In North America, the role of Hepatologists in treatment of hepatocellular carcinoma is limited. We conducted a pilot project wherein a Hepatologist participated directly in microwave ablation of HCC at an academic center in the United States (n = 14). The pilot project shows promising outcomes, with complete remission rate of 93%.
In both transplant and non-transplant settings, the establishment of a multidisciplinary approach for patients with hepatocellular carcinoma (HCC) has been reported to improve outcomes.1,2 In North America, the management of HCC and survival outcomes is affected by having access to multidisciplinary tumor boards and specialists. The role of Hepatologists in active management of HCC is usually limited, however is associated with up to 30% reduction in mortality.3 We theorize that access to Interventional Radiology for care in tumor management may be limited to large tertiary-care facilities and academic institutions, whereas Hepatologists are more readily available in the community setting. We therefore conducted this pilot study to investigate the feasibility of Hepatology-directed microwave ablation (MWA) of HCC tumors in collaboration with Interventional Radiology at an academic liver transplant (LT) center in North America.
Material and MethodsWe reviewed a prospective cohort of consecutive HCC cases receiving MWA for tumor treatment administered by a Hepatologist Dr. Tomohiro Tanaka (TT), who is also the primary Hepatologist involved in the care of these patients at the University of Iowa - Division of Gastroenterology/Hepatology and Organ Transplant Center. TT has completed a fellowship in Gastroenterology/Hepatology at a high volume liver cancer center in Japan.4 This training included comprehensive hands-on teaching of tumor ablative techniques for liver cancers, under the direct supervision of experienced attending Hepatologists. Upon completion of the 3-year fellowship, TT had successfully completed over 120 ablations and was certified for independent practice in performing the procedures. At the onset of this project in January 2017, TT had over 10 years of experience practicing as a Hepatologist.
This project was conducted in collaboration with the Division of Interventional Radiology at the University of Iowa, where professional charges were divided equally amongst the two services depending on the primary practitioner.
The HCC diagnosis was confirmed by multiphase magnetic resonance imaging (MRI) or computed tomography (CT). Board-certified radiologists diagnosed HCC on the basis of Liver Imaging Reporting and Data System (LI-RADS). Prior to the procedure, all patients with LI-RADS 4 or 5 were reviewed at our Multidisciplinary Hepatobiliary Tumor Board.
MWA was performed from January 2017 to April 2018 under general anesthesia, using either Emprint Ablation System with Thermosphere Technology (Covidien, Boulder, CO) or Solero Microwave Tissue Ablation System (AngioDynamics, Latham, NY); both were used under real-time ultrasound guidance.
Follow-up was performed with multiphase MRI or CT following ablation. Time to initial imaging varied between 4 and 6 weeks. MRI or CT was obtained every 3 months to evaluate disease progression in those with an initial complete response (CR), or earlier in those without. Response was evaluated by modified response evaluation criteria in solid tumor (mRECIST) criteria.5 This project was approved by the institutional review board (#201708797).
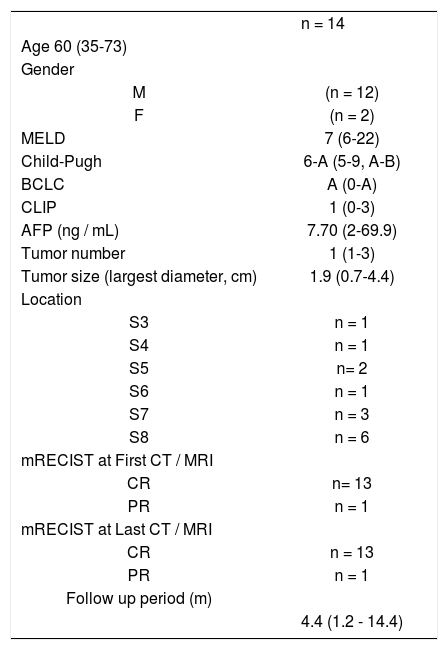
OutcomesDuring the study period, the Hepatologist conducted 14 cases of MWA for HCC (Table 1). The first 5 cases were by Emprint system and the following 8 were by Solero system. Median follow up period was 3.1 (1.2 - 13.4) months post-treatment. 13 patients had solitary lesions which were between 11-44 mm (median 20.5 mm) in diameter, with 1 patient having 2 smaller sub-centimeter nodules (LI-RADS4) that were not amenable to treatment. BCLC stages were 0-A for all 14 patients. CLIP scores were between 0 and 3, with a median of 1. No patients experienced adverse events related to the procedures. All of the 14 underwent at least one (range, 1-4) follow up CT or MRI with 13 (93%) achieving complete remission (CR) and 1, who initially had largest tumor size of 44 mm, achieving partial response (PR). The 1 patient with PR was not indicated for TACE due to non-tumor portal vein thrombosis, and was alive at the end of the study period. Only 1 patient died, from primary lung cancer which was diagnosed 8 months following the MWA for HCC, and no further liver lesions amenable to intervention were observed throughout the follow-up period. All other 12 patients were alive without local or distant recurrence at the end of the study period.
Profile of patients with HCC undergoing MWA.
| n = 14 | |
| Age 60 (35-73) | |
| Gender | |
| M | (n = 12) |
| F | (n = 2) |
| MELD | 7 (6-22) |
| Child-Pugh | 6-A (5-9, A-B) |
| BCLC | A (0-A) |
| CLIP | 1 (0-3) |
| AFP (ng / mL) | 7.70 (2-69.9) |
| Tumor number | 1 (1-3) |
| Tumor size (largest diameter, cm) | 1.9 (0.7-4.4) |
| Location | |
| S3 | n = 1 |
| S4 | n = 1 |
| S5 | n= 2 |
| S6 | n = 1 |
| S7 | n = 3 |
| S8 | n = 6 |
| mRECIST at First CT / MRI | |
| CR | n= 13 |
| PR | n = 1 |
| mRECIST at Last CT / MRI | |
| CR | n = 13 |
| PR | n = 1 |
| Follow up period (m) | |
| 4.4 (1.2 - 14.4) |
Hepatocellular carcinoma (HCC) is the fifth most common cancer and the second most frequent cause of cancer-related death worldwide.6 Liver resection, thermal ablation, and liver transplantation are potentially curative treatments, with 5-year survival up to 70%, with thermal ablative techniques being used for treatment of non-resectable HCC.6 No conclusive studies have been done comparing MWA to radiofrequency ablation (RFA), however likely advantages include shorter ablation time, less pain, and less heat sink effect. MW energy produces faster heating and higher temperatures, which results in better demarcated and larger area of necrosis as compared with RFA,6 thus MWA was chosen for this project.
The treatment of HCC is particularly complex, and thus often involves both tumor-specific (size, number, and portal vein thrombosis) and liver disease-specific (cirrhosis, portal hypertension and/or coagulopathy) considerations. Therefore, the delivery of care to patients with HCC is best conducted with a multidisciplinary approach.2,3 Although multiple studies have shown that multispecialty involvement in regards to treatment of HCC has overall improved survival benefit and patient outcomes, this is often limited by geographical limitations in access to facilities and specialists and may delay initiation of treatment.1,2 In the United States, thermal ablation has been traditionally conducted by trained Radiologists rather than Hepatologists. In contrast, in other parts of the world such as East Asia, Hepatologists have been trained in ultrasound-guided locolesional therapy.7 There are no studies comparing Hepatology-directed thermal ablation therapy to Radiology-directed procedures. We believe that allowing trained Hepatologists to play a pivotal and direct role in HCC treatment using ultrasound-guided MWA in collaboration with Radiologists is a new and innovative strategy to the comprehensive multidisciplinary team approach, with improved early access to treatment and improved patient survival and satisfaction.
The limitations of the pilot study include the relatively small number of patients enrolled thus far without a control arm. In addition, 1 out of the 14 patients died from primary lung cancer in addition to primary liver cancer. It is unlikely that the liver tumor treated was a metastatic lesion given negative chest imaging immediately before the initial diagnosis of HCC, however this has to be taken into consideration. The current training curriculum in North America for Gastrotenterology/Hepatology fellows typically does not include learning image-guided procedures for liver tumors including thermal ablative techniques, which may be an important future consideration for training programs.
Overall, Hepatology-directed thermal ablative management of HCC may be an innovative strategy to improving the patient access and treatment rates, decrease dropouts in LT waitlist, and ultimately allow for improved overall survival with a comprehensive multidisciplinary team approach. Further studies with large number of patients including a control arm and longer follow up period is required to draw more robust conclusions.
Abbreviations- •
CR: complete response.
- •
CT: computed tomography.
- •
HCC: hepatocellular carcinoma.
- •
LI-RADS: liver imaging reporting and data system.
- •
mRECIST: modified response evaluation criteria in solid tumor.
- •
MRI: magnetic resonance imaging.
- •
MWA: microwave ablation.
- •
PR: partial response.
- •
RFA: radiofrequency ablation.
The authors declares that there is no conflict of interest regarding the publication of this article.
FundingThis study is not funded.
Author ContributionsMSA (acquisition of data; drafting of the manuscript), TT (study concept and design; analysis and interpretation of data; critical revision of the manuscript), STL and SS (study concept and design; supervision of the study).