The cleft lip, alveolus and palate is a very common congenital condition in Mexican population (1 of every 700 live births). It requires prompt interdisciplinary attention focused on effective and efficient therapies aimed to improve the esthetic and physiological aspects. These anomalies affect breathing and eating, as well as the esthetics, if they are not corrected in a timely manner. The purpose of this paper is to present a case report of a pediatric patient on an infant stage with unilateral left cleft lip alveolus and palate which was addressed with a treatment based on a static set of plates for the formation and treatment ridge (SPECTRA) with very encouraging results. We present this case to serve as a model of care for future cases in which clinicians may choose the described pre-surgical orthopedics since it is simple, safe, clean, and provides extensive control for the clinician.
La fisura labio alveolo palatina es una patología congénita muy frecuente en la población mexicana (1-700 recién nacidos vivos), estos pacientes requieren siempre de una atención interdisciplinaria inmediata, enfocada de forma eficaz y eficiente a mejorar los aspectos físicos y fisiológicos, debido a que las alteraciones se reflejan en la respiración y la alimentación; y también las estéticas, que se agravaran si no son atendidos de forma oportuna. El propósito de este trabajo es presentar el caso clínico de un paciente en etapa lactante con fisura labio alveolo palatina unilateral izquierda, el cual fue abordado con un tratamiento a base de una serie de placas estáticas para la conformación y tratamiento del reborde alveolar (SPECTRA), con resultados muy alentadores. Se presenta este caso para que sirva como modelo de atención para futuros pacientes, ya que la técnica de ortopedia prequirúrgica descrita es simple, segura, limpia y con un amplio control por parte del clínico.
Cleft lip, alveolus and palate are as old as humanity1 itself and are the result of the lack of fusion of the central and lateral process during embryonic development. It has a congenital and multifactorial etiology.2 Among the determining factors for CLAP are nutrition, lack of folic acid, high alcohol, tobacco or drug consumption during pregnancy, and some medications such as anxiolytics, barbiturics and phenytoin or hydantoin.3
Children that are born with CLAP have their quality of life affected since the moment they are born due to the conditions in which he or she are born and to the controversial feelings that parents often face, especially the mother.4 In Mexico, CLAP incidence according to Arrendares and Lisker is 1:7405–7 live births, and an increased number in the states of Oaxaca, Chiapas, Veracruz, Quintana Roo and Jalisco.2
Clinical featuresChildren with cleft palate present physiopathological irregularities such as the inability to perform suction because the mouth is permanently communicated with the nasal cavity. As a result the liquids contained within the mouth penetrate easily into the larynx causing poor fluid management and recurrent upper airway infections.
McNeil (1950) makes the concept of early maxillary orthopedics in children with CLAP1,7,8 popular as a treatment modality where the forces directed by an intra or extra oral appliance are used to change the position of secondarily displaced tissues due to a deformity such as CLAP.9
Presurgical nasoalveolar moldingDescribed by Grayson and his team (1997- 1999),10–12 it is a method used in patients with unilateral CLAP (UCLAP). Although there are few reports on its efficacy in patients with bilateral CLAP, it is known that the incidence for this deformity is smaller than the one for UCLAP; less than 10% of CLAP13 are bilateral. In recent years this technique has caused great interest and has been applied as a new approach for the traditional presurgical orthopedic methods in children with CLAP.8–10
Series of static plates for the conformation and treatment of the alveolar ridgeThe birth of a baby with unilateral or bilateral CLAP requires a treatment plan based on quality and safety with an organized care interdisciplinary team in which each and every member knows his or her specific role and the exact moment to perform it.
The orthopedic intervention must be performed in the first days of life by taking intraoral photographs whenever this is possible, extraoral photographs and taking impressions of the alveolar ridge under careful supervision from an expert since we are talking about a neonate. Impressions are taken with special baby trays and they must register accurately the depth of the alveolar segments for the fabrication of the appliance using conventional techniques for the conformation of the orthopedics plates.8,14
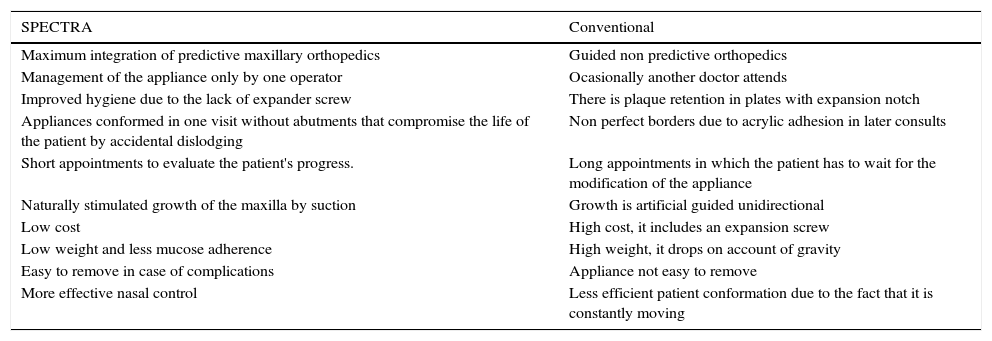
Once the orthopedic appliance has been made (without the expansion screw) (Table I) it can be sustained by means of stainless steel stabilizers coming from the medial region or with aid of an hypoallergenic tape fixed to both cheeks, thus creating a slight pressure that will confront the soft tissues and diminish the cleft.8,15,16
Advantages of using SPECTRA over the conventional technique with expansion screws.
| SPECTRA | Conventional |
|---|---|
| Maximum integration of predictive maxillary orthopedics | Guided non predictive orthopedics |
| Management of the appliance only by one operator | Ocasionally another doctor attends |
| Improved hygiene due to the lack of expander screw | There is plaque retention in plates with expansion notch |
| Appliances conformed in one visit without abutments that compromise the life of the patient by accidental dislodging | Non perfect borders due to acrylic adhesion in later consults |
| Short appointments to evaluate the patient's progress. | Long appointments in which the patient has to wait for the modification of the appliance |
| Naturally stimulated growth of the maxilla by suction | Growth is artificial guided unidirectional |
| Low cost | High cost, it includes an expansion screw |
| Low weight and less mucose adherence | High weight, it drops on account of gravity |
| Easy to remove in case of complications | Appliance not easy to remove |
| More effective nasal control | Less efficient patient conformation due to the fact that it is constantly moving |
By obtaining a better rotation of the bigger segment into a more normal position, the plate notch for the frenulum is commonly widened. The passive acrylic plate is relieved with rectifying acrylic on the palatal surface so that the upper segments are moved into more normal positions and to allow growth in its peripheral margins.8
After the use of the first appliance, the next orthopedic plate is constructed making a transverse cut of the model to separate the alveolar process from its maxillary base and a predictive reposition is made of no more than 2 mm of the segment that is intended to be moved. The segment of the alveolar process is fixed with dental cast and a new objurgating plate is fabricated repeating the technique until the desired results are obtained using each plate for 3 weeks approximately. The complete reduction of the alveolar segments and a passive molding are performed to maintain the alveolar segments in the new position improving maxillary conformation.15,17
«The key of the technique is in the models, not the appliance»
Case report82-day-old male patient diagnosed with hydrocefalia, complete unilateral left CLP and guarded prognosis is referred by neurosurgery (Figure 1). Treatment for maxillary molding is initiated through a series of static plates SPECTRA and guidance for maxillary growth was accomplished through predictive analysis and the reduction of the alveolar segments using six appliances all fabricated with the SPECTRA philosophy. Successful presurgical preparation was obtained in three months (Figure 2).
ResultsThe use of the SPECTRA technique may vary from eight to ten months treatment time with a twelve- hour use per day.15 It is important to know that the use of this passive plate will always be bound to the patient's growth and that it will have developmental consequences, changing the position of anatomical structures until a better molding of the maxilla is achieved.12 Subsequently the lip reduction (cheiloplasty) is performed. Cheiloplasty will be made according to each hospital protocols and the patient's evolution. Once the surgery is conducted the use of the obturating plate is reconsidered.8
ConclusionsIt must be taken under consideration not only the surgical procedures but also, the functional and esthetic maxillofacial growth.14 Good maxillary conformation will have multiple advantages over the primary and secondary palatal closure, as one step procedures after palatoplasties at 18 months average age or sooner due to the language problems that develop at later stages.13 CLAP patients undergo extensive treatments that begin at birth and continue through adulthood after the craniofacial growth has been completed. Treatment may involve orthodontics and occasionally orthognatic surgeries.16 There must be a multidisciplinary team with a maxillofacial surgeon, an orthodontist, a plastic surgeon, a pediatrician phonetician, an audiologist, otorhinolaryngologist, psychologist and sometimes a genetics specialist.6 They must have purposeful ideas that have a positive impact on the quality of life of children with CLAP (Figure 3).
The effect of orthopedics in children with CLAP has been studied for decades and still it is controversial for some authors (Ross, 1987; Asher-McDade et al., 1992; Winters and Hurwitz, 1995) but there are still some advantages that can be considered improving the child's facial appearance and making lip and maxillary conformation surgeries much easier by means of stimulation.18