Clinical Nurse Specialists in the Oncoplastic Breast Cancer Service in the United Kingdom play an essential role in the diagnóstico, treatment and follow up of patients with breast cancer. At Nottingham Breast Institute, they are divided in Breast Care Nurses and Nurse Practitioners with completely different roles. They are able to obtain high level of confidence with the patient usually impossible to reach by the rest of the Breast Team. Through this article we will discuss the different roles and advantages of these essential posts that have increased the standard of breast cancer care in the UK.
Las enfermeras clínicas especializadas del Servicio de Cáncer de Mama Oncoplástico del Reino Unido desempeñan un papel esencial en el diagnóstico, tratamiento y seguimiento de las pacientes con cáncer de mama. En el Instituto de la Mama de Nottingham, se dividen en enfermeras de atención a la mama y enfermeras especializadas con funciones completamente diferentes. Son capaces de obtener un alto nivel de confianza con la paciente, normalmente imposible de alcanzar por el resto del equipo de mama. A través de este artículo hablaremos de las diferentes funciones y ventajas de estos puestos esenciales que han aumentado el nivel de la atención al cáncer de mama en el Reino Unido.
The Nottingham Breast Institute (NBI) sees and treats approximately 800 new breast cancers per year, both screening and symptomatic patients. It is one of the biggest breast units in the United Kingdom and all services and investigations are based at the City Campus, of the Nottingham University Hospitals.
The cancer pathway can be complex, lengthy and fragmented and needs a wide variety of Multi-Disciplinary Team (MDT) members in a range of care settings. The Clinical Nurse Specialist (CNS) is pivotal in providing quality patient centred care, focusing on individual tailored treatment.1 The CNS should be educated to degree level, have acquired specialist knowledge, skills, competencies and experience within a specialist field, be a clinical expert and resource for other team members. The CNS's role is not just clinical; the role should also include leadership, educational, developmental and advocacy components.2 The National Cancer Patient Experience Survey in England has demonstrated that cancer patients feel they were involved as much as they wanted to be in decisions about care and treatment.3
Within the NBI the CNS role is made up of two separate roles; the Breast Care Nurse (BCN) and the Nurse Practitioner (NP). Their roles complement each other well in terms of ensuring the breast cancer patients' individual needs and goals are central to the care they provide. In achieving this, their roles are very different in that they see, support and have input in different parts of the patient's pathway.
The BCNs and NPs roles within the NBI are complex and multi-faceted requiring them to work autonomously and frequently make complex clinical decisions. The BCNs role allows them to be in a unique position where they are able to provide the patient with complete continuity of care, including; meeting the patient before diagnóstico, during diagnóstico in a supportive role, during treatment and for follow up.4 All patients who have a diagnóstico of breast cancer will meet a breast care nurse who will move with them through their breast cancer journey. This makes the BCN role vital in the patient's journey.
The role of the NP within the NBI was initially established more than twenty years ago and was considered to be innovative at the time as it was a role traditionally performed by medical practitioners. The NPs within our unit must all undertake a robust in house training programme in order to undertake the role. Practising NPs work to a strict set of guidelines and protocols to aid the clinical decision making and maintain patient safety along with regular performance reviews.5
The NP's role has evolved throughout the years to encompass the growing needs of the unit. At present there are eight NPs who all undertake solely nurse led symptomatic and screening recall clinics which involves a triple assessment, this includes; a clinical breast exam, imaging, potentially a biopsy of all presenting patients, from a breast cancer perspective this is the start of the patients breast cancer journey. The BCN in the NBI will often meet their patient pre diagnóstico in these new referral or screening clinics during investigations. They will share information, contact details, next steps in the pathway and support the patient during this distressing time.
An MDT meeting is then held to discuss the patient's potential treatment plan, followed by their clinic appointment where they will meet the same BCN who will become their keyworker. At this point in the pathway the main focus of the BCN role is to provide psychological support as well as any symptom control. It is vital that the BCN can provide information to the patient regarding their disease and potential treatments as well as facilitate the clinical choices given by the surgeon.
Once it's been decided that a patient's first choice in the treatment pathway is surgery, this patient's case will be discussed in a specifically dedicated oncoplastic forum. Members of this team include a radiologist, breast surgeon, plastic surgeon and a BCN. This forum has been uniquely designed to discuss all surgical options. Each case is discussed amongst the team, clinical details are presented, photos of the individual are viewed alongside the patient's social situation and plans are formulated in terms of the most suitable surgical options suited to that patient.
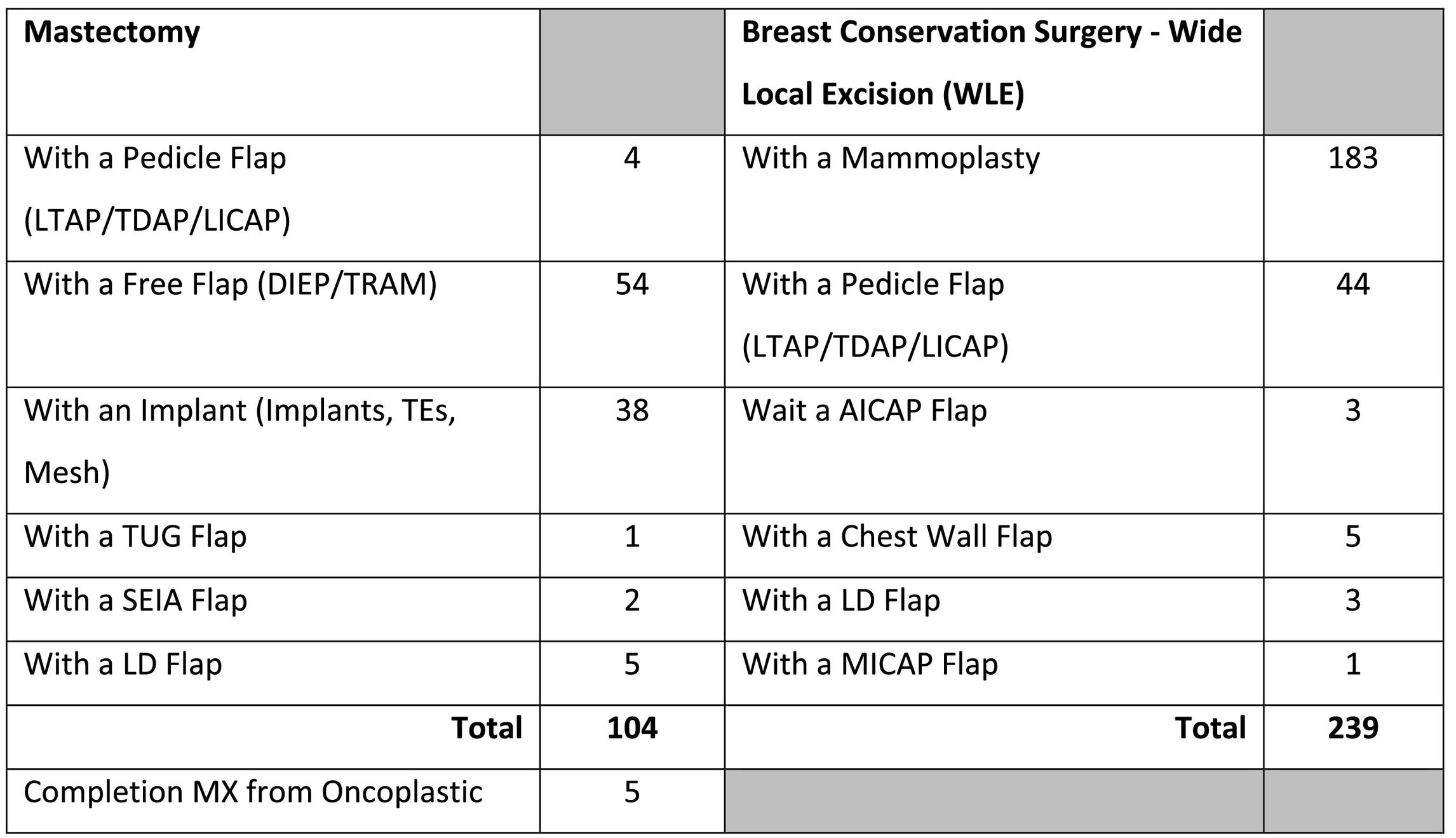
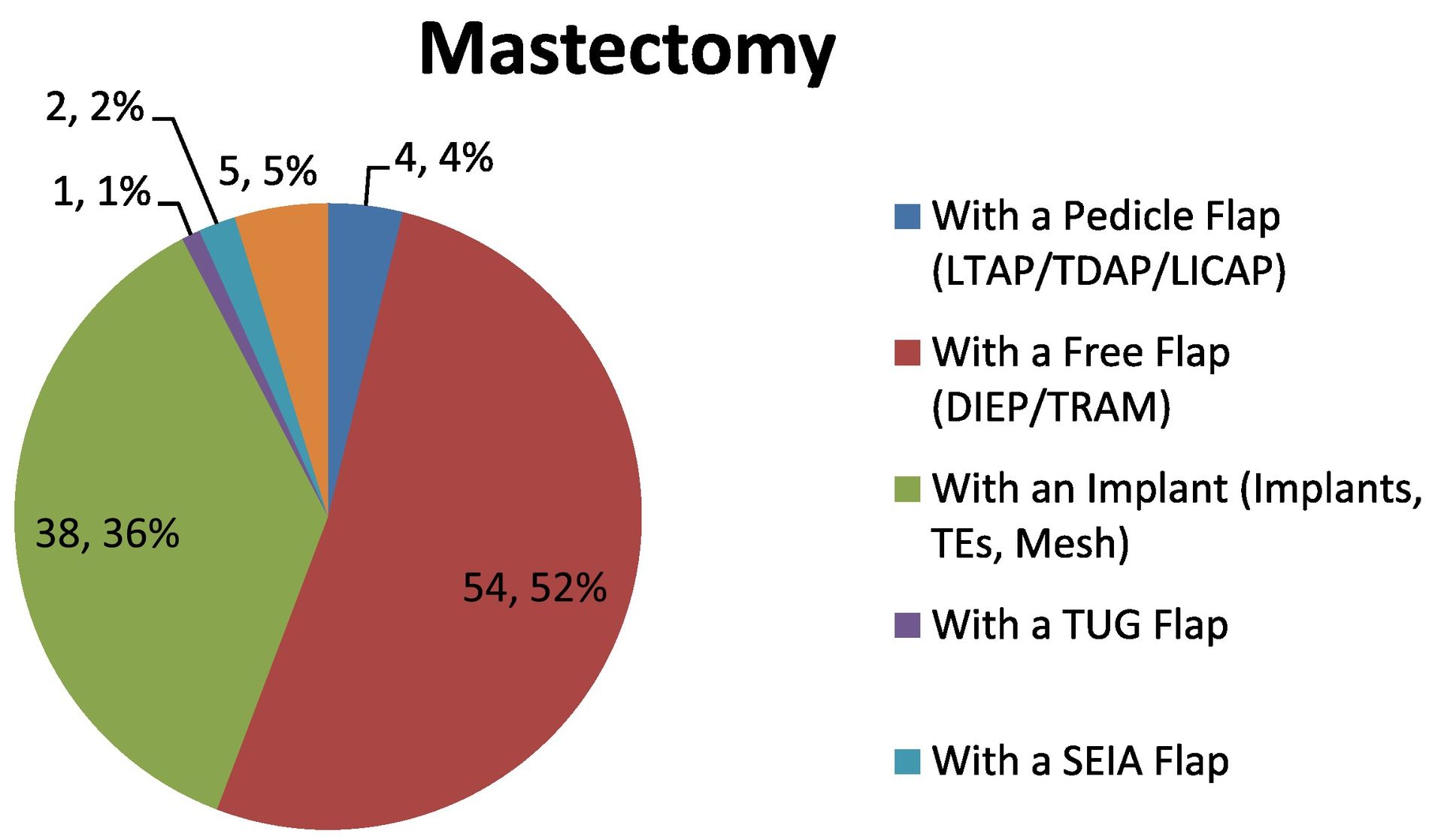
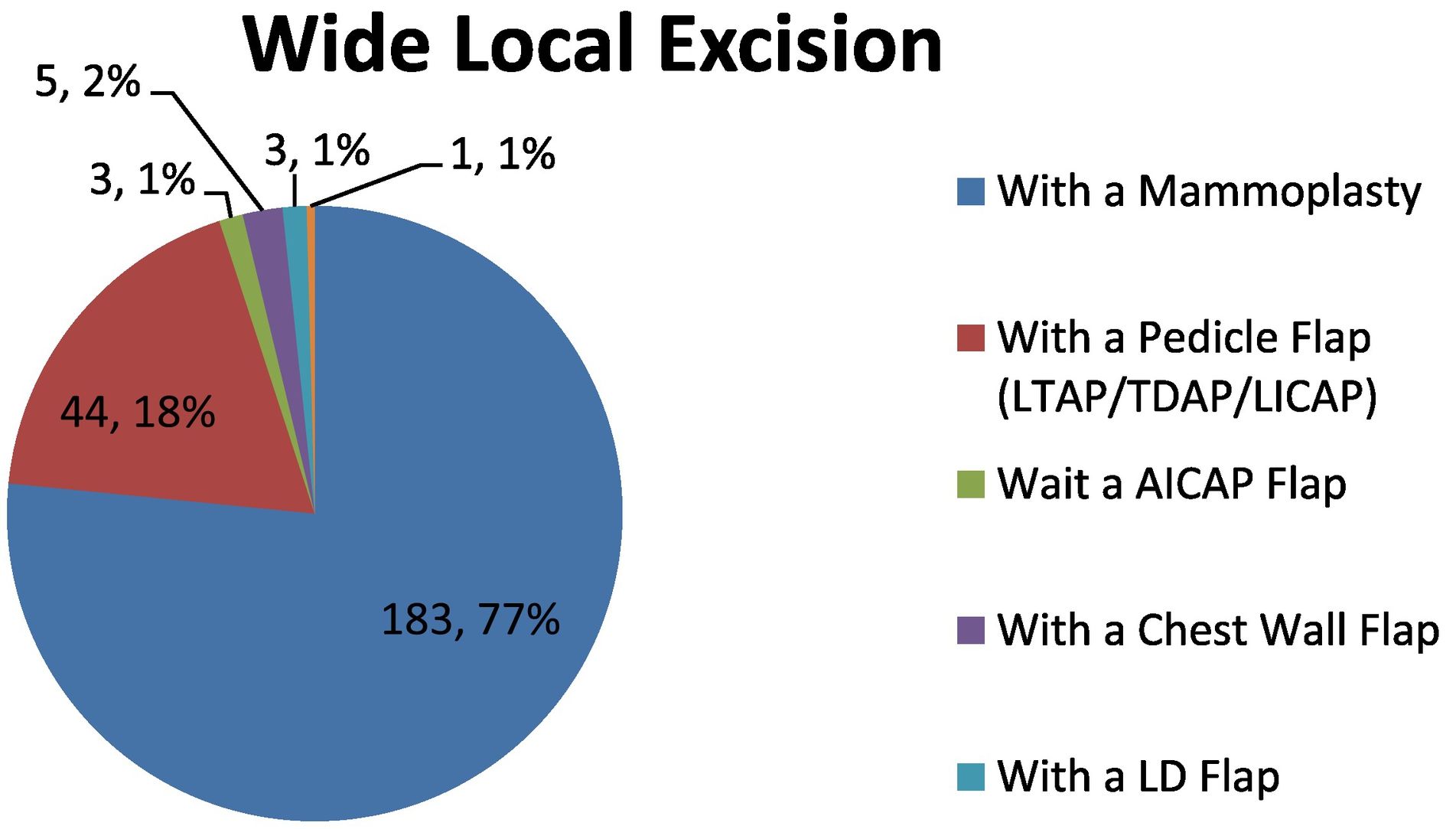
Generally 3–4 choices of surgery are identified. These range from a full mastectomy to Breast Conservation Surgery (BCS). A full range of oncoplastic techniques will be available. Following a mastectomy, options range from Tissue Expanders (TE) to implants; Latimus Dorsi (LD) flap, Deep Inferior Epigastric Perforator (DIEP) free flap, Transverse Rectus Abdominis Muscle (TRAM) free flap, Transverse Upper Gracilis (TUG) flap, Superficial Inferior Epigastric Artery (SIEA) flap or Inferior Gluteal Artery Perforator (IGAP) flap. Following BCS, options include; mammoplasty reconstruction, Anterior Intercostal Artery Perforator (AICAP) flap, chest wall flap, mini LD flap, Medial Intercostal Artery Perforator (MICAP) flap and pedicle flaps; Lateral Thoracic Artery Perforator (LTAP), Thoracodorsal Artery Perforator (TDAP), and Lateral Intercostal Artery Perforator (LICAP).
All the above techniques can be offered immediately or as a delayed option, depending on patient's wishes, stage of disease and likely adjuvant treatment choices. Following on from this forum, the patient is seen in person in clinic to discuss their options in more detail. Generally each patient is seen by 2–4 surgeons, where a thorough clinical examination is carried out, and then a full explanation is given to why each option could be a good choice for this individual.
The BCN is pivotal to this stage in the pathway as although the BCN has already met their patient at diagnóstico, their support is invaluable at this stage. Further support and advice is offered, ascertaining what the patient's preference is and their level of understanding of all choices and techniques will be assessed. Holistic components, like the patient's expectations of cosmetic outcome and lifestyle activities important to the patient will be highlighted and discussed thoroughly. Photos of options can be viewed; including the whole range of each surgeon's previous work. These photos include likely complications resulting in poor cosmetic outcomes so the patient has a realistic expectation of all surgical options. The BCN will also be able to show different prostheses, implants and TEs, drains and bras to help with the decision making process. This appointment is very lengthy and complex. However it is essential for the patient to meet the surgeon, discuss expectations and explore all the likely post op issues with recovery. Ideally a date for surgery will be sourced at this appointment. To accommodate target requirements, a 31 day target will need to be achieved from the date of treatment decision and a 62 day target is essential from the date of referral into service. Surgery can be carried out either as a day case or as an in-patient, dependent on the patient's past medical history, social network and any post op care that is required.
Following on from this appointment it is very common that the BCN meets with the patient again to go through any necessary information required at this stage. Occasionally this consultation can be done on the phone as well. In fact, several further conversations can be essential in order for the patient to feel satisfied and confident with their decision. The BCN can put the patient in touch with a previous patient from the NBI who has had a certain type of operation, similar to what they have been offered. Attention to detail should be made in matching the individuals, taking into account the patient's age, race and social status. If this is unachievable, the BCN can recommend external organisations like Breast Cancer Care, which is a national charity that offers a similar service.
When both the patient and BCN are confident that a final decision has been made, the BCN then feeds back to the individual surgeon with the confirmed plan. This decision made by the patient can often differ from what has been presented by the surgeon, due to the patient feeling the surgery and recovery may go against their chosen lifestyle, or in fact they want to keep surgery simple and avoid excessive lengthy operations if cosmetic outcome isn't a concern for them. The BCN will support the patient's decision even if it differs from the desired options made at the oncoplastic forum. As the patient's advocate, “proactively speaking for another to ensure certain needs or wishes are met is vital”.6
Below are the specific figures for the patients that were operated on using oncoplastic techniques at the NBI in 2019. (Fig. 1-3).
The NP provides a vital role in the management of the many complex oncoplastic procedures offered within our unit from the simple aspiration of seroma's following breast surgery to the management of complex wounds i.e. LD flap reconstruction. Within a week of surgery, the patient will have a follow up appointment with an NP for a wound review. This again is a completely nurse led clinic and has also expanded to meet the needs of the ever increasing specialised surgery offered within our unit increasing from 1 clinic per week to 3 at present. The NP's undertaking these clinics are all highly experienced and have chosen to specialise within the field of wound care as an extra facet to their role.
Three weeks post operatively the results from surgery will be discussed and a clear plan of adjuvant treatment is outlined. The BCN continues contact with the patient to aid them through this particular stage of the treatment pathway.
Following the completion of all adjuvant treatment, if a patient was then unhappy with their cosmetic image, the BCN will navigate them through further discussions with the surgeon in regard to fat transfer techniques, mastopexy procedures or any other form of corrective surgery.
ConclusionA CNS supports patients from the initial diagnostic investigations right through to discharge at 5 years, although this can be longer if the individual is under the age of 50. Psychological support is one of the biggest components of the CNS role. There are a wide range of specialist oncoplastic options available to patients at NBI and this can be a perplexing time for patients. The level of support and information the CNSs can provide is invaluable to the patients navigating through their treatment journey. The CNS is also a vital member of the MDT in making sure seamless communication is made between the patient and surgeons ensuring all holistic and psychological wellbeing needs are addressed.
The oncoplastic forum and surgery options are incredibly specialised services that we are fortunate to have within the NBI. The process involves a number of professionals across different specialities coming together for this sole purpose which they all have an investment and interest in. Without the effort of all these individuals together the oncoplastic forum would not be able to function, especially not to the standard it currently is within the NBI. We are very thankful that we are able to offer this specialised service to our breast cancer patients here at NBI.
Ethics approval and consent to participateNot applicable.
FundingThis work has not received any funding.
The authors would like to thank Amanda Bland, breast care nurse assistant, Lisa Brock, research assistant and Ben Rose-Walton, data audit manager, all of the Nottingham Breast Institute, Nottingham University Hospitals NHS Trust (NUH) for their contributions to this article.