Ectopic breast tissue can arise at any point along the primitive milk line, which runs from the axilla to the groin. The incidence of ectopic breast cancer ranges from 0.2% to 0.6%. We report the case of a 60-year-old woman with a history of left mastectomy for breast cancer one year prior to presentation, who presented with bilateral vulvar erosion found to be a moderately differentiated adenocarcinoma on biopsy. The extension workup being negative, a radical vulvectomy was performed. The postoperative course was uneventful, and the specimen's pathologic study revealed a vulvar localization of non-specific invasive breast carcinoma. It was positive for estrogen receptor and human epidermal growth factor receptor 2/neu, and negative for progesterone receptor. Adjuvant chemoradiotherapy was given to the patient. There is no dedicated guideline for both diagnosis and management of this particular tumor; the treatment is similar to that of orthotopic breast cancer.
El tejido de mama ectópico puede presentarse en cualquier punto de la línea de la leche primitiva, que discurre desde la axila a la ingle. La incidencia de cáncer de mama ectópico oscila entre el 0,2 y el 0,6%. Reportamos el caso de una mujer de 60 años con historia de mastectomía izquierda por cáncer de mama un año antes de la presentación, que acudió con erosión bilateral en la vulva, que fue considerada un adenocarcinoma moderadamente diferenciado en la biopsia. Siendo negativas las pruebas complementarias, se realizó una vulvectomía radical. El curso postoperatorio transcurrió sin incidentes, y el estudio de la muestra patológica reveló la localización en la vulva de un cáncer de mama invasivo no específico, que fue positivo para receptor de estrógenos y receptor del factor de crecimiento epidérmico humano 2/neu, y negativo para el receptor de progesterona. Se administró quimioterapia adyuvante a la paciente. No existen directrices especializadas para el diagnóstico y manejo de este tumor particular, siendo su tratamiento similar al del cáncer de mama ortotópico.
Ectopic breast tissue can arise at any point along the primitive milk line, which runs from the axilla to the groin, as a result of incomplete involution of the ectodermal ridges of the breast during embryologic development.1 The axilla and vulva are the two most common sites of ectopic breast tissue. Like the breast, ectopic mammary tissue can be subject to malignant degeneration; invasive ductal carcinoma being the predominant histological subtype.2 The incidence of ectopic breast cancer ranges from 0.2% to 0.6%.3 Cancerous transformation of this ectopic breast tissue can be challenging both diagnostically and therapeutically. Here, we report a rare case of a metachronous vulvar ectopic localization of breast cancer.
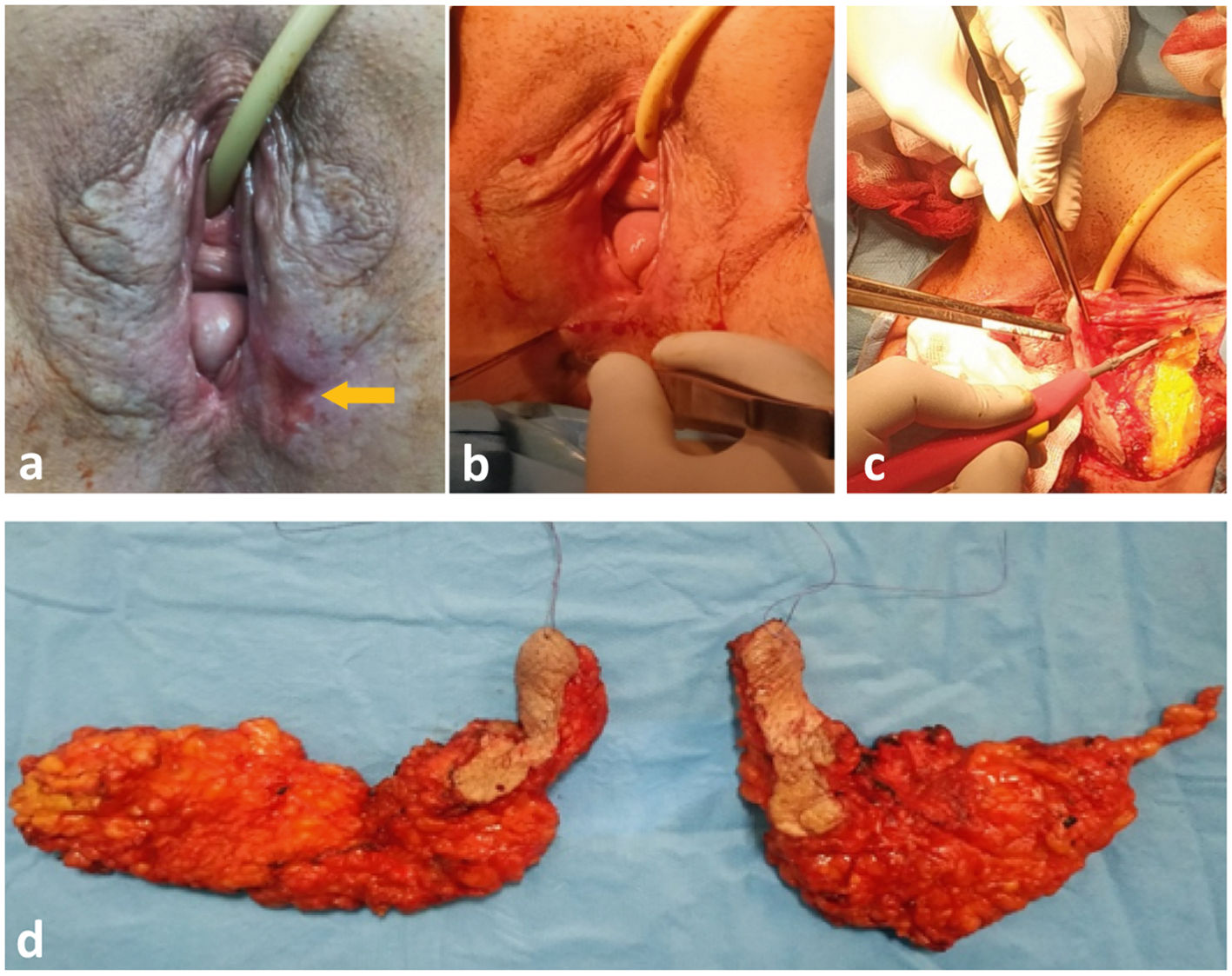
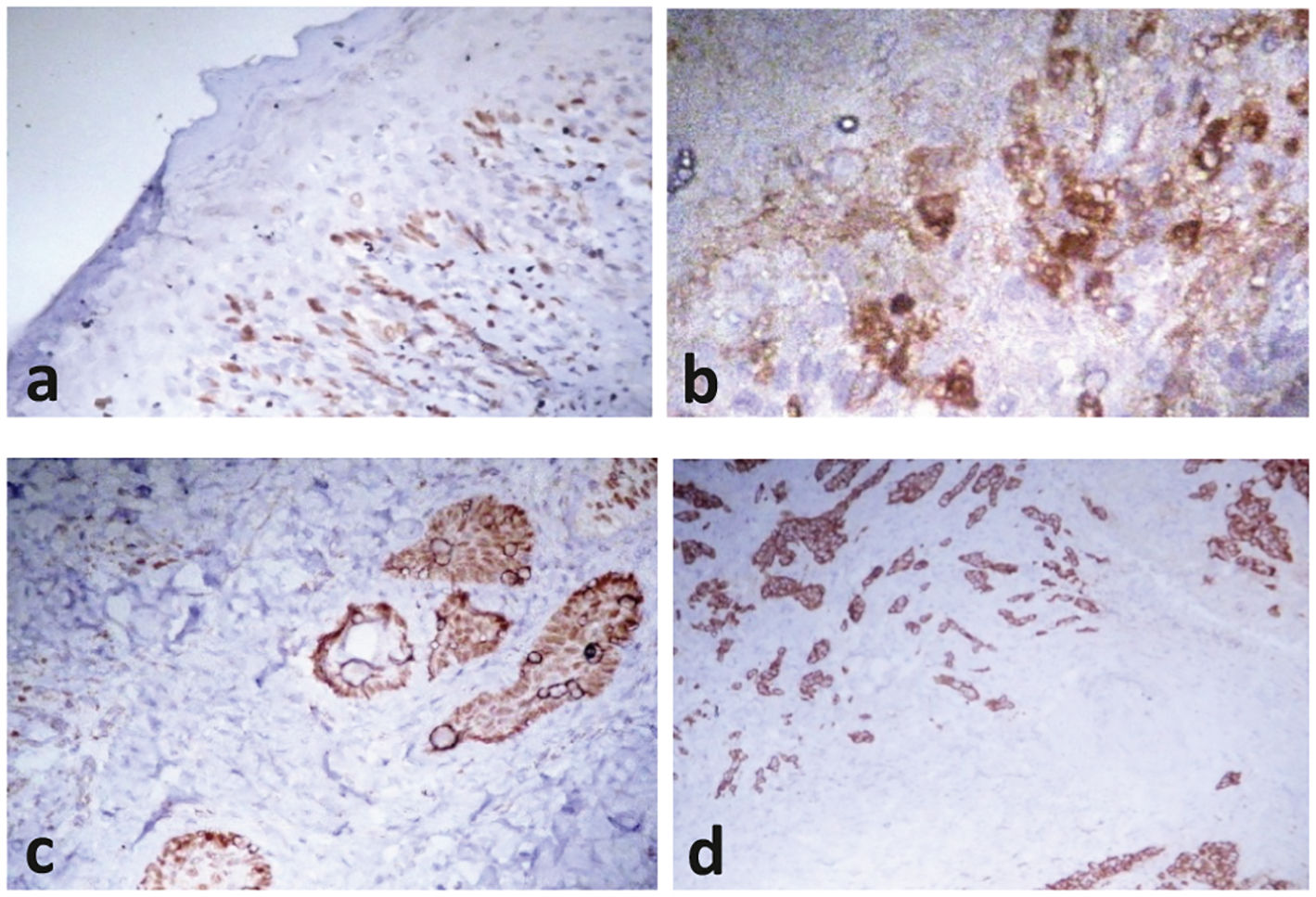
Case reportA 60-year-old postmenopausal woman with a history of left mastectomy with sentinel lymph node mapping for ductal carcinoma; in whom bilateral vulvar erosion was found corresponding to a moderately differentiated adenocarcinoma (Fig. 1a). Pelvic MRI showed a right median and micronodular lineal diffusion hypersignal confined to the vulva, with absence of lymph nodes. The PET-CT showed no other evidence of metastatic disease. The diagnosis retained at that time was metachronous vulvar metastasis of breast cancer. A bilateral radical vulvectomy without inguinal lymph nodes dissection was performed (Fig. 1b,c,d). The postoperative course was uneventful, and the specimen's pathologic study confirmed the diagnosis of a vulvar localization of non-specific invasive breast carcinoma with pagetoid aspect. Resection margins were free of infiltration; the tumor was positive for estrogen receptor and human epidermal growth factor receptor 2/neu, and negative for progesterone receptor on immunohistochemical findings (Fig. 2). After a multidisciplinary discussion, adjuvant chemotherapy with Paclitaxel and Trastuzumab was prescribed. The patient was already treated with an aromatase inhibitor, anastrazole 1 mg daily orally. In addition, radiotherapy of the operative site and the inguinal area was recommended. No local or distant recurrence was observed at 12 months follow-up.
(a) Bilateral vulvar lesions with left ulceration (yellow arrow).
(b) Incision drawing.
(c) Subcutaneous dissection of the left vulva.
(d) Bilateral vulvectomy specimen oriented by two wires. (For interpretation of the references to color in this fig. legend, the reader is referred to the web version of this article.)
Ectopic breast tissue is observed in about 2–6% of women and 1–3% of men.1 It can occur at any site along the milk line due to incomplete embryologic regression of the mammary ridge, which extends from the axillary to the inguinal folds bilaterally at the sixth week of gestation.1,4 The axilla is the most common site of ectopic breast tissue, closely followed by the area just below the orthotopic breast. Besides these areas, its occurrence in the acromial or scapular region, the vulva, the thoracic and abdominal midline remains rare.5 The ectopic breast tissue is exposed to almost all of the physiological and pathological conditions usually observed in the pectoral breast, including carcinogenesis.6 Hartung, in 1872, reported for the first time the case of a completely developed mammary gland on a thirties old female's left labia majora.7,8 It is to Greene that we owe the first report of primary ectopic breast cancer of the vulva in 1936.9 The presence of ectopic breast tissue in the vulva is explained by a theory other than the one mentioned above; a mammary-like variant of skin glands in the anogenital region was described by Van der Putte.10 Their similarity to the mammary parenchyma gives them a comparable neoplasic potential. Any of the various histologic subtypes of breast cancer may occur in the vulva, including infiltrating ductal, lobular, mucinous, and mixed ductal and lobular carcinomas.5 Mammarylike adenocarcinomas of the vulva are considered locally aggressive tumors that frequently relapse with lymph node metastases in around 60% of cases.11 To consider the lesion as primary vulvar origin, Irvin et al. have defined precise criteria.12 If the primary ectopic breast carcinoma is a rare event, the possible association with synchronous or metachronous breast cancer remains even rarer, with less than twenty cases published in the literature.4,5 Due to the rarity and atypical presentation of the disease, the diagnosis is often delayed.4 Management of this rare entity is challenging because of a lack of specific guidelines. Therefore, the treatment is similar to that of breast cancer. It should consist of an individualized combination of surgery, chemotherapy, monoclonal antibody therapy, radiation, and adjuvant endocrine therapy, as appropriate.5 Surgery varies from broad local excision to radical vulvectomy with bilateral inguinofemoral lymph node dissection.13 The role of lymphadenectomy is still unclear,14 and the sentinel inguinal lymph node sampling seems to be an interesting alternative.15,16 In our patient, we did not perform an inguinal lymph node dissection because of the negativity of the extension workup on pelvic MRI and PET-CT. On the other hand, the inguinal region was irradiated bilaterally. Data seem to show that postoperative pelvic radiation provided a clear benefit in terms of recurrence-free survival and cancer-related death compared to inguinal and pelvic lymphadenectomy.17 Adjuvant treatment with anthracycline-based chemotherapy, hormonal therapy, and radiation reduces the risk of local and distant recurrence with a median survival of 22 months.18 Prognostically, it is crucial to know whether the vulvar tumor is a synchronous or metachronous ectopic breast cancer or a metastasis of a known breast cancer in which case it will be a stage IV with a 5-year survival of around 20%.13 Follow-up by clinical exam, imaging and tumor marker tests is recommended regularly, although the duration of surveillance in remission patients is still debated.19
Clinicians must be aware of this rare entity to avoid treatment delays. Any hypoechogenic subcutaneous nodule found along the milk line without inflammatory signs should suggest an ectopic breast carcinoma. Accurate characterization via detailed immunohistochemical analysis is required. There is no dedicated guideline for both diagnosis and management of this particular tumor. Treatment is that of similarly staged orthotopic breast cancer.
FundingNo funds, grants, or other support was received.
Ethical disclosuresThe authors declare that they have followed their center's protocols on the publication of patient data
Authors contributionsChemseddine Chekman, Hani Bendib and Amina Mekerba were involved in conception, data collection and article drafting. All authors were involved in final approval of the article.
Patient consentThe authors declare that they obtained the patient's consent for publication of the article.