Pediatric bipolar disorder (PBD) has emerged as a research field in which psychosocial treatments have provided a plethora of empirical findings over the last decade. We addressed this issue through a systematic review aimed of establishing their effectiveness and feasibility as adjunctive therapies for youth with PBD or at high-risk for PBD. A comprehensive search of databases was performed between 1990 and September 2014. Overall, 33 studies were specifically related to the issue and 20 of them were original articles. Evidence suggests that both “multi-family psychoeducational psychotherapy” and “family-focused therapy” are possible effective treatments for PBD. Likewise, “child and family-focused cognitive-behavioral therapy” may be characterized as a treatment in its experimental phase. The remaining therapies fail to obtain enough empirical support due to inconsistent findings among clinical trials or data solely based on case reports. Studies of psychosocial treatments provide concluding results concerning their feasibility and acceptability. Larger sample sizes and more randomized controlled trials are mandatory for diminishing methodological shortcomings encountered in the treatments displayed.
El trastorno bipolar pediátrico (TBP) se ha convertido en un campo de investigación en el que los tratamientos psicosociales han proporcionado una gran cantidad de hallazgos empíricos en la última década. Abordamos esta cuestión a través de una revisión sistemática destinada a establecer su eficacia y viabilidad como terapias adyuvantes para los jóvenes con TBP o en alto riesgo de TBP. Se realizó una búsqueda exhaustiva en bases de datos entre 1990 y septiembre del 2014. En total, 33 estudios se relacionaron específicamente con el tema y 20 de ellos eran artículos originales. La evidencia muestra que tanto la “psicoeducación familiar” como la “terapia familiar para adolescentes” son tratamientos probablemente eficaces en el TBP. Del mismo modo, la “terapia cognitivo-conductual centrada en el niño y la familia” se puede caracterizar como un tratamiento en fase experimental. Las terapias restantes no obtienen suficiente apoyo empírico, ya sea por la presencia de hallazgos inconsistentes entre los distintos ensayos clínicos, ya por contar con datos únicamente provenientes de estudios de casos. Además, los resultados de los estudios sobre tratamientos psicosociales proporcionan resultados concluyentes en cuanto a la viabilidad y aceptabilidad de dichas terapias. Son necesarios ensayos clínicos controlados con muestras de mayor tamaño con el fin de disminuir las deficiencias metodológicas encontradas en una gran parte de los tratamientos descritos.
Pediatric bipolar disorder (PBD) is a mental disorder affecting roughly 2% of youth less than 18-years-old.1,2 Likewise, for 55–60% of adult subjects with bipolar disorder (ABD) their pathology is initiated during childhood or adolescence,3 frequently exhibiting subthreshold forms of the disorder.4–6 The persistence of this psychopathology into early adulthood leads to poorer academic achievements as well as greater interpersonal conflicts.7–9 Hence, reducing early etiopathogenic factors and symptoms of bipolarity may increase the probability of good prognosis at long-term.
Over the last 15 years, a biopsychosocial framework for PBD has obtained growing recognition. Thus, an increasingly multimodal treatment approach has emerged. Accordingly, although psychopharmacological treatments are considered the primary intervention in the PBD,10,11 psychosocial therapies have been proposed as a means of addressing psychological vulnerabilities (e.g., emotional dysregulation), family distress (e.g., expressed emotion, EE), and life stress (e.g., interpersonal conflicts) that may influence PBD at early stages.12 As adjunctive interventions, some psychosocial therapies, mainly adapted from ABD, have provided preliminary evidence about their feasibility and effectiveness in PBD subjects.13,14 Likewise, other psychosocial interventions have been postulated to cope with the prodromal signs of bipolarity in childhood and adolescence.15 Overall, both primary and secondary interventions constitute proper treatments among non-adult populations.
To date, several previous systematic reviews have been undertaken in PBD.14,15 However, none of them have included: (i) recent advances in some psychosocial treatments for adolescents (family-focused therapy, FFT-A; interpersonal and social rhythm therapy, IPSRT-A; dialectical behavioral therapy, DBT-A), (ii) motivational techniques for decreasing untoward effects of psychotropic medications in PBD and (iii) psychological treatments for comorbid conditions among PBD youth.16,18 Overall, the main aim of this systematic review is to examine every psychological intervention delivered in PBD patients from childhood to adolescence. For each specific therapy we seek to show its (i) rationale, (ii) core features and therapeutic elements and (iii) degree of empirical support.
MethodsSearch strategyA literature search was carried out through PsycINFO and PubMed databases from 1990 to September 2014. Terms employed included indexing terms (e.g., MeSH) and free texts: ((psychosocial treatment OR psychological treatment) AND (youth OR pediatric OR child OR adolescent) AND (bipolar disorder)).
Selection criteriaSelected manuscripts should include subjects: (i) aged from 6 to 19-years-old; (ii) undergoing psychotherapy for PBD and (iii) diagnosed of bipolar disorder type I (BDI), bipolar disorder type II (BD II), or bipolar disorder not otherwise specified (BD NOS) according to DSM-IV-TR criteria.19 Likewise, children whose parents suffered from BD were also included in the HR-PBD section. Overall, we collected 20 original manuscripts, namely: 4 case reports (CR), 9 open trials (OT), and 7 randomized controlled trials (RCT). It must be pointed out that our review comprised RCT, OT and CR due to the scarcity of experimental research on this topic. Moreover, all the psychological interventions were employed with subjects undergoing psychopharmacological treatment with the exception of youth at HR-BD. Moreover, other 13 related manuscripts were recruited, that is 8 systematic reviews and 5 theoretical essays. In addition, 61 papers were used to account for the rationale and core features of every intervention displayed. Studies in which patients were diagnosed through questionnaires (e.g., child behavior checklist “CBCL-bipolar phenotype”) were excluded because of lack of diagnostic validity.20
Data extractionThe following variables were recorded: (i) type of psychological intervention; (ii) sample targeted (children vs adolescents); (iii) rationale and background; (iv) core features (e.g., number and duration of sessions, goals, psychological techniques); (v) empirical support (CR vs OT vs RCT studies) and (vi) outcomes measure (e.g., time to recovery, recurrence episodes, depressed/manic mood, interpersonal functioning).
Method of analysisThere was remarkable heterogeneity among selected studies concerning the design (CR vs OT vs RCT) and the outcomes measure (e.g., psychopathology, functionality and course). Also, the sample sizes were generally small. For these reasons, we present a descriptive review of the studies instead of a meta-analysis.
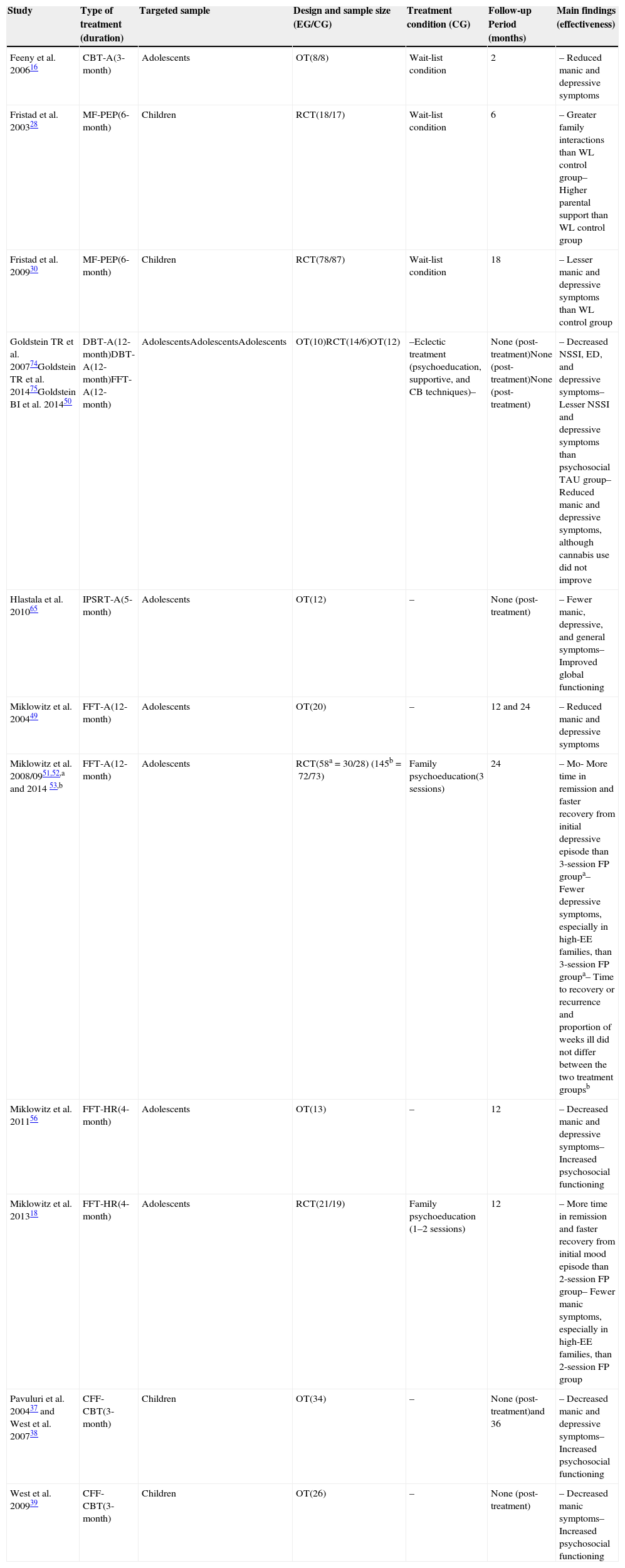
ResultsDue to developmental considerations, psychological interventions were divided according to their use with either children or adolescents with PBD/HR-PBD. For instance, family psychoeducation (FP) as well as child and family-focused cognitive-behavioral therapy (CFF-CBT) were classified as therapies for children. Moreover, a group of psychological interventions were included as therapies for adolescents, namely: FFT-A, CBT-A, IPSRT-A, DBT-A, and motivational interviewing (MI). Major findings are described in Table 1.
Overview of clinical trials related to psychosocial treatments in PBD.
| Study | Type of treatment (duration) | Targeted sample | Design and sample size (EG/CG) | Treatment condition (CG) | Follow-up Period (months) | Main findings (effectiveness) |
|---|---|---|---|---|---|---|
| Feeny et al. 200616 | CBT-A(3-month) | Adolescents | OT(8/8) | Wait-list condition | 2 | – Reduced manic and depressive symptoms |
| Fristad et al. 200328 | MF-PEP(6-month) | Children | RCT(18/17) | Wait-list condition | 6 | – Greater family interactions than WL control group– Higher parental support than WL control group |
| Fristad et al. 200930 | MF-PEP(6-month) | Children | RCT(78/87) | Wait-list condition | 18 | – Lesser manic and depressive symptoms than WL control group |
| Goldstein TR et al. 200774Goldstein TR et al. 201475Goldstein BI et al. 201450 | DBT-A(12-month)DBT-A(12-month)FFT-A(12-month) | AdolescentsAdolescentsAdolescents | OT(10)RCT(14/6)OT(12) | –Eclectic treatment (psychoeducation, supportive, and CB techniques)– | None (post-treatment)None (post-treatment)None (post-treatment) | – Decreased NSSI, ED, and depressive symptoms– Lesser NSSI and depressive symptoms than psychosocial TAU group– Reduced manic and depressive symptoms, although cannabis use did not improve |
| Hlastala et al. 201065 | IPSRT-A(5-month) | Adolescents | OT(12) | – | None (post-treatment) | – Fewer manic, depressive, and general symptoms– Improved global functioning |
| Miklowitz et al. 200449 | FFT-A(12-month) | Adolescents | OT(20) | – | 12 and 24 | – Reduced manic and depressive symptoms |
| Miklowitz et al. 2008/0951,52,a and 2014 53,b | FFT-A(12-month) | Adolescents | RCT(58a=30/28) (145b=72/73) | Family psychoeducation(3 sessions) | 24 | – Mo- More time in remission and faster recovery from initial depressive episode than 3-session FP groupa– Fewer depressive symptoms, especially in high-EE families, than 3-session FP groupa– Time to recovery or recurrence and proportion of weeks ill did not differ between the two treatment groupsb |
| Miklowitz et al. 201156 | FFT-HR(4-month) | Adolescents | OT(13) | – | 12 | – Decreased manic and depressive symptoms– Increased psychosocial functioning |
| Miklowitz et al. 201318 | FFT-HR(4-month) | Adolescents | RCT(21/19) | Family psychoeducation (1–2 sessions) | 12 | – More time in remission and faster recovery from initial mood episode than 2-session FP group– Fewer manic symptoms, especially in high-EE families, than 2-session FP group |
| Pavuluri et al. 200437 and West et al. 200738 | CFF-CBT(3-month) | Children | OT(34) | – | None (post-treatment)and 36 | – Decreased manic and depressive symptoms– Increased psychosocial functioning |
| West et al. 200939 | CFF-CBT(3-month) | Children | OT(26) | – | None (post-treatment) | – Decreased manic symptoms– Increased psychosocial functioning |
CB, cognitive behavioral; CFF-CBT, child and family-focused cognitive-behavioral therapy; CG, control group; DBT-A, dialectical behavioral therapy for adolescents; ED, emotional dysregulation; EE, expressed emotion; EG, experimental group; FP, family psychoeducation; FFT-A, family-focused therapy for adolescents; FFT-HR, family focused therapy for high-risk; IPSRT-A, interpersonal and social rhythm therapy for adolescents; MF-PEP, multifamily psychoeducational psychotherapy; OT, open trial; NSSI, non-suicidal self-injuries; RCT, randomized controlled trial; PBD, pediatric bipolar disorder; TAU, treatment as usual; WL, wait-list.
Rationale. A vast majority of studies carried out in adult bipolar disorder (BD) have found decreased insight among these patients, even during periods of symptom remission.21 Poor insight is related to worse treatment adherence,22 ultimately increasing the risk for relapses and caregiver burden.23 Hence, identifying prodromal features of PBD may improve both insight and the course of the illness.24 This suggests the need for increasing the knowledge that youth and their relatives possess about PBD.
Core features and therapeutic elements. Multi-family psychoeducational psychotherapy (MF-PEP) includes 8 sessions of 90min that occur separately but simultaneously for parents and children.25 The main goals of MF-PEP are: increasing knowledge and understanding about PBD as well as its treatment options and compliance; improving detection and management of the prodromal symptomatology; and enhancing the child and family's sense of support in dealing with PBD.26
Empirical support. Compared to the empirical support for psychoeducational programs for adults with BD, there is still scarce research about FP in PBD.27 However, two RCT for MF-PEP have been implemented over the past 10 years. In the first RCT, 35 children with mood disorders (BD, n=16) aged 8–11-years-old and 47 parents were allocated to either MF-PEP (n=18) or a 6-month wait-list control condition (n=17). Main outcomes found in the MF-PEP group were: increased parental knowledge about childhood mood symptoms; enhanced positive family interactions as reported by the parent; improved perceptions of parental support as reported by children; and increased utilization of appropriate services by families. Surprisingly, there was no decrease in negative family interactions throughout a 6-month follow-up.28 Likewise, the MF-PEP group reported more gains in knowledge, skills and support than the control group during the initial 4 months of follow-up.29 The second RCT comprised 165 children aged 8–12 years with a major disorder (BD, n=115) who were assigned to MF-PEP (n=78) or 1 year wait-list condition (n=87). It obtained that the addition of MF-PEP improved affective symptomatology over 18 months of follow-up.30 Furthermore, as hypothesized, no significant pre- to post-treatment differences were found between groups for the mean number of current medications, but variance declined significantly from pre- to post-treatment.31 In sum, there is preliminary evidence supporting MF-PEP for PBD.26 As noted by the second RCT described, more empirical research with large sample size and adequate follow-up assessment is warranted.
Child and family-focused cognitive-behavioral therapy (CFF-CBT)Rationale. Youth that suffer from PBD are characterized by a failure of affect regulation prior to BD onset, which is exacerbated or sustained across the course of the illness.32 Likewise, subjects with PBD exhibit deficits in neurocognitive domains such as social cognition and working memory.33,34 Overall, these shortcomings preclude appropriate development in social, familiar, and academic settings. Ultimately, these deficits are reinforced and maintained by negative reactions from peers and family members.35 Thus, psychological interventions aimed at addressing (neuro) cognitive and emotional disturbances or biases are needed to improve the symptomatology and the functionality in subjects with PBD.
Core features and therapeutic elements. CFF-CBT, also known as the RAINBOW Program, includes children aged 6–12 and their parents, both individually and together. It comprises 12 sessions of 60–90min delivered weekly over the course of 3 months. CFF-CBT incorporates various psychological techniques that stem from an integrative approach not limited to traditional CBT, namely: psychoeducation, cognitive restructuring, self-regulation skills (mindfulness), positive thinking, interpersonal problem-solving, and communication skills. The main goals are improving symptomatology as well as psychosocial functioning. Specifically, CFF-CBT therapy aims at enhancing development in 7 core areas: routines, affect regulation, self-efficacy, negative thoughts and behaviors, social skills, interpersonal and family problem-solving, and social support.36
Empirical support. To date, one CR36 and three OT37–39 have been carried out. RCT have not been implemented yet. Firstly, an OT with 34 PBD children (mean age 11.33) and their relatives showed significant reductions in the severity of symptomatology as well as increased functionality. Higher levels of treatment compliance and satisfaction were also achieved.37 Later, an extension of the original study was carried out over 3 years in order to facilitate long-term improvements, with booster sessions administered every 1 or 3 months. Results obtained throughout these years found that there were no statistical differences on any measure, indicating the maintenance of the original results.38 No dropout was identified during this period. Moreover, an OT with CFF-CBT adapted for being delivered in parallel group format for both 26 children (mean age 9.45) and their parents found remarkable improvements in manic, but not depressive, symptoms and in children's psychosocial functioning post-treatment. Families stressed the feasibility and acceptability of this intervention.39 Finally, a CR showed improvements in psychopathology and psychosocial development in one child undergoing CFF-CBT.36 In sum, CFF-CBT is a promising intervention for PBD, but empirical support specifically focused on RCT is still lacking.
Psychological interventions for adolescents with bipolar disorderFamily-focused therapy for adolescents (FFT-A)Rationale. As noted by various studies, PBD parents are less warm and more punitive than control parents in communication with their offspring, with high EE interaction.40 Some factors that may account for this type of interaction are: elevated symptoms of mania, comorbidity with attention deficit and hyperactivity disorder (ADHD), an earlier onset of illness, living in a single parent home, and the presence of a parental mood disorder.40 In particular, parents who themselves have mood disorders are likely to transfer risk to their offspring through both environmental (e.g., negative affect) and genetic mechanisms.41 Related to this issue, some prospective studies have stressed that adolescents with BD and high EE parents have higher levels of depressive and manic symptoms over 1 or 2 years than BD adolescents with low EE parents.12,42,43 As a result, EE parents have been pointed out as useful predictors of the course of adolescent mood symptoms.12 Thus, family conflict may be an important target for psychological interventions in order to boost the speed and quality of recovery of these patients.
Core features and therapeutic elements. FFT-A involves the patient and parents or extended relatives (e.g., siblings), depending on who lives with the patient and who has a caregiving responsibility. FFT-A is given in 21 sessions over 9 months and is usually initiated during the recovery period following an acute episode of depression or (hypo)mania.44 The treatment is composed of 3 modules: (i) “psychoeducation” to make sense of their experiences with symptoms, recognize warning signs (through sleep logs and daily mood charts), accept the need for mood-stabilizing medications, and discriminate which behaviors are driven by personality vs bipolar disorder; (ii) “communication enhancement training” through role-playing for decreasing aversive interactions and encouraging active listening, giving constructive negative feedback and making positive requests for change and (iii) “problem-solving skills” to learn coping strategies and preventive measures for dealing with stressful events that may trigger mood swings.
Empirical support. Unlike FFT for adults with bipolar disorder,45,46 there are few studies of FFT focused on PBD, concretely two CR,47,48 two OT49,50 and two RCT.51–53 An OT comprised of 20 adolescents with BD (mean age 14.8) showed that FFT-A, in combination with mood stabilizing medications, yielded improvements in depression and manic symptoms over 1 year follow-up.49 Moreover, one RCT with 58 BD adolescents allocated to either FFT (n=30) or 3 sessions of family education (n=28) evidenced that FFT group had shorter recovery times from their initial depressive episodes, fewer depressive symptoms, and had more time in remission over 2 years of follow-up.51 FFT-A was particularly effective in stabilizing manic and depressive symptoms among adolescents in high EE (vs low EE) families.52 However, an extension of this previous study with 145 bipolar adolescents showed that time to recovery, or recurrence and proportion of weeks ill, did not differ between the two groups over 2 years.53 Finally, the application of FFT-A in addressing either suicide attempts or comorbid substance abuse among PBD subjects found promising results in CR studies.47,48 However, a further OT study with 10 bipolar adolescents evidenced that reduction in cannabis use was insignificant.50 In sum, there is preliminary empirical support in favor of FFT-A as an adjunctive treatment for PBD.44 However, studies with a rigorous methodology should still corroborate its potential benefits.
Family-focused therapy for youth at high-risk (FFT-HR)Rationale. High EE in families has not been postulated as the sole maintenance factor for PBD, though it has been posed as a vulnerability factor for HR-PBD subjects.54 The main methodological barrier to elucidating this issue stems from establishing what features define the clinical phenotype of HR-PBD subjects. Thereby, studies focused on this controversial issue have usually recruited adolescents who met DSM-IV criteria for depressive disorder, cyclothymic disorder or BD-NOS, with at least one first-degree relative with BD I or BD II.55
Core features and therapeutic elements. The use of FFT-A for HR-PBD requires some modifications in how the therapy is administered. Unlike FFT-A for PBD, 12 sessions are delivered over 4 months (8 weekly sessions and 4 fortnightly sessions). The treatment is also integrated with three modules, although with some differences about their goals: (i) “psychoeducation” to increase the family's ability to recognize the escalation of early subsyndromal symptoms and working with the adolescent toward stabilization of daily routines and sleep/wake cycles; (ii) “communication enhancement training” through role-playing for decreasing aversive parent–adolescent interactions, especially criticism and hostility and (iii) “problem-solving skills” to learn coping strategies for dealing with general stress.56
Empirical support. Compared to PBD, empirical data on FFT-A for HR-PBD is limited, comprising one OT and one RCT. For instance, an OT with 13 outpatient adolescents (mean age 13.4) showed low rates of attrition (15%) and significant improvements in depression, hypomania, and psychosocial functioning over 1 year of follow-up.56 Another RCT with 40 adolescents with HR-PBD (mean age 12.3) who were randomly assigned to either FFT-HR (n=21) or an education control group (two family sessions) (n=19) proved that FFT-HR participants tended to recover more quickly from their initial mood symptoms, had more weeks in remission, and manifested an improved trajectory for remission of manic symptoms across 1 year follow-up.18 Strikingly, the impact of the treatment was greater among adolescents in high EE (vs low EE) families. In sum, there is preliminary evidence supporting FFT-A for HR-PBD. However, higher number of RCT with larger sample size is needed.
Cognitive-behavioral therapy for adolescents (CBT-A)Rationale. As noted in the CFF-CBT section, PBD is characterized by affective dysregulation, deficit in working memory, lack of insight, and social cognition disabilities. Overall, these factors hinder both psychosocial functionality (e.g., poor academic achievements, impaired peer relationships) as well as remission of the symptomatology (e.g. subthreshold manic or depressive symptoms).33,34 These concerns must encourage psychological interventions aimed at targeting cognitive-affective features related to PBD, mostly in an individual format instead of a familiar setting, due to the adolescent need for independence.
Core features and therapeutic elements. CBT-A comprises 12 sessions of 60min over 3 months mostly delivered individually (parents attend two sessions). CBT for adolescents with BD includes therapeutic elements of standard CBT, namely: psychoeducation, mood charts, problem-solving skills, relaxation, reframing negative thoughts, role-playing, and assertiveness. The main goals are (i) improving psychopharmacological compliance; (ii) stabilizing routines (sleep–wake cycle); (iii) ameliorating communication within family and peer relationships and (iv) enhancing self-monitoring of mood.16
Empirical support. Unlike CBT for ABD,57 research on CBT-A for PBD is scarce, amounting to one OT.16 A study with 16 PBD adolescents aged 10–17, who were allocated to CBT (n=8) or non-psychosocial treatment condition (n=8). The CBT group showed a reduction in both manic and depressive symptoms over 2 months of follow-up.16 Likewise, retention across the course of treatment was adequate (only one dropout in the CBT group). In sum, evidence of CBT-A for PBD is insufficient and findings should be replicated in RCT.
Interpersonal and social rhythm therapy for adolescents (IPSRT-A)Rationale. Prospective studies have found that sleep impairment plays a substantial role in both the maintenance (relapses) and the onset (early marker) for PBD in adolescence.58 Sleep problems are associated with difficulties in regulating affect and impulsivity.59 One of the most prominent causes of sleep–wake disturbances are life events, particularly interpersonal problems.60,61 Hence, multicomponent interventions focused on circadian rhythms as well as on interpersonal themes are needed for managing adolescents with PBD.
Core features and therapeutic elements. IPSRT-A represents a format modified from IPSRT for adults with BD.62 It comprises 16–18 individual sessions over 20 weeks. The main objectives are to establish more regular daily social routines (meals, sleep) and resolving the interpersonal problems (unresolved grief, role transition, role disputes, or more pervasive interpersonal issues) identified through the initial appraisal.63 Psychological techniques employed include: daily charts, communication analysis, role-playing and interpersonal problem-solving skills.
Empirical support. In contrast to IPSRT for adults with BD, there are few empirical studies of IPSRT-A in PBD.64 In this context, 1 OT with 12 adolescents (mean age 16) yielded fewer manic, depressive, and general psychiatric symptoms in the post-treatment assessment.65 Participants’ global functioning increased as well. Regarding attrition rates, 11 of 12 referred patients completed the treatment. In sum, evidence of IPSRT for PBD is almost lacking and further empirical research is justified.
Dialectical behavioral therapy for adolescents (DBT-A)Rationale. Empirical research indicates that adolescents with PBD exhibit extreme positive and negative emotions,66 suggesting that an underlying feature of PBD is emotional dysregulation.32,67 Likewise, prospective studies have found that PBD subjects had a high rate of suicide attempts, almost one-third of patients over 5 years of follow-up assessments.68,69 Regarding this issue, variables such as depressive or mixed symptomatology are considered risk factors for suicidal behavior in PBD.70 This evidences the aptness of psychological interventions aimed at addressing emotional triggers for suicide attempts.
Core features and therapeutic elements. DBT-A for PBD is an adapted version of DBT for suicidal adolescents,71,72 which in turn proceeds from an original format delivered in adult subjects with borderline personality disorder (BPD).73 It comprises both family skills training and individual therapy over 1 year of treatment in an outpatient setting. The acute treatment phase (first 6 months) includes 24 weekly sessions, alternatively implemented. The second part of the treatment (7–12 months) consists in 12 supplementary sessions. The main modules applied are: mindfulness, emotion regulation, distress tolerance and interpersonal effectiveness. DBT-A intends to manage emotional dysregulation, providing adaptative tools to cope with suicidal thoughts.74
Empirical support. Despite being a promising intervention, there is a scarcity of empirical support for this type of psychological treatment in adolescent samples with BD. One OT carried out with 10 patients aged 14–18 years (mean age 15.8) showed significant improvement from pre- to post-treatment in suicidality, non-suicidal self-injuries, emotional dysregulation, and depressive symptoms.74 Moreover, rates of attrition were low (9 of 10 patients completed the treatment). An RCT which compared 14 bipolar adolescents undergoing DBT vs 6 bipolar adolescents receiving psychosocial treatment showed that the former group demonstrated significantly less severe depressive symptoms and were nearly three times more likely to demonstrate a reduction in suicidal ideation.75 In sum, although promising, DBT-A for PBD should be replicated in further RCT with larger sample size.
Motivational interviewing (MI)Rationale. Mood stabilizing medications (e.g., lithium) and second-generation antipsychotics (e.g., olanzapine) are key components in the treatment of PBD.11 However, one of the main etiological factors for weight gain among patients with BD is psychotropic treatments.76 Post-treatment weight gain is associated with worse psychiatric outcomes and increased risk of non-adherence to treatment,77,78 especially among patients worried about their body image. Therefore, taking into account the importance of body image during adolescence, the focus on eliciting intrinsic motivation for preventing or decreasing weight gain might be relevant in youth with PBD subjected to psychopharmacological treatment.
Core features and therapeutic elements. MI comprises 5 individual sessions (three 45-min in-person sessions and two 15-min phone sessions) over a 10–12 week time period. It addresses 5 specific behaviors associated with weight in youth: (i) sweet beverages consumed per day; (ii) fast food meals consumed per week; (iii) dinners eaten with at least one parent per week; (iv) media time per day (e.g., television, video games); and (v) physical activity for at least 30min per week. In MI, the clinician encourages the adolescent with BD to talk about weight-related behaviors, highlighting and exploring any discrepancies between concerns, goals, and current health behaviors. The adolescent is then guided in the creation of a change plan for each targeted behavior.17
Empirical support. Unlike MI for adult or adolescent patients diagnosed with other mental disorders, evidence for MI for PBD is almost non-existent.79,80 An exception is a CR that showed a slight reduction in BMI (body mass index) over the period of treatment (session 1=BMI 24.0; session 5=BMI 23.0).17 In sum, evidence of MI for PBD is almost lacking and needs more empirical research.
Discussion and conclusionsThis systematic review has intended to exhibit main findings and research about psychosocial treatments as an adjunctive intervention for PBD. Despite being an incipient field of research, psychosocial treatments for PBD have steadily increased over the last 10 years. Some treatments have obtained more empirical support than others, especially MF-PEP for children as well as FFT for adolescents. According to current guidelines,81 both treatments could be considered “possibly effective treatments” for PBD. Results for these therapies include improvements in both mood psychopathology and functionality. Likewise, CFF-CBT has attained some empirical validation from OT studies, although it may be characterized as a “treatment in experimental phase” because of a lack of RCT. The remaining treatments (CBT-A, IPSRT-A, DBT-A, MI) need further empirical research, both OT and RCT. In contrast to the uneven effectiveness of these therapies, treatments for PBD have conclusively proven their feasibility and acceptability, being deemed satisfactory for the participants as well as achieving low rates of attrition.82
Regardless of the psychosocial treatment displayed, there are some common features across these interventions. For instance, most of the treatments highlight the benefits of a psychoeducation module, irrespective of it being considered a primary or a secondary goal. Likewise, a significant percentage of these interventions focus on youth and parents as complementary targets, notably among children with PBD. This is due to the fact that youth and parents must both cope with an unknown illness that alters family interactions. A comprehensive etiopathogenic model regarding main psychosocial risk factors involved in PBD is still lacking. Some theories highlight the role of affect dysregulation, whereas others suggest the role of high EE in families. Overall, these varied approaches depict a heterogeneous framework to address PBD from a psychological perspective.83
From a clinical perspective, a major key component for improving non-adult bipolarity seems to imply psychoeducation in youth and in their parents as well. For instance, when comparing those RCT with larger sample sizes and follow-up assessments,30,53 the psychoeducation module may account for the improvements on time to recovery, recurrence and time in remission, irrespective of other techniques included (e.g., “communication skills” or “problem-solving skills”). One possible explanation could be that these complementary techniques may be adequate for a subset of PBD youth rather than for the whole PBD sample. Hence, an accurate assessment for the potential risk factors for each sample may lead to an adapted treatment focused on these specific vulnerability factors involved. Accordingly, research should not merely measure “family interactions” for each sample, even more it should include complementary assessments such as executive functioning capabilities. Another potential explanation for our initial assumption could be that parental distress and communication deficits were not primary etiopathogenic factors in PBD. Rather, these problems may be secondary consequences when families must cope with a serious mental illness. Thus, psychoeducation may provide the main psychological tools to deal with this family burden. To elucidate whether or not these other techniques may be helpful, we underline two possible ways. First, to include a control group based on psychoeducation techniques across similar number of sessions than the clinical groups. Second, to conduct dismantling studies that enable us to identify the program's key ingredients.
Limitations and directions for future researchOne of the most prominent methodological shortcomings identified in the psychological treatment of PBD is the failure to utilize both adequate sample size and control groups to assess the effectiveness of these interventions. Ultimately, these methodological constraints undermine the statistical power and the internal validity of results obtained. Therefore, RCT with larger sample sizes are warranted. Moreover, empirical evidence from some of these therapies has been quite consistent at short- and mid-term. However, follow-up studies at long-term (more than 12-months) are scarce and have usually failed to obtain benefits from these therapies when compared to control conditions. Hence, RCT (vs OT) with larger follow-up assessment are needed to verify whether these therapies may lead to a stable course of PBD over time. Furthermore, empirical validation of these therapies from several or different research teams is especially needed. Research about psychological treatments for PBD also has limitations regarding its ecological validity. In this context, empirical studies engaging PBD subjects usually exclude or overlook the widespread psychiatric comorbidity in these types of clinical samples, for example substance misuse, anxiety disorders, or conduct disorders.84–87 Thus, appropriate therapeutic approaches must be encouraged in order to manage these comorbidities.88 Moreover, there are some psychological variables not taken into account so far. For instance, psychosocial interventions that include psychoeducational programs have not addressed whether these modules may improve insight into illness and psychopharmacological compliance. Future research among youth with PBD must investigate this question. Likewise, there are no empirical studies about cognitive rehabilitation for neurocognitive impairments in PBD,89–91 so the possible contributions from these therapies remain unclear. Future research must establish to what extent these cognitive therapies may obtain results similar to adult samples.92 Finally, psychosocial interventions among HR-PBD youth are scarce.93 Further clinical trials focused on this cohort are warranted.94
Conflicts of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Frías Á, Palma C, Farriols N. Intervenciones psicosociales en el tratamiento de los jóvenes diagnosticados o con alto riesgo para el trastorno bipolar pediátrico: una revisión de la literatura. Rev Psiquiatr Salud Ment (Barc). 2015;8:146–156.