The sequelae and the disability and dependence that follow an acquired brain injury (ABI) may result in a significant reduction in the quality of life (QoL) of those affected. The objective was to assess the QoL of a sample of Spanish patients with an ABI and analyze the influence of certain sociodemographic and injury-related variables on their QoL. Method: The sample comprised 421 adults (60% male; Mage = 53.12; SD = 14.87). Professionals and relatives assessed the patients’ QoL through the CAVIDACE scale, an ABI-specific tool based on the eight-domain QoL model. Results: Univariate analyses showed statistically significant differences in the QoL scores in several sociodemographic (age, civil status, education level, prior employment status, type of home, level of supports, loss of legal capacity, recognized dependence, and degree of dependence) and injury-related (time since the injury, location of the injury, and presence of post-traumatic amnesia) variables. The multiple linear regression showed that loss of legal capacity, time since the injury, prior employment status, location of the injury, and degree of dependence were significant QoL predictors. Conclusions: These findings provide knowledge for the development of programs aimed at reducing the negative impact of ABI on QoL.
Las secuelas, discapacidad y dependencia que siguen al daño cerebral adquirido (DCA) pueden resultar en una reducción significativa en la calidad de vida (CV) de los afectados. El objetivo fue evaluar la CV de una muestra española con DCA y analizar la influencia de variables sociodemográficas y relacionadas con la lesión en su CV. Método: La muestra comprendió 421 adultos (60% hombre; Medad = 53,12; DT = 14,87). Profesionales y familiares evaluaron la CV de los pacientes a través de la escala CAVIDACE, una herramienta específica para DCA basada en el modelo de CV de ocho dimensiones. Resultados: Los análisis univariantes mostraron diferencias estadísticamente significativas en las puntuaciones de CV en variables sociodemográficas (edad, estado civil, nivel educativo, situación de empleo previa, tipo de hogar, nivel de apoyos, incapacidad legal, situación de dependencia reconocida y su nivel) y relacionadas con la lesión (tiempo desde la lesión, localización de la lesión y presencia de amnesia postraumática). El análisis de regresión múltiple mostró la incapacidad legal, el tiempo desde la lesión, la situación de empleo previa, la localización de la lesión y el nivel de dependencia como predictores significativos de CV. Conclusiones: Estos hallazgos proporcionan conocimiento para el desarrollo de programas dirigidos a reducir el impacto negativo del DCA en la CV.
Acquired brain injury (ABI) is caused by a sudden injury to the brain that occurs as a result of a cerebrovascular accident (CVA), traumatic brain injury (TBI), brain anoxia, brain tumor, or cerebral infection. As a consequence, the person may experience a variety of lifelong impairments at the behavioral, physical, cognitive, emotional, and social levels (Nestvold & Stavem, 2009), which could lead to a significant deterioration of his/her health conditions and quality of life (QoL) (Andelic et al., 2009; Dikmen, Machamer, Powell, & Temkin, 2003; Jacobsson, Westerberg, & Lexell, 2010; Nestvold & Stavem, 2009). ABI is the leading cause of death and disability in the world (Nichol et al., 2011). Aspects such as its high frequency (i.e., incidence-prevalence), the typical profile of the affected population (usually young and working-active), and the high percentage of survivors (mostly with some type of associated comorbidity) explain its high sociosanitary repercussion (Castellanos-Pinedo, Cid-Gala, Duque, Ramírez-Moreno, & Zurdo-Hernández, 2012).
In Spain, there are approximately 420,064 people with ABI, and 104,701 new cases are estimated per year (Quezada, Huete, & Bascones, 2015). Advances in medicine and medical care have increased the ABI survival rates. However, although these advances have allowed the saving of a large number of lives, many survivors live with dependency and disability that can significantly compromise their QoL. These reasons highlight and justify the need to address the QoL construct in the ABI population as a priority action to improve their life project.
Traditionally, the QoL after an ABI has been discussed and conceptualized from a health-related QoL approach (HRQoL). This model focuses on the impact that a medical condition and its treatment may have on specific domains of a person's life, mainly in physical, emotional, or social well-being areas. However, the outcomes obtained through this approach are circumscribed to a few QoL-related aspects and may offer a limited outcome-profile by disregarding or omitting other crucial areas of people’s welfare. In this sense, the HRQoL approach seems limited, insofar as it does not consider the wide variety of sequelae and needs that generally derive from this condition. Therefore, we propose a different approach for the QoL assessment from a comprehensive perspective, characterized by a broader view of personal outcomes and far from the narrow focus of medical models or others focused on restricted domains of life.
According to Schalock and Verdugo (2002, 2007), QoL is a multidimensional phenomenon that reflects the well-being desired by the person in relation to eight basic needs: emotional, material, and physical well-being, interpersonal relationships, social inclusion, rights, self-determination, and personal development. Each domain is operationalized through culturally sensitive indicators and items that reflect the personal outcomes of each domain (Gómez & Verdugo, 2016; Schalock, Verdugo, Gomez, & Reinders, 2016). Moreover, these core domains are common to all people, include subjective and objective aspects, are influenced by environmental and personal factors and their interaction, and can be enriched through quality enhancement strategies, such as individualized supports, personal growth opportunities, or inclusive environments (Schalock, Baker et al., 2018; Schalock, van Loon, & Mostert, 2018; Schalock et al., 2016;). Thus, the model incorporates a positive approach of the person, emphasizing not only the limitations, but also the strengths, as key elements in the enhancement of the systems of supports and QoL outcomes (Schalock, 2018; Thompson, Walker, Shogren, & Wehmeyer, 2018).
QoL-related personal outcomes have been considered as the key element in the rehabilitation process, aimed at limiting the consequences as much as possible and allowing the person to return to his/her preinjury life (Bullinger, 2002; Jacobsson et al., 2010; Nichol et al., 2011). In this sense, almost 20 years ago, Steadman-Pare, Colantonio, Ratcliff, Chase, and Vernich (2001) already emphasized the importance of researching this construct to develop effective intervention programs that allow enhancing the personal QoL outcomes after an ABI.
In a more recent approach, several studies have focused on analyzing the changes in QoL over time, examining the improvements from the first months/years after the injury (Forslund, Roe, Sigurdardottir, & Andelic, 2013; Scholten et al., 2015; Soberg et al., 2013; Vieira, Hora, Oliveira, Ribeiro, & Sousa, 2013) to a very long-term (Andelic et al., 2009, 2018; Jacobsson et al., 2010; Nestvold & Stavem, 2009; Steadman-Pare et al., 2001). Moreover, they analyze the association between QoL outcomes and certain variables that are expected to influence these results, identifying potentially predictive factors of a better QoL. Because of these contributions, we know that aspects such as absence of depressive symptoms (Andelic et al., 2018; Forslund et al., 2013; Soberg et al., 2013), a satisfactory community integration (Andelic et al., 2018; Forslund et al., 2013; Kalpakjian, Lam, Toussaint, & Merbitz, 2004), and the return to work (Matérne, Strandberg, & Lundqvist, 2018; Steadman-Pare et al., 2001), have a strong relationship with and a great predictive capacity for a better QoL. However, less is known about the relationships between this construct and the sociodemographic and injury-related aspects. Considering that a person’s QoL will be especially influenced by personal and environmental characteristics, it seems sensible to focus on this type of variables and analyze how these influence the person's life and recovery process (Simões & Santos, 2016). This manuscript aims to contribute to the current literature by (1) describing the QoL profile of a wide Spanish sample of adults with ABI, (2) examining the impact of sociodemographic and injury-related variables on their QoL, and (3) identifying the predictors of a better QoL.
MethodParticipantsThe sample of respondents was recruited by a non-probabilistic convenience sampling process. ABI participants had to meet the following inclusion criteria: (a) have an ABI; (b) are at least 16 years old; (c) are users of ABI-specific rehabilitation center; and (d) sign the informed consent to participate in the study. The ABI sample was composed of 421 adults from 17 rehabilitation centers providing health and social services throughout Spain. Just over half of the sample were men (60%), aged from 17 to 91 years (M = 53.12; SD = 14.87). Half of the sample were married (49.5%) and the employment situation prior to the injury shows that almost the entire sample (76.1%) was active (i.e., working and/or studying). However, it should be noted that after the injury, practically the whole sample (94.5%) was inactive. The main causes of ABI were CVA (56.3%) and TBI (21.9%), and the average time since the injury was 8.12 years (M = 6; SD = 7.3; range 1-57).
Although the ABI participants’ QoL was assessed, the respondents were 155 people, given that a report of others was used. To be an informant, they had to meet two requirements: (a) knowing the person for at least three months; and (b) being able to observe the person in different environments for substantial periods of time. Among respondents, 97 (62.6%) were health professionals and 58 (37.4%) were relatives. The relatives were mostly partners (43.1%) or parents (27.6%). Professionals were mostly neuropsychologists (24.7%), occupational therapists (22.7%), or physiotherapists (11.3%). The professionals knew the assessed person for periods between three months and 19 years (M=2.90; SD = 3.04 years).
InstrumentThe assessment of QoL was carried out through the administration of the CAVIDACE scale (Fernández, Verdugo, Gómez, Aguayo, & Arias, 2018; Verdugo, Gómez, Fernández, Aguayo, & Arias, 2018), which is a disease-specific instrument aimed to assess the QoL-related personal outcomes of adults with ABI. The scale has shown excellent evidences of validity and reliability (Fernández et al., 2019), and it has a suitable internal consistency (alpha ordinal values ranged from .81 to .93) and high inter-rater reliability (ICC = .97). The analysis of construct validity supported the eight correlated factors model (TLI = .87; CFI = .89; RMSEA = .06; SRMR = .07). The CAVIDACE scale comprises 64 items assessing different aspects of a person’s life, eight items per domain randomly distributed around the eight core domains proposed by Schalock and Verdugo (2002): Emotional well-being (EW), Interpersonal relationships (IR), Material well-being (MW), Personal development (PD), Physical well-being (PW), Self-determination (SD), Social inclusion (SI), and Rights (RI). The items are drafted as third-person statements with four frequency response options (never = 0, sometimes = 1, often = 2, always = 3). For its correction, the scale provides specific ABI yardsticks, allowing interpretation of the obtained results. Thus, direct scores obtained in each of the eight domains are converted into standard scores (M = 10; SD = 3) and percentiles. Moreover, the scale provides an overall raw QoL score (i.e., the sum of the scores obtained in each of the domains) that may vary from 0 to 192 (96 is the theoretical midpoint of the scale), where higher scores indicate higher QoL. This overall score may be converted into an easily interpretable Quality of Life Index (M = 100; SD = 15) by providing a QoL profile that allows professionals to elaborate person-centered support plans and rehabilitation programs.
ProcedureThis is a quantitative cross-sectional study. The research team contacted several organizations and health professionals that provide support and rehabilitation programs to the ABI population to obtain a broad and heterogenous sample. Interested participants were contacted by telephone and email to be informed about the study. The respondents had to score the 64 QOL-related items of the scale, estimating the frequency of the observable behaviors and circumstances that were described in them. Moreover, they completed a sociodemographic and injury-related questionnaire, based on the objective information available to each patient. Respondents had the possibility to complete the scales in a hard copy version or an online version. Then, the scales were collected, and the data were analyzed.
The Bioethics Committee of the University of Salamanca approved the research, which has complied with the ethical standards of the 1964 Declaration of Helsinki and its later amendments. Written informed consent forms were obtained from all the centers involved. These centers, in turn, have the consent forms of their patients and/or family members, which allow the use of their data for research purposes. Personal and clinical data were collected, stored, and protected, guaranteeing the confidentiality and anonymity of the participants.
Statistical analysesData were analyzed using SPSS.25 for Windows. Univariate and multivariate analyses were used to assess determinants of QoL scores. Due to the normal distribution of the dependent variable (QoL score), comparisons between groups (i.e., univariate analysis) were done using parametric tests: independent-sample t-tests were conducted to compare the total QoL score in independent variables with two levels (e.g., gender); one-way between-group analyses of variance (ANOVA) were conducted to compare the effect of the independent variables with more than two levels (e.g., civil status) in the total QoL score. In case of significant result, a Tukey post-hoc test was used to explore which means differed. A significance level of 95% was set (p ≤ .05), and effect sizes were analyzed using eta-squared (η2). The Cohen (1988) guidelines were followed to interpret the values (i.e., .01=small; .06=moderate; .14=large).
Multiple linear regression analysis was used to identify which independent variables significantly predicted QoL outcomes, and their contribution to the model. First, the sociodemographic and clinical variables that were significant in the univariate analysis were included simultaneously as an initial model (the enter method) to identify which variables were significant in the set. Factors with p ≤ .10 were retained. Once potential predictors were identified, the model was built by the backward stepwise method and then was checked by the forward method. Results are presented as R2, R2 change, F change, and standardized beta values. R2 was interpreted according to the Cohen (1988) guidelines (i.e., .02=small; .13=medium; .26=large).
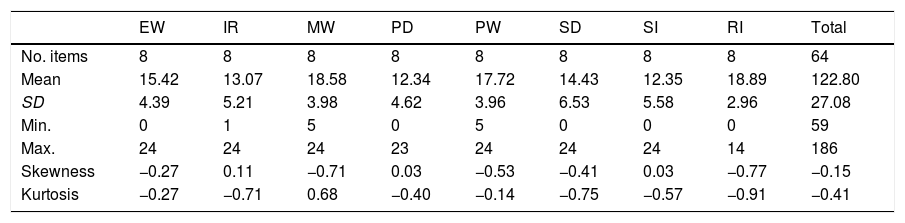
ResultsThe total QoL scores were normally distributed. The average score was 122.8 (Md = 124; SD = 27.08) and ranged from 59 to 186. The QoL scores obtained by domains were not distributed normally. These scores may range from 0 to 24 in each of the domains. In this sense, the domains with the highest values were RI (M = 18.89; SD = 2.96) and MW (M = 18.58; SD = 3.98), and the lowest values were found in PD (M = 12.34; SD = 4.62) and SI (M = 12.35; SD = 5.58) domains. These descriptive results are listed in Table 1.
Descriptive statistics of QoL scores (N = 421).
| EW | IR | MW | PD | PW | SD | SI | RI | Total | |
|---|---|---|---|---|---|---|---|---|---|
| No. items | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 64 |
| Mean | 15.42 | 13.07 | 18.58 | 12.34 | 17.72 | 14.43 | 12.35 | 18.89 | 122.80 |
| SD | 4.39 | 5.21 | 3.98 | 4.62 | 3.96 | 6.53 | 5.58 | 2.96 | 27.08 |
| Min. | 0 | 1 | 5 | 0 | 5 | 0 | 0 | 0 | 59 |
| Max. | 24 | 24 | 24 | 23 | 24 | 24 | 24 | 14 | 186 |
| Skewness | −0.27 | 0.11 | −0.71 | 0.03 | −0.53 | −0.41 | 0.03 | −0.77 | −0.15 |
| Kurtosis | −0.27 | −0.71 | 0.68 | −0.40 | −0.14 | −0.75 | −0.57 | −0.91 | −0.41 |
Note. EW = Emotional well-being; IR = Interpersonal relationships; MW = Material well-being; PD = Personal development; PW = Physical well-being; SD = Self-determination; SI = Social inclusion; RI = Rights.
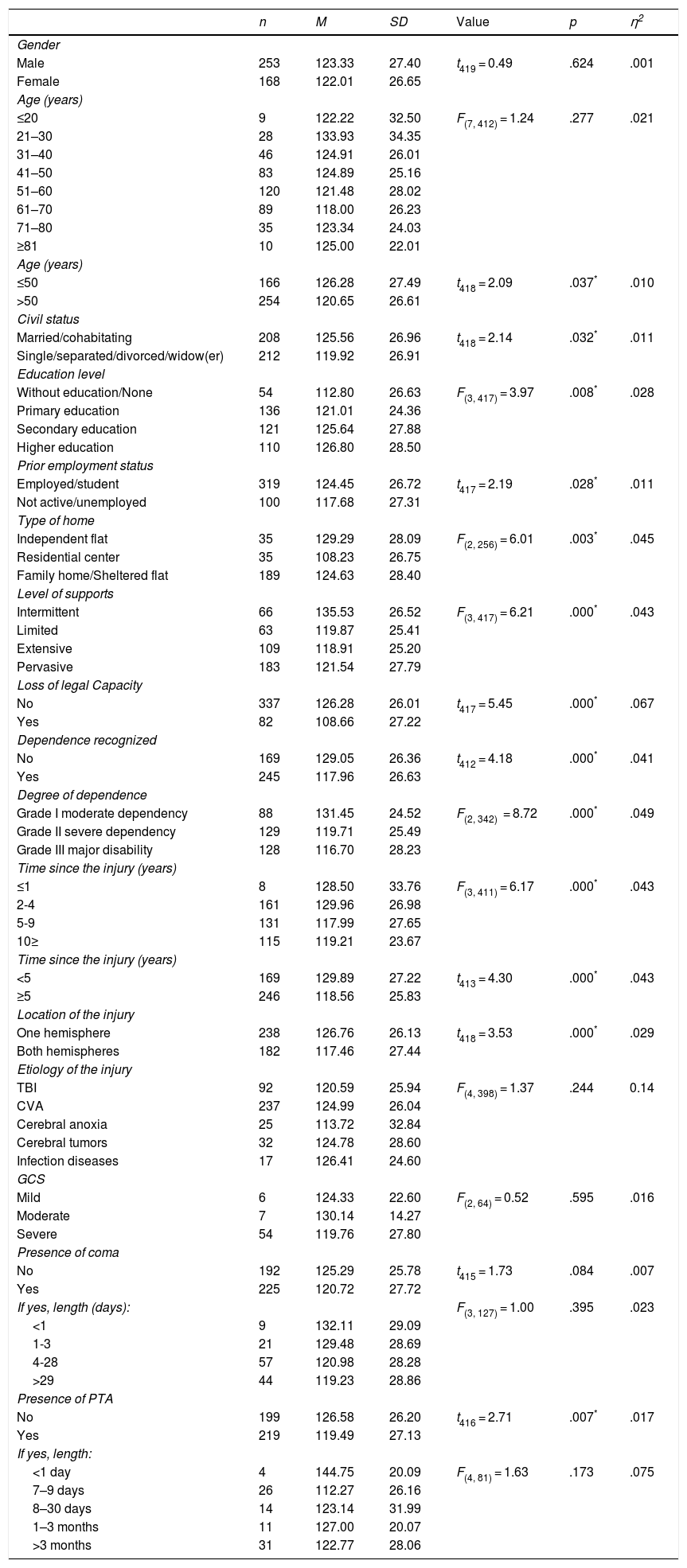
Statistically significant differences were found in total QoL score by age, civil status, education level, prior employment status, type of home, level of supports, loss of legal capacity (i.e., the loss in the ability to make legally valid decisions and establish binding contractual relationships), recognized dependence and degree of dependence (i.e., people who, due to their age or because an illness or disability situation, cannot carry out their daily basic activities without the help of another person, can apply for long-term care), time since the injury, location of the injury, and presence of post-traumatic amnesia (PTA).
A moderate effect size was found in the loss of legal capacity, degree of dependence, type of home, level of supports, time since the injury, and dependence recognized variables, in decreasing order. The remaining significant variables obtained small effect sizes, indicating a small influence on the QoL outcomes. No significant differences were detected in QoL scores (p > .05) according to gender, age (grouped variable), etiology, severity of the injury (measured with the Glasgow Coma Scale, GCS), presence of coma and its length, and length of PTA. The results of the univariate analyses are presented in Table 2.
Parametric test results for QoL total score.
| n | M | SD | Value | p | η2 | |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Male | 253 | 123.33 | 27.40 | t419 = 0.49 | .624 | .001 |
| Female | 168 | 122.01 | 26.65 | |||
| Age (years) | ||||||
| ≤20 | 9 | 122.22 | 32.50 | F(7, 412) = 1.24 | .277 | .021 |
| 21–30 | 28 | 133.93 | 34.35 | |||
| 31–40 | 46 | 124.91 | 26.01 | |||
| 41–50 | 83 | 124.89 | 25.16 | |||
| 51–60 | 120 | 121.48 | 28.02 | |||
| 61–70 | 89 | 118.00 | 26.23 | |||
| 71–80 | 35 | 123.34 | 24.03 | |||
| ≥81 | 10 | 125.00 | 22.01 | |||
| Age (years) | ||||||
| ≤50 | 166 | 126.28 | 27.49 | t418 = 2.09 | .037* | .010 |
| >50 | 254 | 120.65 | 26.61 | |||
| Civil status | ||||||
| Married/cohabitating | 208 | 125.56 | 26.96 | t418 = 2.14 | .032* | .011 |
| Single/separated/divorced/widow(er) | 212 | 119.92 | 26.91 | |||
| Education level | ||||||
| Without education/None | 54 | 112.80 | 26.63 | F(3, 417) = 3.97 | .008* | .028 |
| Primary education | 136 | 121.01 | 24.36 | |||
| Secondary education | 121 | 125.64 | 27.88 | |||
| Higher education | 110 | 126.80 | 28.50 | |||
| Prior employment status | ||||||
| Employed/student | 319 | 124.45 | 26.72 | t417 = 2.19 | .028* | .011 |
| Not active/unemployed | 100 | 117.68 | 27.31 | |||
| Type of home | ||||||
| Independent flat | 35 | 129.29 | 28.09 | F(2, 256) = 6.01 | .003* | .045 |
| Residential center | 35 | 108.23 | 26.75 | |||
| Family home/Sheltered flat | 189 | 124.63 | 28.40 | |||
| Level of supports | ||||||
| Intermittent | 66 | 135.53 | 26.52 | F(3, 417) = 6.21 | .000* | .043 |
| Limited | 63 | 119.87 | 25.41 | |||
| Extensive | 109 | 118.91 | 25.20 | |||
| Pervasive | 183 | 121.54 | 27.79 | |||
| Loss of legal Capacity | ||||||
| No | 337 | 126.28 | 26.01 | t417 = 5.45 | .000* | .067 |
| Yes | 82 | 108.66 | 27.22 | |||
| Dependence recognized | ||||||
| No | 169 | 129.05 | 26.36 | t412 = 4.18 | .000* | .041 |
| Yes | 245 | 117.96 | 26.63 | |||
| Degree of dependence | ||||||
| Grade I moderate dependency | 88 | 131.45 | 24.52 | F(2, 342) = 8.72 | .000* | .049 |
| Grade II severe dependency | 129 | 119.71 | 25.49 | |||
| Grade III major disability | 128 | 116.70 | 28.23 | |||
| Time since the injury (years) | ||||||
| ≤1 | 8 | 128.50 | 33.76 | F(3, 411) = 6.17 | .000* | .043 |
| 2-4 | 161 | 129.96 | 26.98 | |||
| 5-9 | 131 | 117.99 | 27.65 | |||
| 10≥ | 115 | 119.21 | 23.67 | |||
| Time since the injury (years) | ||||||
| <5 | 169 | 129.89 | 27.22 | t413 = 4.30 | .000* | .043 |
| ≥5 | 246 | 118.56 | 25.83 | |||
| Location of the injury | ||||||
| One hemisphere | 238 | 126.76 | 26.13 | t418 = 3.53 | .000* | .029 |
| Both hemispheres | 182 | 117.46 | 27.44 | |||
| Etiology of the injury | ||||||
| TBI | 92 | 120.59 | 25.94 | F(4, 398) = 1.37 | .244 | 0.14 |
| CVA | 237 | 124.99 | 26.04 | |||
| Cerebral anoxia | 25 | 113.72 | 32.84 | |||
| Cerebral tumors | 32 | 124.78 | 28.60 | |||
| Infection diseases | 17 | 126.41 | 24.60 | |||
| GCS | ||||||
| Mild | 6 | 124.33 | 22.60 | F(2, 64) = 0.52 | .595 | .016 |
| Moderate | 7 | 130.14 | 14.27 | |||
| Severe | 54 | 119.76 | 27.80 | |||
| Presence of coma | ||||||
| No | 192 | 125.29 | 25.78 | t415 = 1.73 | .084 | .007 |
| Yes | 225 | 120.72 | 27.72 | |||
| If yes, length (days): | F(3, 127) = 1.00 | .395 | .023 | |||
| <1 | 9 | 132.11 | 29.09 | |||
| 1-3 | 21 | 129.48 | 28.69 | |||
| 4-28 | 57 | 120.98 | 28.28 | |||
| >29 | 44 | 119.23 | 28.86 | |||
| Presence of PTA | ||||||
| No | 199 | 126.58 | 26.20 | t416 = 2.71 | .007* | .017 |
| Yes | 219 | 119.49 | 27.13 | |||
| If yes, length: | ||||||
| <1 day | 4 | 144.75 | 20.09 | F(4, 81) = 1.63 | .173 | .075 |
| 7–9 days | 26 | 112.27 | 26.16 | |||
| 8–30 days | 14 | 123.14 | 31.99 | |||
| 1–3 months | 11 | 127.00 | 20.07 | |||
| >3 months | 31 | 122.77 | 28.06 |
Note. p ≤ .05*; eta-squared = η2.
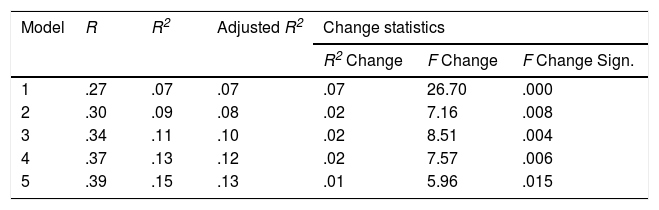
A multiple linear regression was carried out to examine the potential QoL predictors of ABI participants through the analysis of the variance in QoL scores, using first the enter method (introducing 12 factors into the model) and then the stepwise method (introducing five factors). Stepwise analysis showed five models, of which the last one was the one with the greatest predictive capacity (Table 3).
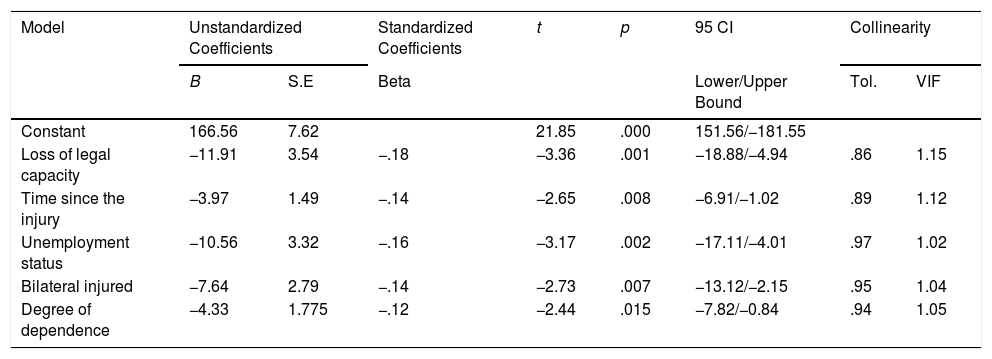
A significant model (F(5, 328) = 11.77, p<.001) predicted 15.2% of the sample outcome variance with a coefficient of determination (Adj. R2 = .13) considered medium according to the Cohen guidelines. The model fulfills homoscedasticity, and the residues are normally distributed. The resulting model contains five significant QoL predictors: loss of legal capacity (β=−11.91, t=−3.36, p=.001), time since the injury (β=−3.97, t=−2.65, p=.008), prior unemployment status (β=−10.56, t=−3.17, p=.002), location of the injury (β=−7.64, t=−2.73, p=.007), and degree of dependence (β=−4.33, t=−2.44, p=.015). The model predicted lower QoL for cases with loss of legal capacity, higher degree of dependence, prior unemployment status, longer time injured, and injured bilaterally (Table 4).
Regression analysis of variables predicting QoL: Coefficients of the factors included in the final model.
| Model | Unstandardized Coefficients | Standardized Coefficients | t | p | 95 CI | Collinearity | ||
|---|---|---|---|---|---|---|---|---|
| B | S.E | Beta | Lower/Upper Bound | Tol. | VIF | |||
| Constant | 166.56 | 7.62 | 21.85 | .000 | 151.56/−181.55 | |||
| Loss of legal capacity | −11.91 | 3.54 | −.18 | −3.36 | .001 | −18.88/−4.94 | .86 | 1.15 |
| Time since the injury | −3.97 | 1.49 | −.14 | −2.65 | .008 | −6.91/−1.02 | .89 | 1.12 |
| Unemployment status | −10.56 | 3.32 | −.16 | −3.17 | .002 | −17.11/−4.01 | .97 | 1.02 |
| Bilateral injured | −7.64 | 2.79 | −.14 | −2.73 | .007 | −13.12/−2.15 | .95 | 1.04 |
| Degree of dependence | −4.33 | 1.775 | −.12 | −2.44 | .015 | −7.82/−0.84 | .94 | 1.05 |
Note. B=Unstandardized beta; S.E=Standard error; Tol=Tolerance; VIF=Variance inflation factor; CI=Confidence Interval.
The study presents the QoL-related personal outcomes in a wide sample of adult population with ABI in Spain, as measured by the CAVIDACE scale. Likewise, it also explores the association between QoL and a set of sociodemographic and injury-related factors that were expected to influence the person’s QoL and identify the potential predictors that may best predict the QoL. In this sense, the study contributes to the current knowledge and understanding of the QoL construct in ABI population.
The results by domains showed that RI and MW were the ones with the highest values, whereas PD and SI obtained the lowest scores. These results are consistent with those obtained in other studies assessing recipients of social services (Gómez, Verdugo, Arias, Navas, & Schalock, 2013), children and adolescents with rare diseases and intellectual disability (González, Gómez, & Alcedo, 2016), or breast cancer patients (Finck, Barradas, Zenger, & Hinz, 2018). The highest outcomes could be explained by the attention and support received in the sociosanitary organizations they attend, which strive to achieve adequate emotional, material, and physical support, as well as the defense of their rights (Simões & Santos, 2016). On the other hand, the lowest scores could be a reflection of the typical limitations that people with ABI usually experience in social relationships and community participation, personal autonomy, activities of daily living, and problem solving. These facts highlight the especially vulnerable character of the mentioned areas after an ABI, identifying them as priorities when developing strategies to improve results.
Sociodemographic variables were expected to influence QoL by reflecting populations with particular life problems. Thus, statistically significant differences were found in several of them. First, younger people showed a better QoL compared with the elders. This finding is widely supported by previous ABI research, which reports that QoL decreases as age increases, possibly due to the slow recovery of the elderly (Forslund et al., 2013; Scholten et al., 2015). Second, those with a partner or in a relationship showed a better QoL, reflecting the importance attributed to having a close relationship in the satisfaction of the person (Steadman-Pare et al., 2001; Vieira et al., 2013), although there are also studies that do not find any association (Forslund et al., 2013; Jacobsson et al., 2010; Kalpakjian et al., 2004; Matérne et al., 2018; Sharma, Jain, Sharma, Mittal, & Gupta, 2015). Third, a better QoL was found in those who had completed secondary or higher education compared with those who had no studies, possibly due to the greater opportunities that the education level can generate in access to employment and economic resources (Forslund et al., 2013; Matérne et al., 2018), although this was inconsistent with results by Kalpakjian et al. (2004); Sharma et al. (2015), and Vieira et al. (2013). Fourth, in line with previous research (Andelic et al., 2009, 2018; Forslund et al., 2013; Jacobsson et al., 2010; Soberg et al., 2013), those who were employed/studying (i.e., active) at the time of the injury showed significantly higher QoL scores, reflecting the importance of a productive lifestyle to QoL (Jacobsson et al., 2010; Soberg et al., 2013). Fifth, living more independently is significantly related to a better QoL (Alcedo, Fontanil, Solís, Pedrosa, & Aguado, 2017; Claes, van Hove, Vandevelde, van Loon, & Schalock, 2012), contrary to Matérne et al. (2018) and Kalpakjian et al. (2004), who did not find differences regarding living arrangements. Sixth, as expected, the greater the level of support needs, the lower the QoL (González et al., 2016). Seventh, people with deprived legal capacity showed a lower QoL, probably due to the importance of being able to make preference-based elections/decisions/choices (Verdugo et al., 2015). Finally, needing support or supervision to carry out the activities of daily living (i.e., recognized dependence) was significantly related to a worse QoL. In this way, the greater the degree of dependence, the greater are the deficits or limitations to cope with these activities and, therefore, the worse is the QoL.
According to the clinical variables, those who were recently injured reported a better QoL (Andelic et al., 2018; Man, Yip, Ko, Kwok, & Tsang, 2010). This could be due to the fact that the alterations produced by the injury could worsen with the passage of time and are added to those specific to the aging process. Other studies indicated that the passage of time could decrease the impact of the injury, contributing to the stability of the sequelae (Jacobsson et al., 2010; Nestvold & Stavem, 2009; Sharma et al., 2015). In addition, a better QoL was reported in those whose injury occurred unilaterally, probably due to the fact that bilateral injuries could imply greater severity and a greater number of sequelae compromising the correct functioning of the individual. Finally, PTA influenced QoL scores. This is a very controversial variable, regardless of how it is measured, and the literature is inconsistent (Kalpakjian et al., 2004; Soberg et al., 2013; Steadman-Pare et al., 2001).
Other variables included were not associated with total QoL scores in our sample. Nonetheless, there is clear agreement in the fact that being a woman results in a worse QoL (Dijkers, 2004; Theadom et al., 2016). In fact, Farace and Alves (2000) corroborated in a meta-analysis study that women fare worse than men across several aspects, alluding to aspects such as the cause of the injury, premorbid factors, treatment variables, or differences in cognition or psychosocial aspects, as the possible causes of a worse performance. This implies that females are at risk of poorer outcomes than males in several aspects, the QoL among them. The etiology of the ABI did not have a significant impact on the QoL (Matérne et al., 2018), possibly because, regardless of the cause the injury, the consequences will have a serious impact on the person's life.
Finally, although many of the variables impacted the QoL outcomes, only five were QoL predictors in ABI. In this sense, having deprived legal capacity, having a greater degree of dependence, being unemployed or inactive before the injury, being injured recently, and being injured bilaterally were significant predictors of a worse QoL. These aspects should be considered when providing support and services aimed to improve the lives of people with ABI. Nevertheless, it should be noted, according to the scientific literature, that adding possible variables in the regression model (e.g., the return to work, the presence of depressive symptoms or the community integration; Andelic et al., 2018; Matérne et al., 2018), could considerably increase the value of the explained variance in QoL so this should be considered in future studies.
This study has limitations. First, its cross-sectional design showed only relationships between predictors and QoL scores, not causal connections. Second, a convenience sampling allowed us to obtain participants using the most readily available members of the study population. Nevertheless, this method does not allow to make inferences about the larger population. However, the heterogeneity of the sample must be also highlighted. While most of the studies focus mainly on the two most common types of ABI (CVA and TBI), our sample is composed of all the etiologies that make up this condition, providing a broader view of the condition. Third, an evaluation carried out by informants (in this case, professionals and family members) may over-or underreport patients' problems, thereby reducing ecological validity of the instruments (Winter, Moriarty, Robinson, & Newhart, 2016). This property should be addressed in future research, analyzing the discrepancy in the results depending on the person who administers it.
Future research should consider the use of a measure that captures the personal-related QoL outcomes through a self-report, giving voice to the person with ABI as the main character of his/her life. Moreover, the use of additional measures that capture aspects particularly relevant and influential in the QoL, and the longitudinal studies that evaluate these outcomes at different times, could provide more evidence in the study of the QoL predictors in ABI. A more detailed analysis of the association and impact of these variables with the results of QoL by domains will yield more specific information.