In the assessment of the second specialty training programs, the opinion of residents and graduates is essential to know the degree of satisfaction with the training received. The aimed was to assess the perceptions of Peruvian nephrology residents and graduates regarding their training.
MaterialA descriptive, cross-sectional study included all final-year residents and graduates of the nephrology program in 2022. An anonymous virtual survey assessed sociodemographic aspects, nephrology tutoring, clinical training, external rotations, research, the impact of the COVID-19 pandemic, and overall perception of their training.
ResultsWith a response rate of 79.68%, 51 participants were evaluated. 76.48% of the participants rated their overall training during the residency as good. 58% agreed or strongly agreed that their tutor's performance was good. 66.6% agreed or strongly agreed that their theoretical training was good, with less certainty in genetic kidney diseases. 90% agreed or strongly agreed that their practical training was good, with less certainty in training in slow therapies, renal biopsies, acute peritoneal dialysis, and peritoneal dialysis catheter placement. 80.4% agreed or strongly agreed that the pandemic affected their training. The general perception had a positive correlation with the tutor's performance as good (r=0.50; P<.001), the good perception of the hospital's research level (r=0.47, P<.001), and the perception of good opportunities to get a job as a nephrologist (r=0.67, P<.001).
ConclusionAlthough, in general, the perception is positive, there are aspects in which the training of Peruvian nephrology residents should be improved.
En la valoración de los programas formativos de segunda especialidad, la opinión de los residentes y egresados es fundamental para conocer el grado de satisfacción con la formación recibida. El objetivo fue evaluar las percepciones de los residentes y egresados de nefrología peruanos sobre su formación.
MétodosEstudio descriptivo transversal que incluyó a todos los residentes de último año y egresados de la carrera de nefrología en el año 2022. Mediante encuesta virtual anónima se evaluaron aspectos sociodemográficos, tutorías de nefrología, formación clínica, rotaciones externas, investigación, impacto del COVID-19 pandemia, y la percepción general de su formación.
ResultadosCon una tasa de respuesta del 79,68%, se evaluaron 51 participantes. El 76,48% de los participantes calificaron como buena su formación global durante la residencia. El 58% estuvo de acuerdo o muy de acuerdo en que el desempeño de su tutor fue bueno. El 66,6% estuvo de acuerdo o muy de acuerdo en que su formación teórica fue buena, con menor certeza en enfermedades renales genéticas. El 90% estuvo de acuerdo o muy de acuerdo en que su formación práctica fue buena, con menor certeza en la formación en terapias lentas, biopsias renales, diálisis peritoneal aguda y colocación de catéter de diálisis peritoneal. El 80,4% estuvo de acuerdo o muy de acuerdo en que la pandemia afectó su formación.
ConclusiónSi bien, en general, la percepción es positiva, existen aspectos en los que se debe mejorar la formación de los residentes de nefrología peruanos.
Chronic kidney disease (CKD) is a growing public health problem in all countries, including small- and middle-income countries such as Peru.1,2 The prevalence of CKD in our country doubled from 2010 to 2017, and the number of hemodialysis clinics increased; however, the number of nephrologists decreased from 4.36 to 1.91 per 1000 patients with CKD in the same period.3 This trend is similar to that reported in North American and European countries, where the number of nephrologists per patient also decreased.4 In this context, second specialty programs are essential for training new nephrology specialists to meet the growing demand, and the quality of their training must be a priority.3
In Peru, the medical specialization in Nephrology is regulated by the "Reglamento del Consejo Nacional del Residentado Médico del Perú" (Regulations of the National Council of Medical Residency of Peru), which establishes its length and basic competencies.5 Currently, 8 universities offer the Nephrology specialization program, with approximately 15 hospital sites nationwide, most of them in Lima, the capital of the country, with 40 vacancies in the 2022 admission process.6 Due to the need for more specialist physicians in our country, the number of residency positions in all medical specialties nationwide, including Nephrology, has increased; however, it has been suggested that this increase does not go hand-in-hand with improvements in the conditions that ensure their quality,7 so the evaluation of their training is a necessity.
In the assessment of the second specialty training programs, the opinion of residents and graduates is essential to know the degree of satisfaction with the training received, which includes their perception as to whether the knowledge and skills obtained during residency are sufficient to be able to practice as specialists.8–10 In this regard, different studies in Europe, North America, and Latin America have explored the perceptions of nephrology residents regarding their training.8–10 These research studies show that, while most residents in different regions identify strengths in their programs,8,9 others identified weaknesses such as lack of support from the assigned tutor, insufficient training in peritoneal dialysis, and lack of opportunities for performing renal biopsies, among others.8,9,11,12
In Peru, a study among residents and graduates in 2012 showed that, although about 60% of respondents considered their training to be good, they highlighted aspects such as poor support from tutors, deficient scientific activity during residency, and the lack of clinical spaces to complete their training.10 From 2015 to 2022, the number of vacancies in medical residency programs in our country increased by almost 50%,13 an increase that was probably not accompanied by improved conditions to ensure quality.7 This may mean that the general perception of their training and some specific aspects have worsened. For example, in 2015, the regulation of medical residency in our country changed, and the requirement to complete a research project to graduate was withdrawn, so the perception of aspects related to research has likely been affected.5 Likewise, the COVID-19 pandemic compromised the training of residents in Peru and the world, which affected the quality of their training in some aspects.14,15 However, specifically among nephrology residents, some studies suggest that the impact was not significant.16 However, the pandemic in our country revealed the structural deficiencies of our health system that impacted medical education,14 so it is possible that, in the case of Peru, the pandemic may have affected the perception of its quality. Therefore, it is necessary to evaluate the residents' perception of their academic training in Nephrology to identify aspects that can be improved to establish strategies to guarantee the continuous improvement of the programs. Therefore, the objective of this study was to evaluate the perceptions of Peruvian nephrology residents and graduates regarding their training.
Material and methodsStudy design, context, population, and sampleThis cross-sectional, descriptive study included all final-year residents and graduates of the nephrology program in 2022 in Peru. Residents and graduates who did not sign the informed consent form and the final-year resident directly related to the development of this study were excluded. Sampling was done by the snowball method.
In Peru, each of the universities has its own syllabus, even if it did not establish workload homogeneity and mandatory rotations, the biggest difference is the number of years in training. The Universidad Peruana Cayetano Heredia offers a 4-year program, and the other universities offer a 3-year program.
VariablesTo assess the perception of Nephrology residency training in Peru, a virtual survey was used as an instrument, adapted from a similar one used in a research study published in 2015 that mainly included the Likert scale used in previous evaluations in our country.10,17,18
To assess the instrument's coherence, relevance, and clarity, it was submitted to the judgment of experts following the Delphi methodology. The panel of experts was formed by the Chiefs of the Nephrology Service of the Dos de Mayo National Hospital and the Cayetano Heredia National Hospital, the coordinator of Nephrology residents of the National University of San Marcos (Universidad Nacional Mayor de San Marcos) at the Edgardo Rebagliati Martins National Hospital, and the coordinator of Nephrology residents of the Cayetano Heredia National Hospital at the Arzobispo Loayza National Hospital. Subsequently, a pilot study was conducted on a sample of five nephrology residents and graduates to ensure an understanding of the questions.
The survey included the following aspects: sociodemographic data, Nephrology tutoring, clinical training, external rotations, research, the impact of the COVID-19 pandemic, and overall perception of their training. The survey was anonymous, included informed consent, and the average time to fill out the survey was 15 min.
ProceduresThe Peruvian Society of Nephrology (SPN) provided the list of residents and graduates. The SPN has an updated census of the country's residents and nephrologists for planning regular training activities. This census includes e-mail and cell phone numbers.
The study details and the link to the virtual survey were disseminated through the SPN's official communications media, inviting residents and graduates to fill out the survey. Additionally, the survey was sent via email and WhatsApp messages to residents and graduates once a week, and, in case of non-response, the message was repeated weekly for 3 weeks. The data collection period was from March 24 to April 15, 2023.
With the data from the questionnaire, a database was created using the Microsoft Excel program, which did not include names, last names, identity documents, or other personal data since a code was assigned to each participant.
Statistical analysisThe Stata v. 17 program was used for database analysis. For categorical variables, relative and absolute frequencies were calculated. The mean and standard deviation were estimated for analyzing continuous variables. The results are presented in tables and graphs. The correlations between variables were carried out using the Spearman coefficient (ρ). Statistical significance was set at a P-value <.05.
Ethical aspectsThe Institutional Research Ethics Committee of the Universidad Católica Santa María, Arequipa, approved the study protocol on March 9, 2023, through favorable pronouncement N° 024-2023.
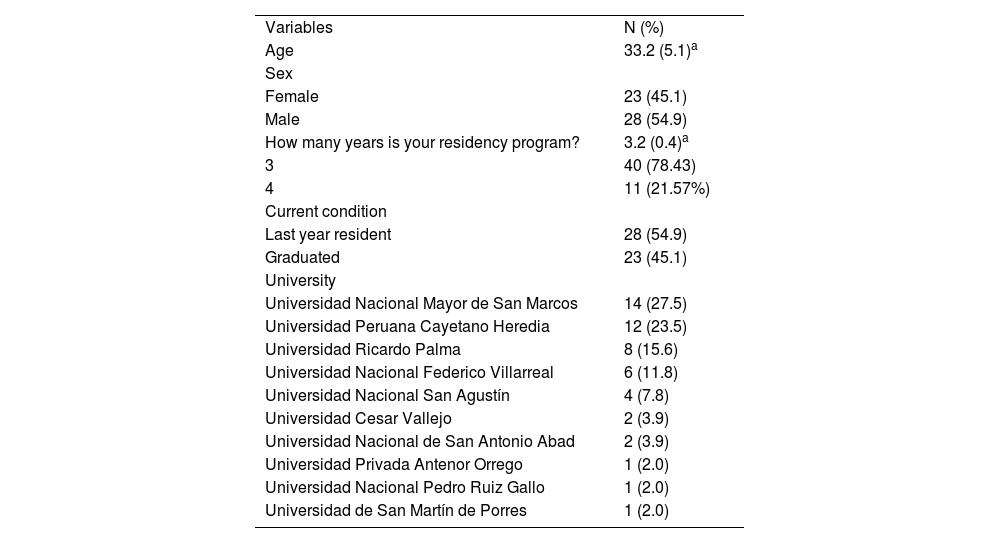
ResultsIn total, the population of final-year residents and graduates of Nephrology in 2022 was 64, and 51 participants responded to the survey, representing a response rate of 79.68%. The mean age was 33.2 years; most were male (54.9%), final-year residents (54.9%), from the National University of San Marcos (27.5%), and belonged to a 3-year training program (78.43%) (Table 1).
Sociodemographic characteristics of nephrology residents and graduates.
| Variables | N (%) |
| Age | 33.2 (5.1)a |
| Sex | |
| Female | 23 (45.1) |
| Male | 28 (54.9) |
| How many years is your residency program? | 3.2 (0.4)a |
| 3 | 40 (78.43) |
| 4 | 11 (21.57%) |
| Current condition | |
| Last year resident | 28 (54.9) |
| Graduated | 23 (45.1) |
| University | |
| Universidad Nacional Mayor de San Marcos | 14 (27.5) |
| Universidad Peruana Cayetano Heredia | 12 (23.5) |
| Universidad Ricardo Palma | 8 (15.6) |
| Universidad Nacional Federico Villarreal | 6 (11.8) |
| Universidad Nacional San Agustín | 4 (7.8) |
| Universidad Cesar Vallejo | 2 (3.9) |
| Universidad Nacional de San Antonio Abad | 2 (3.9) |
| Universidad Privada Antenor Orrego | 1 (2.0) |
| Universidad Nacional Pedro Ruiz Gallo | 1 (2.0) |
| Universidad de San Martín de Porres | 1 (2.0) |
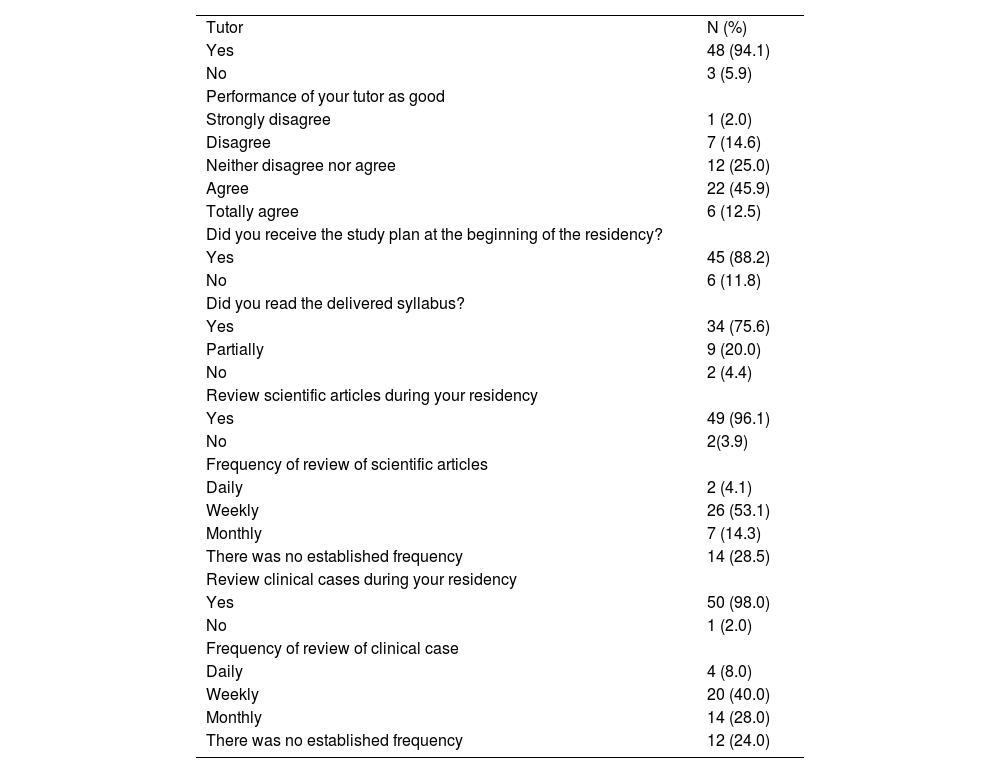
94.1% of respondents noted that they had a Nephrology tutor during residency, and 58% agreed or strongly agreed that their performance was good (Table 2).
Nephrology tutoring and clinical training.
| Tutor | N (%) |
| Yes | 48 (94.1) |
| No | 3 (5.9) |
| Performance of your tutor as good | |
| Strongly disagree | 1 (2.0) |
| Disagree | 7 (14.6) |
| Neither disagree nor agree | 12 (25.0) |
| Agree | 22 (45.9) |
| Totally agree | 6 (12.5) |
| Did you receive the study plan at the beginning of the residency? | |
| Yes | 45 (88.2) |
| No | 6 (11.8) |
| Did you read the delivered syllabus? | |
| Yes | 34 (75.6) |
| Partially | 9 (20.0) |
| No | 2 (4.4) |
| Review scientific articles during your residency | |
| Yes | 49 (96.1) |
| No | 2(3.9) |
| Frequency of review of scientific articles | |
| Daily | 2 (4.1) |
| Weekly | 26 (53.1) |
| Monthly | 7 (14.3) |
| There was no established frequency | 14 (28.5) |
| Review clinical cases during your residency | |
| Yes | 50 (98.0) |
| No | 1 (2.0) |
| Frequency of review of clinical case | |
| Daily | 4 (8.0) |
| Weekly | 20 (40.0) |
| Monthly | 14 (28.0) |
| There was no established frequency | 12 (24.0) |
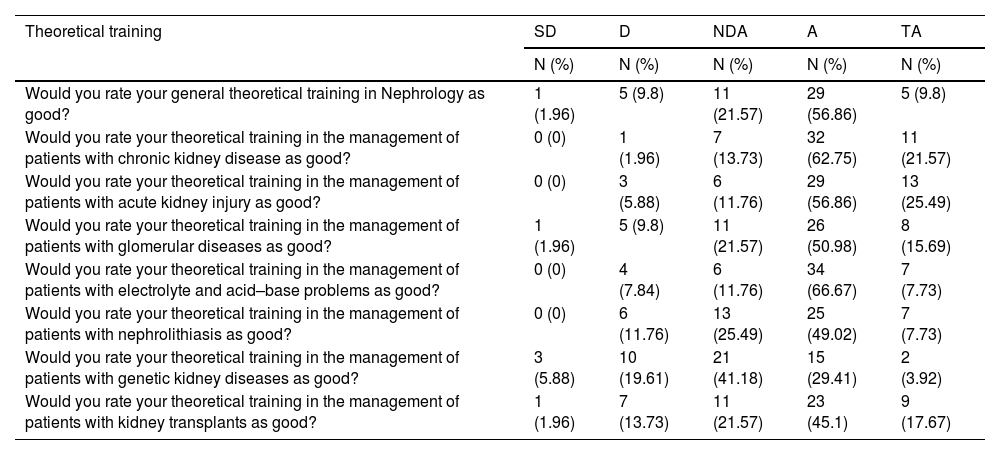
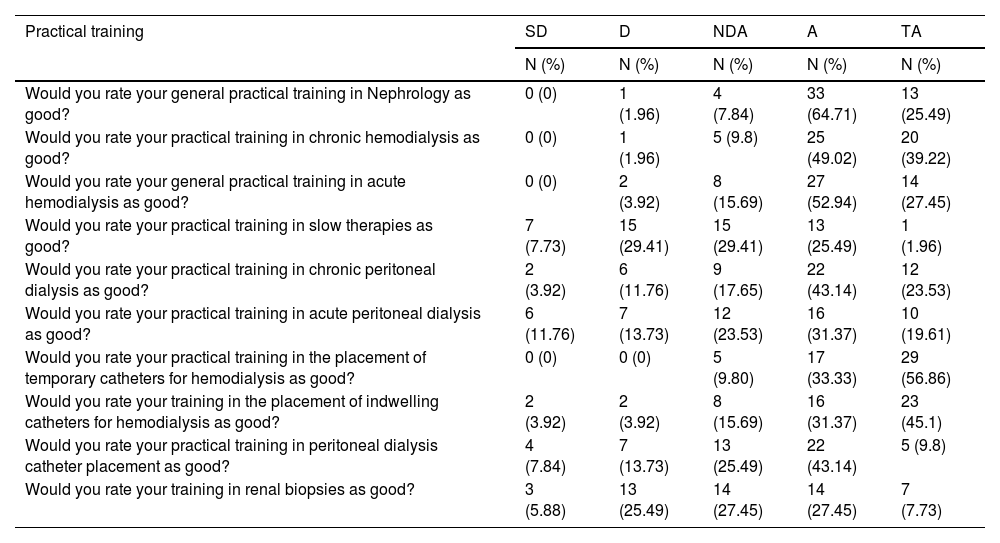
88.2% of the respondents indicated they received a syllabus at the beginning of their residency, and 95% read it partially or completely. 96.1% reviewed scientific articles mostly every week (53.1%). Similarly, 98% reviewed clinical cases, mostly every week (40%). Regarding their theoretical training, 66.6% agreed or strongly agreed that it was good, with less certainty in the case of genetic kidney diseases, whereas 25.49% disagreed or strongly disagreed (Table 3). In the case of practical training, 90% agreed or strongly agreed that it was good, with less certainty in the case of training in slow therapies, renal biopsies, acute peritoneal dialysis, and peritoneal dialysis catheter placement, where 43.14%, 31.37%, 25.49%, and 21.57% disagreed or strongly disagreed, respectively (Table 4).
Theoretical training.
| Theoretical training | SD | D | NDA | A | TA |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | |
| Would you rate your general theoretical training in Nephrology as good? | 1 (1.96) | 5 (9.8) | 11 (21.57) | 29 (56.86) | 5 (9.8) |
| Would you rate your theoretical training in the management of patients with chronic kidney disease as good? | 0 (0) | 1 (1.96) | 7 (13.73) | 32 (62.75) | 11 (21.57) |
| Would you rate your theoretical training in the management of patients with acute kidney injury as good? | 0 (0) | 3 (5.88) | 6 (11.76) | 29 (56.86) | 13 (25.49) |
| Would you rate your theoretical training in the management of patients with glomerular diseases as good? | 1 (1.96) | 5 (9.8) | 11 (21.57) | 26 (50.98) | 8 (15.69) |
| Would you rate your theoretical training in the management of patients with electrolyte and acid–base problems as good? | 0 (0) | 4 (7.84) | 6 (11.76) | 34 (66.67) | 7 (7.73) |
| Would you rate your theoretical training in the management of patients with nephrolithiasis as good? | 0 (0) | 6 (11.76) | 13 (25.49) | 25 (49.02) | 7 (7.73) |
| Would you rate your theoretical training in the management of patients with genetic kidney diseases as good? | 3 (5.88) | 10 (19.61) | 21 (41.18) | 15 (29.41) | 2 (3.92) |
| Would you rate your theoretical training in the management of patients with kidney transplants as good? | 1 (1.96) | 7 (13.73) | 11 (21.57) | 23 (45.1) | 9 (17.67) |
SD: Strongly disagree D: disagree NDA: Neither disagree nor agree A: Agree TA Totally agree.
Practical training.
| Practical training | SD | D | NDA | A | TA |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | |
| Would you rate your general practical training in Nephrology as good? | 0 (0) | 1 (1.96) | 4 (7.84) | 33 (64.71) | 13 (25.49) |
| Would you rate your practical training in chronic hemodialysis as good? | 0 (0) | 1 (1.96) | 5 (9.8) | 25 (49.02) | 20 (39.22) |
| Would you rate your general practical training in acute hemodialysis as good? | 0 (0) | 2 (3.92) | 8 (15.69) | 27 (52.94) | 14 (27.45) |
| Would you rate your practical training in slow therapies as good? | 7 (7.73) | 15 (29.41) | 15 (29.41) | 13 (25.49) | 1 (1.96) |
| Would you rate your practical training in chronic peritoneal dialysis as good? | 2 (3.92) | 6 (11.76) | 9 (17.65) | 22 (43.14) | 12 (23.53) |
| Would you rate your practical training in acute peritoneal dialysis as good? | 6 (11.76) | 7 (13.73) | 12 (23.53) | 16 (31.37) | 10 (19.61) |
| Would you rate your practical training in the placement of temporary catheters for hemodialysis as good? | 0 (0) | 0 (0) | 5 (9.80) | 17 (33.33) | 29 (56.86) |
| Would you rate your training in the placement of indwelling catheters for hemodialysis as good? | 2 (3.92) | 2 (3.92) | 8 (15.69) | 16 (31.37) | 23 (45.1) |
| Would you rate your practical training in peritoneal dialysis catheter placement as good? | 4 (7.84) | 7 (13.73) | 13 (25.49) | 22 (43.14) | 5 (9.8) |
| Would you rate your training in renal biopsies as good? | 3 (5.88) | 13 (25.49) | 14 (27.45) | 14 (27.45) | 7 (7.73) |
SD: Strongly disagree D: disagree NDA: Neither disagree nor agree A: Agree TA Totally agree.
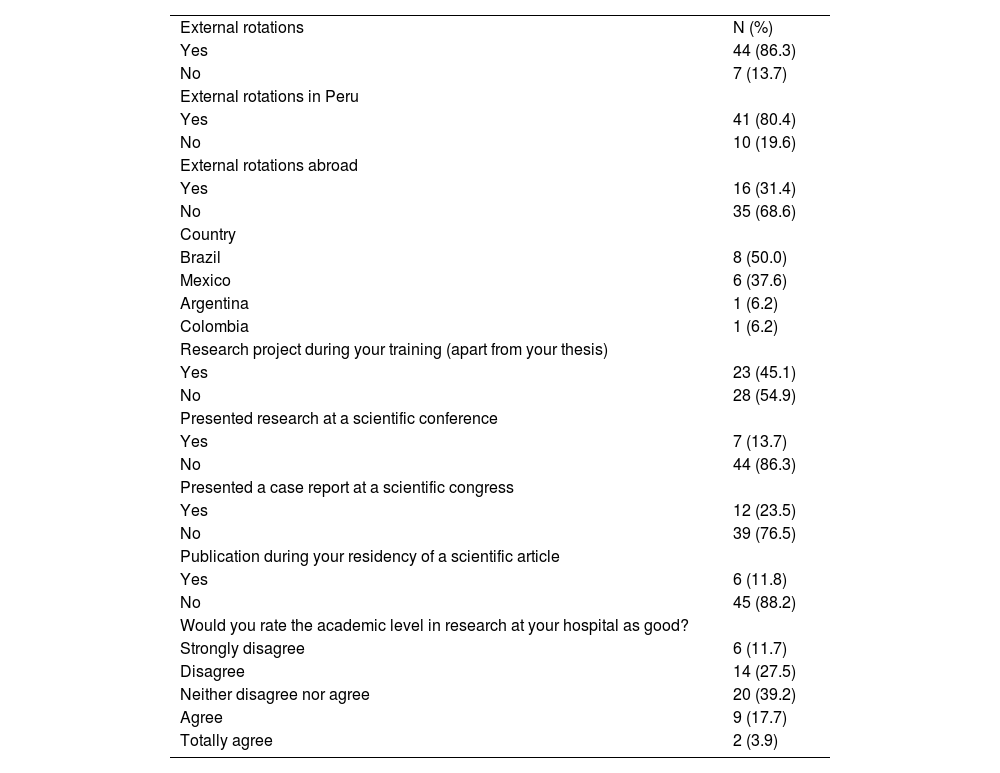
86.3% had external rotations, 80.4% in Peru, and only 31.4% abroad, mainly in Brazil (50%) (Table 5).
External rotations and research.
| External rotations | N (%) |
| Yes | 44 (86.3) |
| No | 7 (13.7) |
| External rotations in Peru | |
| Yes | 41 (80.4) |
| No | 10 (19.6) |
| External rotations abroad | |
| Yes | 16 (31.4) |
| No | 35 (68.6) |
| Country | |
| Brazil | 8 (50.0) |
| Mexico | 6 (37.6) |
| Argentina | 1 (6.2) |
| Colombia | 1 (6.2) |
| Research project during your training (apart from your thesis) | |
| Yes | 23 (45.1) |
| No | 28 (54.9) |
| Presented research at a scientific conference | |
| Yes | 7 (13.7) |
| No | 44 (86.3) |
| Presented a case report at a scientific congress | |
| Yes | 12 (23.5) |
| No | 39 (76.5) |
| Publication during your residency of a scientific article | |
| Yes | 6 (11.8) |
| No | 45 (88.2) |
| Would you rate the academic level in research at your hospital as good? | |
| Strongly disagree | 6 (11.7) |
| Disagree | 14 (27.5) |
| Neither disagree nor agree | 20 (39.2) |
| Agree | 9 (17.7) |
| Totally agree | 2 (3.9) |
45.1% carried out a research project during their residency in addition to their thesis project, 13.7% presented research at a specialty congress, 23.5% a case report, and 11.8% published a scientific article. 21.6% agreed or strongly agreed that the academic level of research in their hospital was good (Table 5).
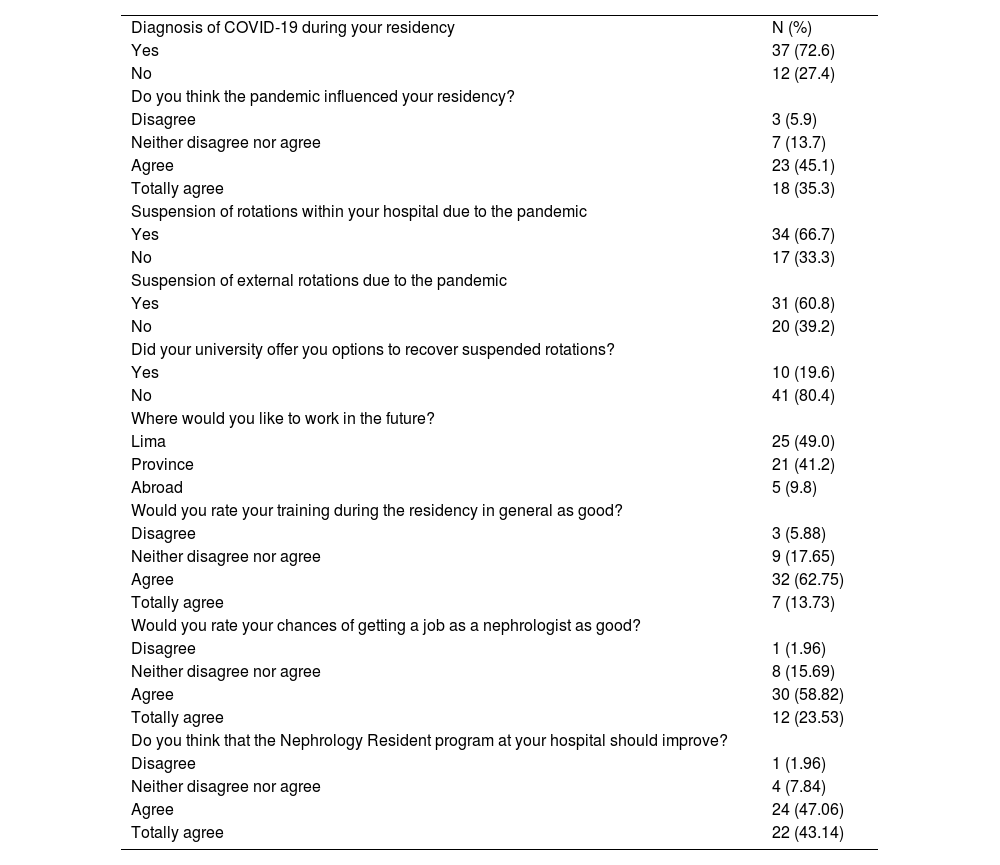
Impact of the pandemic72.6% were diagnosed with COVID-19 during their residency. 80.4% agreed or strongly agreed that the pandemic affected their training. 66.7% failed rotations within their hospital due to the pandemic, and 60.8% failed external rotations. 80.4% stated that their university did not offer them options to make up for suspended rotations (Table 6).
Pandemic impact, external rotations, and general perception.
| Diagnosis of COVID-19 during your residency | N (%) |
| Yes | 37 (72.6) |
| No | 12 (27.4) |
| Do you think the pandemic influenced your residency? | |
| Disagree | 3 (5.9) |
| Neither disagree nor agree | 7 (13.7) |
| Agree | 23 (45.1) |
| Totally agree | 18 (35.3) |
| Suspension of rotations within your hospital due to the pandemic | |
| Yes | 34 (66.7) |
| No | 17 (33.3) |
| Suspension of external rotations due to the pandemic | |
| Yes | 31 (60.8) |
| No | 20 (39.2) |
| Did your university offer you options to recover suspended rotations? | |
| Yes | 10 (19.6) |
| No | 41 (80.4) |
| Where would you like to work in the future? | |
| Lima | 25 (49.0) |
| Province | 21 (41.2) |
| Abroad | 5 (9.8) |
| Would you rate your training during the residency in general as good? | |
| Disagree | 3 (5.88) |
| Neither disagree nor agree | 9 (17.65) |
| Agree | 32 (62.75) |
| Totally agree | 7 (13.73) |
| Would you rate your chances of getting a job as a nephrologist as good? | |
| Disagree | 1 (1.96) |
| Neither disagree nor agree | 8 (15.69) |
| Agree | 30 (58.82) |
| Totally agree | 12 (23.53) |
| Do you think that the Nephrology Resident program at your hospital should improve? | |
| Disagree | 1 (1.96) |
| Neither disagree nor agree | 4 (7.84) |
| Agree | 24 (47.06) |
| Totally agree | 22 (43.14) |
49% want to work in Lima at the end of their residency, and 54.9% think the Nephrology residency should last 4 years. 76.48% of the participants rated their training during residency as generally good, and 82.35% rated their chances of getting a job as a nephrologist as good. However, 83.01% believe that the Nephrology residency program at their hospital should be improved (Table 6).
Correlation analysis between the perception of training in general and variables related to trainingWhen correlating the general perception of the training during the residency, a positive correlation is evidenced with the tutor's performance as good (r=0.50; P<.001), the good perception of the hospital's research level (r=0.47, P<.001) and the perception of good opportunities to get a job as a nephrologist (r=0.67, P<.001). There is no evidence of a correlation between the influence of the pandemic on residency (r=0.08), P=.591) and the need to improve the residency program (r=−0.18, P=.239).
DiscussionOur main results show that, although, in general, almost 7 out of 10 participants rated their training as good, 8 out of 10 considered that the residency at their hospital should be improved. Likewise, although their theoretical training was considered good, some practical aspects were considered deficient, including research activity in their hospital. More than 7 out of 10 residents had COVID-19, and 8 out of 10 felt the pandemic affected their training.
There were 49 residents and graduates in 2012 (10), meaning there was a 30% increase for 2023. This increase is due to the need for more nephrologists to attend to the rise in patients with kidney diseases and dialysis in our country, as occurs worldwide.3,4 However, this increase in vacancies did not initially mean an improvement in teaching conditions in second specialization programs. A study in 2 national referral hospitals in 2015 that evaluated the perception of residents of several medical specialties regarding teaching conditions after the increase in vacancies showed that the number of tutors, the activity of these, and the infrastructure for residents were perceived as unchanged.7 These aspects had already been described as poor, with the usual number of vacancies in a previous study.19 Although our study does not explicitly assess whether teaching conditions improved, we can indirectly assess it by verifying the variation of some perceptions concerning the 2012 assessment.
The presence of tutors increased from 88.1% to 94.1%, as well as academic activities increased since, in 2012, 40% referred that scientific articles were reviewed, and only 15% performed clinical case reviews.10 Our results also suggest that satisfaction regarding their theoretical training improved, as only 11.76% disagreed or strongly disagreed that it was good, whereas, in 2012, 32.5% considered it deficient or very deficient.10 However, regarding their practical training, some aspects did not improve significantly; for example, in 2012, 45% considered that their training in renal biopsy was adequate, and now, 41.18% agree or strongly agree that their training in this aspect was good.10 This is relevant because, at least at the hospital level, which is where our residents are trained, renal biopsies are mostly performed by nephrologists, so this decrease may be related to the increase of residents and lower probability of training in this procedure.7 On the contrary, some aspects did show improvement, such as training in peritoneal dialysis catheter placement, since 52.94% currently agree or strongly agree that their training in this aspect is good, in contrast to the 22.5% reported in 2012.10 A decrease in international rotations was observed since 65% mentioned that they did or would do it in 2012, while, in our study, only 31.4% did it.10 In the research item, there were also improvements since, in 2012, 67.5% of respondents said they never did research during residency.10 The overall perception of training during residency and job prospects did not change significantly; it remained positive since, in 2012, 80% considered their training as good or very good, and 70% considered their job prospects were also good or very good.10
The improvements observed may mean that, despite the limitations, the universities offering residency programs have improved their students' training. However, it is also possible that rather than the universities, changes in the internal organization of the hospitals cause this progress. Indeed, in our country, although physicians apply for residency programs offered by universities, the implementation of these programs depends on the hospitals in which they will be trained. In other words, several residents from the same university may perceive that their training is different since they are in various hospitals. These improvements may be independent of the official program of the universities when, for example, the Nephrology service of each hospital organizes the academic activities, or a physician designated by the same service oversees directing these activities for all residents regardless of their university or the length of their programs (only the Cayetano Heredia University offers a 4-year residency program in Nephrology). This probably explains our findings of the improvement in the perception regarding the theoretical training of the residents. In that sense, our results may reflect not only the perception of their training by the university but also their training by the hospital where they are located. However, despite these positive aspects, based on the high percentage of respondents who are not completely satisfied with the work of their designated tutor, there are still areas to work on.
Despite the improvements that the internal organization of hospitals may undergo, the structural problems of the country's hospitals are well known. For example, in the Ministry of Health, hospitals are far from the recommended quality standards, with notable deficiencies in their capacity for resolution due to the lack of diagnostic aid methods and equipment; and weakness in the acquisition of medicines and supplies.20 This, together with the increase in the number of residents, reduces the number of procedures per resident and limits their practical training, as shown in our results. This situation is not exclusive to our country. A study in Australia showed that the number of trainees in nephrology specialization programs increased from 2004 to 2010, which resulted in the trainees' exposure to dialysis patients gradually decreasing, as well as the number of temporary hemodialysis catheters inserted and the number of renal biopsies.21 An outstanding example of this, which would explain the primary deficiency in the practical training area, is the lack of machines for slow therapies in the country's hospitals, which limits the training of our residents in this type of therapy.22 To overcome these limitations, some organizations have suggested using simulators to train nephrology residents in some procedures, which could be an alternative in our country.23
Although, in 2015, the completion of a research study to become a specialist was eliminated, being necessary to present a research project only,5 our results show that scientific activity experienced an increase among our residents. This may be related to the implementation of policies that promote research in our country after the enactment of the new university law24 and the need for accreditation of undergraduate medical programs by the National Superintendency of University Higher Education (SUNEDU), which proposed that 2 of its 3 accreditation standards are related to research.25 The efforts made by the medical programs in training and incorporation of teachers probably had an impact on the internal organization of the hospitals, where the students of these programs carry out their training, which may also have affected the research activities of the residents. These improvements are significant, although probably still isolated to the personnel involved in the modernization of undergraduate medical programs, given the large percentage of respondents who still do not consider their hospital to have a good academic level in research. Even though the accreditation of undergraduate medical programs was suspended due to internal changes at SUNEDU, the improvements implemented should continue and increase.
The COVID-19 pandemic disrupted the world's healthcare systems and impacted medical education.26 Although a survey of more than 1000 residents conducted by researchers of the American Society of Nephrology in 2020 showed that the respondents considered that the pandemic had a minimal impact on their academic training,16 our results show that, in our country, it did have a great impact. Our health system, as well as those of other countries, was not prepared to face the pandemic, which was one of the reasons why, at some point during the pandemic, we were the country with the most deaths due to this disease, including a high number of physicians.27,28 In this context, it is not surprising that nearly 7 out of 10 residents have been infected. Although outbreaks of COVID-19 have been reported among personnel in various hospitals or residents in our continent,29,30 as far as we know, such a high figure was not reported. This reflects the working conditions in our hospitals and the socioeconomic conditions and compliance with health protection measures in our country that led to a high infection rate.27,31 These conditions explain why many academic rotations established in the residency programs to complete their training were not performed, including rotations in foreign hospitals.26 Although, unfortunately, the universities have not provided alternatives to make up for these rotations, this could be because some were scheduled during lockdown measures or when hospitals limited health personnel as a biosecurity measure.27
Even though the general perception and job prospects are favorable, more than 80% of the respondents consider that the residency program in their hospitals should be improved. This discrepancy can be partially explained by the social desirability that prompts a better response on what is assessed but, in a question such as the latter, it shows their real opinion. In other words, the responses overestimate the perception of the various aspects assessed. Although we assessed perceptions and not the quality of the residency itself, other authors also assessed the perception of Nephrology residents about their training and published their research after our first assessment more than 10 years ago. Our results show that the general perception is related to some modifiable factors, such as the perception of the good level of research in their hospital and the performance of the tutor. This reinforces the need to continue SUNEDU's efforts in terms of university research25 and the need to strengthen the work of tutors. It should be noted that the appointment of a tutor does not have homogeneous criteria among universities, is usually not remunerated and its activities depend on the time available and the will of each tutor.
These studies show varying results regarding the perception of some aspects of a Nephrologist's training and differences in the rate of positive perception. In 2017, in Australia and New Zealand, an assessment among newly graduated residents showed that respondents indicated adequate training in most clinical skills except home hemodialysis, palliative care, automated peritoneal dialysis, and evaluation of kidney transplant recipients.32 Other areas in which they did not report being well trained were management and research skills.33 In 2020, another investigation in these countries showed that respondents felt that their training was adequate in most aspects of clinical nephrology; however, more than 80% of respondents felt poorly prepared to enter private practice, and more than 60% reported inadequate training in renal histopathology.33 Exposure to clinical procedures was variable, with adequate training in percutaneous renal biopsy but inadequate in dialysis access insertion.33 Another study among interns who received American Society of Nephrology (ASN) membership at the end of the 2015–2016 academic year showed that only 55% of second-year interns felt "fully prepared" for independent practice.34 In 2020, a study among French residents and young nephrologists showed that more than 70% considered that the teaching of central venous catheter placement during their residency was sufficient, although only 34.4% for the case of renal biopsy.35 In contrast, in 2018, another study in the United States showed that 83% of graduates of a Nephrology program felt they had adequate training in native kidney biopsy.36 These differences may reflect not only the different interests of the residents or the organizations that train them but also give some idea of differences in training practices between countries. In this sense, although our results are not comparable, they allow showing a general overview of some aspects that university authorities may consider improving the training of our residents.
Our study has some limitations. First, we could not obtain 100% participation of the residents in Peru, which may limit the generalizability of the results. Second, our assessment was on the perception of their training and not on its quality. Thirdly, we did not evaluate all the theoretical or practical aspects of the training of a nephrology resident. Despite this, we believe that our results show aspects in a representative sample of nephrology residents and graduates that will allow university authorities to propose strategies for improvement.
In conclusion, although the general perception of our nephrology residents and graduates is good, there are aspects related to procedural training and tutoring, among others, that are still deficient or have room for improvement. Both university and hospital authorities should propose strategies to improve the training of nephrologists in our country.
Name of the funding agencyThe authors declare no funding.
Indication of authors’ contributionConceptualization: Herrera-Añazco P, Rivas-Nieto AC, and Gomez Martin. Data curation: Rivas-Nieto AC3, Vicente Benites Zapata and Muñoz-del Carpio-Toia Agueda. Formal analysis: Vicente A. Benites-Zapata. Methodology: Herrera-Añazco P, Rivas-Nieto AC, Vicente Benites Zapata, Muñoz-del Carpio-Toia Agueda and Gomez Martin. Project administration and Supervision Percy Herrera-Añazco. Writing-original draft Percy Herrera-Añazco. Writing-review & editing: Herrera-Añazco P, Rivas-Nieto AC, Vicente Benites Zapata, Muñoz-del Carpio-Toia Agueda, Gomez Martin.