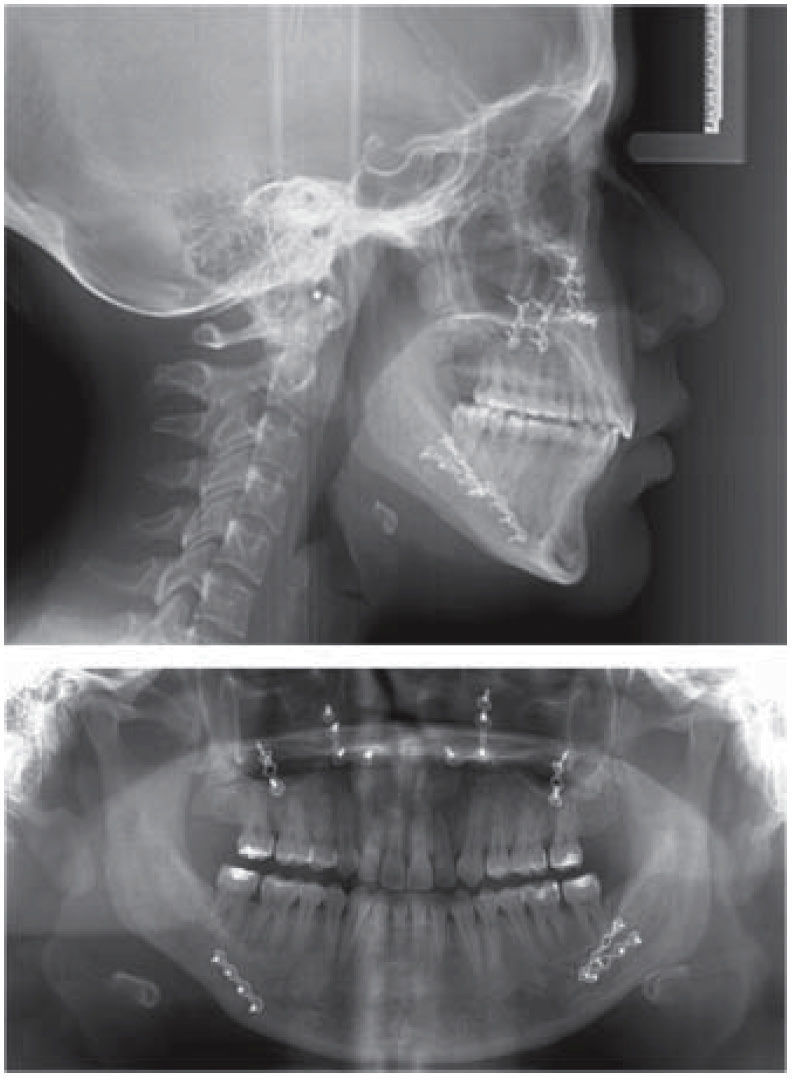
The phase of alignment and leveling lasted approximately 8 months and the space closure phase, approximately 7 months, so that after 15 months the case was re-assessed by obtaining study and work models, a lateral headfilm, and an orthopantomography. Working as a team with the department of maxillofacial surgery the orthognathic surgery was programmed (Figure 8), the patient was informed of the surgical risks and complications by means of validly informed consent.
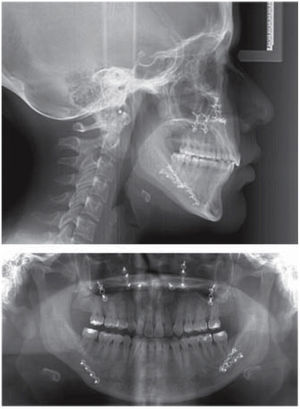
Surgical arch wires (0.019” x 0.025” stainless steel with crimpable hooks) were placed prior to the surgery. The surgical procedure consisted in a Lefort 1 osteotomy, 3mm maxillary advancement and 1mm anterior impaction; vertical osteotomies of the mandibular ramus, mandibular retrusion of 3mm. The osteosynthesis material that was used in the maxilla consisted of two short L-plate bridges with 12 screws in total and a plate of 6 holes. In the mandible, two plates of 8 holes each were used, 7 screws on the right side and 6 on the left.
Seven days after the surgery intermaxillary elastics were placed in order to correct the muscle pattern. These elastics had class III settlement vectors (Figure 9).
The patient continued to wear the elastics to correct muscular patterns and occlusal settlement (Figure 10).
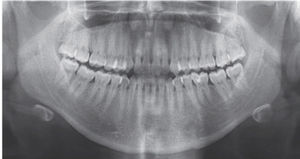
An orthopantomography was obtained to verify root parallelism (Figure 11).
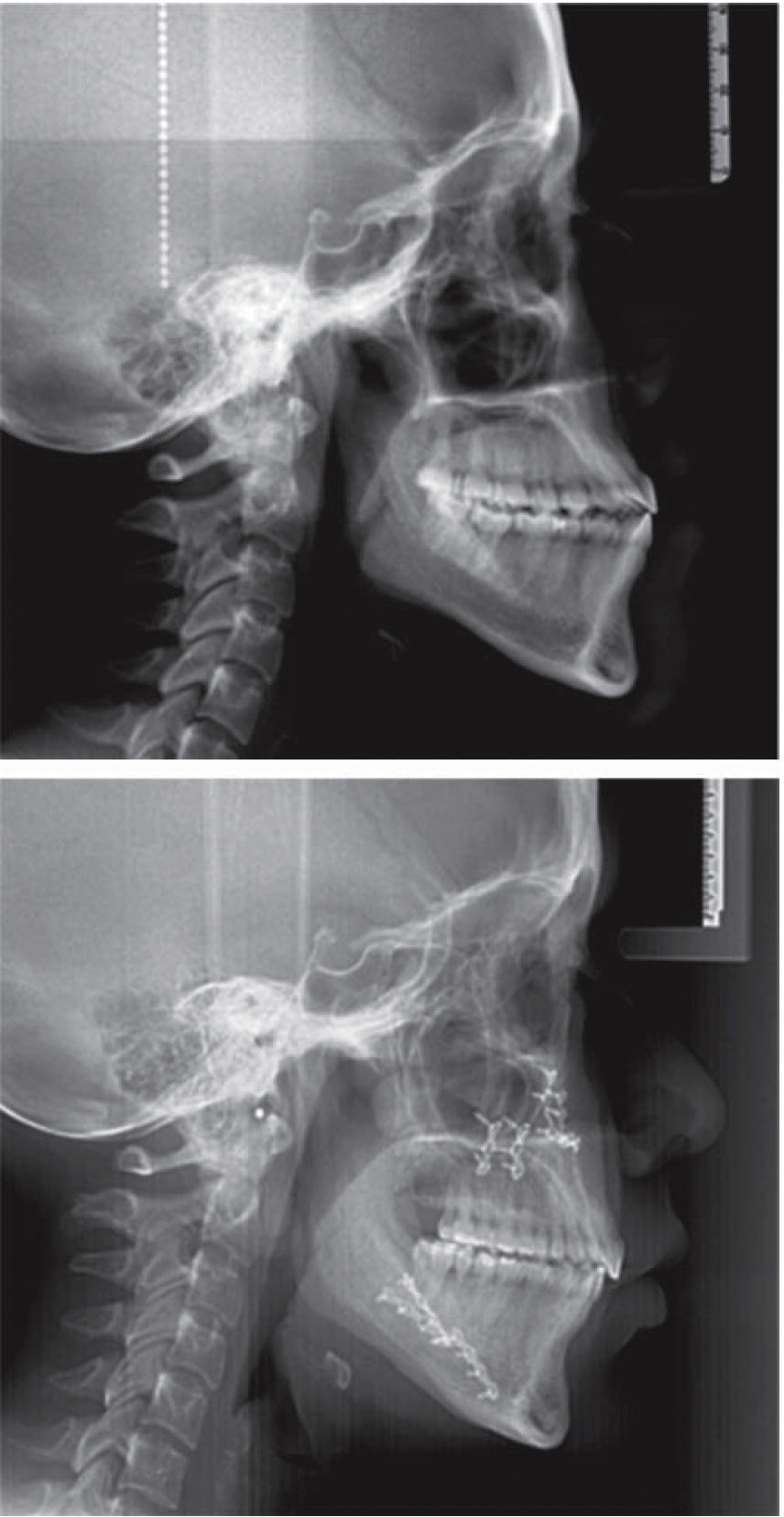
RESULTSTreatment was completed in 24 months. Prognathism was corrected, the profile was improved, a decrease of the lower third of the face was obtained and the skeletal class I was achieved, providing improvement in the facial harmony.
The patient retained her positive smile (Figure 12).
The crossbite was corrected thus leaving a more stable case; canine class I and molar II were obtained. The dental midlines were kept coincident, arch form was improved as well as the overbite and overjet. The dental crowding was corrected as were the dental rotations (Figure 13).
The axial inclinations of the incisors were corrected and root parallelism was achieved as well as a skeletal class I (Figure 14).
0.036” wire circumferential retainers with acrylic on the anterior teeth were placed. Likewise, an occlusal adjustment was performed (Figure 15).
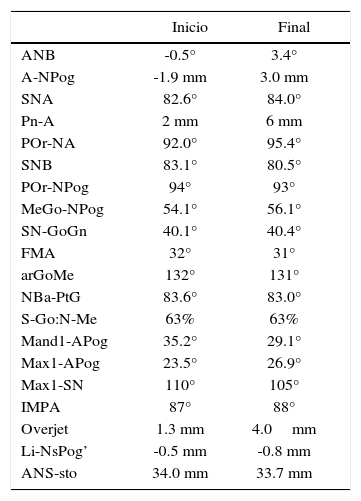
The obtained facial changes may be observed (Figure 16), intraoral (Figure 17), radiographic (Figures 18 and 19) and cefalometric (Table II).
Comparative cephalometric values.
| Inicio | Final | |
|---|---|---|
| ANB | -0.5° | 3.4° |
| A-NPog | -1.9 mm | 3.0 mm |
| SNA | 82.6° | 84.0° |
| Pn-A | 2 mm | 6 mm |
| POr-NA | 92.0° | 95.4° |
| SNB | 83.1° | 80.5° |
| POr-NPog | 94° | 93° |
| MeGo-NPog | 54.1° | 56.1° |
| SN-GoGn | 40.1° | 40.4° |
| FMA | 32° | 31° |
| arGoMe | 132° | 131° |
| NBa-PtG | 83.6° | 83.0° |
| S-Go:N-Me | 63% | 63% |
| Mand1-APog | 35.2° | 29.1° |
| Max1-APog | 23.5° | 26.9° |
| Max1-SN | 110° | 105° |
| IMPA | 87° | 88° |
| Overjet | 1.3 mm | 4.0mm |
| Li-NsPog’ | -0.5 mm | -0.8 mm |
| ANS-sto | 34.0 mm | 33.7 mm |
Direct source.
Espeland and Bailey pointed out that skeletal class III malocclusions are the anomalies that in the majority of cases are corrected with orthognathic surgery combined with orthodontic treatment.17,18
Bailey and Johnston mentioned that historically, skeletal class III malocclusions have been treated only with mandibular retrusion, but several recent studies indicate that bimaxillary procedures have become more frequent.14,18
Kwon recognizes that skeletal class III malocclusion is frequently combined with a vertical discrepancy. The nature of the abnormality provides instructions for performing surgical repositioning and in this way achieve facial harmony. It has been indicated that vertical changes can affect the amount of mandibular relapse.19 Bothur and Proffit et al mentioned that there are numerous studies on maxillary surgery stability.20,21 Jakobsone, Moldez, Costa and Proffit stated that several studies have established that stability has been maintained after vertical changes in the position of the maxilla.22–25
Typical dental decompensation consists in retracting or retroclining the proclined maxillary incisors and proclinating the retroclined mandibular incisors to a more normal axial inclination. This increases the severity of the class III dental malocclusion and often results in a less esthetic facial profile before the surgery.13,14,26 The presurgical dental decompensation determines the magnitude and type of the surgical changes and is the main factor in treatment success. The absence of an optimal dental decompensation compromises the quality and quantity of the orthodontic correction.26,27
Proffit collected that within the hierarchy of procedures for orthognathic surgery with long-term stability, maxillary impaction is the most stable procedure and its maintenance with internal rigid fixation or with wire, has no influence on the stability of maxillary impactions.27
It is of the utmost importance that patients who have been undergone dental decompensation use orthodontic appliances during some months after the surgery in order to achieve stability of the dentoalveolar and skeletal structures thus achieving a totally harmonic result.28
An adequate bone support was achieved, producing a better appearance of the soft tissues. Facial analysis and the knowledge of the effects that the surgical changes of the mandible originates when it is displaced horizontally, are the key to improving the balance and harmony of the face.
CONCLUSIONSBone discrepancies play an important role in orthodontic treatments; before beginning treatment one must have a precise diagnosis aided by all the tools available at the moment. Planning for orthodontic-surgical treatments must be performed in an interdisciplinary manner since diagnosis is begun. Patient cooperation is essential. Whatever the dentofacial deformity, there should be a protocol of individualized attention, by listing in order of importance the needs of the patient in order to resolve them in a timely manner and in the required order.
In the clinical practice, the choice between several surgical procedures is based on clinical examination and cephalometric evaluation. One of the main issues of maxillofacial surgeons and orthodontists in the diagnosis and treatment planning of the surgical patients is the final aesthetic appearance of the soft tissues profile. To achieve an optimal profile in the post-surgical phase, the contour balance of the soft tissues and the relative anteroposterior positions of the nose, lips and chin should be assessed. Despite the fact that most of the skeletal relapse occurs during the first six months after surgery, the patient hereby presented showed skeletal stability and benefited from the stability obtained through the maxillary advancement and impaction. Dental decompensation contributed to the occlusal stability, highlighting the importance of the post-surgical orthodontic stage by means of detailing and retention.
The orthodontic-surgical protocol allowed for the patient to have, at the end of the orthodontic treatment, a beautiful facial profile thanks to the maxillary advancement and impaction as well as the mandibular retroposition. The posterior cross bite was also corrected; bilateral canine and molar class I was achieved, dental midlines coincided and normal overbite and overjet were obtained, as well as an adequate root parallelism, canine guidance and incisive disocclusion. During smile, a good exposure of the maxillary incisors and an excellent facial balance was obtained. The patient responded well physiological and psychologically and was very satisfied with the treatment results.
Student of the Orthodontics Specialty of the Division of Postgraduate Studies and Research.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia
Professor of the Orthodontics Specialty.
Student of the Oral and Maxillofacial Department, Division of Postgraduate Studies and Research, Faculty of Dentistry, UNAM.
Professor of the Oral and Maxillofacial Department, Division of Postgraduate Studies and Research, Faculty of Dentistry, UNAM.