Dermatofibrosarcoma protuberans (DFSP) is an uncommon skin-depending soft tissue neoplasm which behaves biogically with intermediate malignancy. Although it rarely develops metastasis, it provokes high morbidity due to its great ability to infiltrate nearby tissues and its high recurrence rate after surgical resection. It is most prevalent between 20 and 40 years-old, and males are more commonly affected than females. The best treatment consists of surgical resection, ensuring wide margins including sublay fascia.1
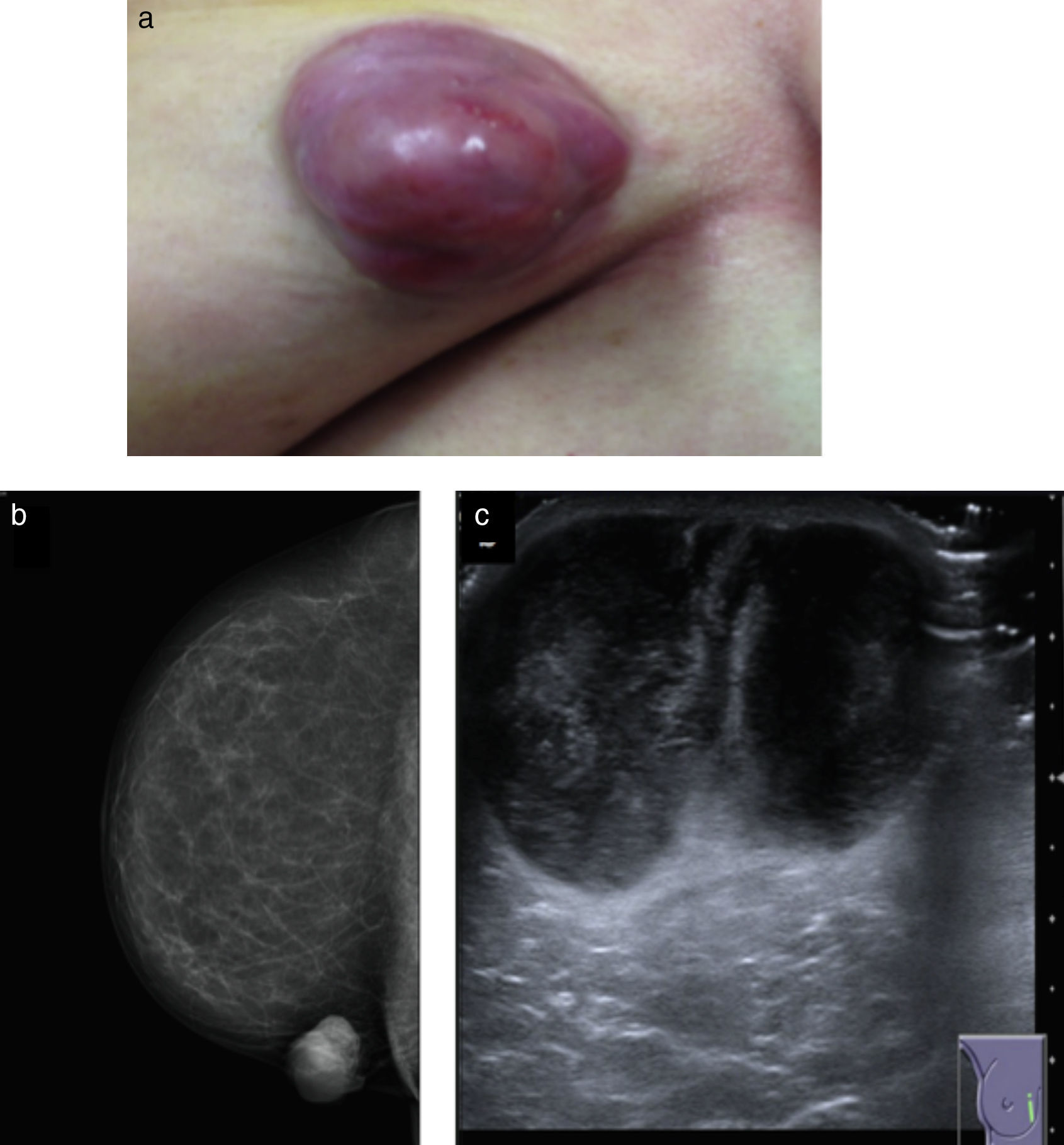
A 56 year-old female consults for right breast tumor. Physical examinations shows non-ulcerated, well-circumscribed, multilobe, nodular lump in the internal quadrants of the right breast (Fig. 1a). Radiological examinations are conducted. The mammography shows a dense, well-circumscribed, nodular lesion with a cutaneous cover that is not associated to calcifications or alterations of the breast architecture (Fig. 1b).
(a) Well-circumscribed, multilobe, nodular tumor. (b) Right breast mammography: dense, well-circumscribed, nodular lesion with a cutaneous cover, that is not associated to calcifications or alterations of the breast architecture. (c) Ultrasound: two adjacent heterogeneous, nodular masses that on the whole, measure 32×36×48mm.
The ultrasound identifies two adjacent heterogeneous, nodular masses that on the whole, measure 32×36×48mm. No definite alterations or abnormalities are shown in the axillary lymph nodes (Impression BIRADS 4) (Fig. 1c). Microscopic examination illustrates high cellular density tumoral lesion that infiltrates adjacent fat tissue. Cellularity is formed into short intersecting beams with storiform focal formation without necrosis or mitosis. It also shows elongated cells with scant cytoplasm and monomorphic nuclei (spindle cell). The cells extensively express vimentin and CD34, and actin is focally expressed. No immunoreactivity for PS-100, desmin, P63, AE1-3 cytokeratin and estrogen is observed. The proliferation index (Ki-67) is 15%. In conclusion, this is a mesenchymal tumor morphology and immunohistochemistry consistent with DFSP.
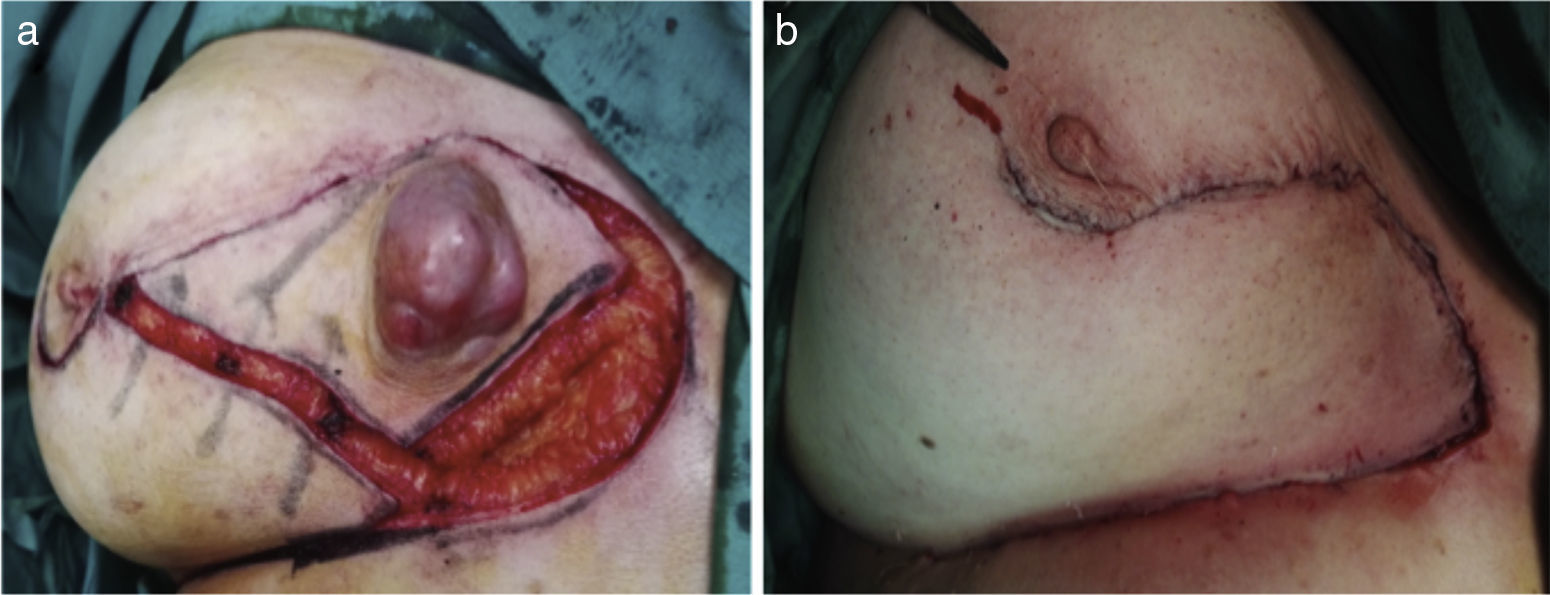
In multidisciplinary committee, it was decided that the best treatment consisted of surgical resection with wide margins including pectoral fascia. To repair the defect, an inferior rotation oncoplasty was employed. The pathology study confirmed the diagnosis and disease-free margins (Fig. 2a and b).
DFSP was first described by Darier and Ferrand in 1924. It constitutes less than 0.1% of all malignant tumors and approximately 1% of all soft tissue sarcoma.2,3 It originates in the dermis, and has great ability to infiltrate the subcutaneous tissue, the fascia and the sublay muscle. Its clinical behavior is defined by its progressive growth and a tendency to local recurrence. However, it rarely metastasizes (1–4%), developing mostly lung metastasis, and less frequently affecting lymph nodes.4,5 It is usually located in the chest and abdomen (40–50%), 30–40% in the limbs proximal portion, and 10–15% is located in head and neck.
It has been demonstrated in genetic studies that 90% of these tumors present chromosomal translocation.5
The standard treatment consists of local resection with 2–3cm margins, in order to secure free resection edges. In this case, the tumor affected the internal quadrants of the breast, where any surgical treatment causes important esthetic deformity, so an inferior rotation flap was decided to cover the defect and accomplish an adequate esthetic result.
When the surgical margins are affected, local recurrence happens in approximately 70%, most of them during the first three years after surgery.6,1 However, if resection margins are not affected, it recurs in up to 30%. The high rate of local recurrence is explained by the eccentric growth when the tumor reaches the subcutaneous tissue, where it infiltrates as tentacles far from its initial location, which go clinically unnoticed and may remain concealed if an exhaustive pathology exam is not implemented. The main disadvantage to surgical resection with wide resection margins is that the removal of ample areas of non-invaded tissue implies great morbidity.
That is why Mohs’ micrographic surgery is established as the best surgical technique, enabling the entire study of the margins and limiting the resection of healthy tissue. This approach obtains the highest percentages of healing, reaping a local recurrence rate lower than 5%.7 Patients with locally advanced or metastatic DFSP require neoadjuvant treatment, and in these cases, imatinib has been successfully employed.8
To conclude, dermatofibrosarcoma is a slow-growing uncommon skin neoplasm, which presents high rates of recurrence but that rarely develops metastasis. The best treatment consists of surgical extirpation with extensive resection margins. It is recommended a long term follow-up due to the high probability of relapse.