Introduction. Imaging surveillance and multidisciplinary conference (MDC) review can potentially improve survival in patients with hepatocellular carcinoma (HCC) by increasing access to liver transplantation. Geographic disparities in donor organ availability may reduce this benefit. This study evaluated the impact of HCC surveillance on use of curative therapies and survival in a region with long transplant waiting times.
Material and methods. 167 HCC patients were retrospectively studied. Subjects had an established HCC diagnosis or were diagnosed during hepatology follow-up. Collected data included patient demographics, HCC surveillance and MDC review status, portal hypertension complications, laboratory and radiologic parameters, tumor size, therapeutic interventions, tumor progression, and mortality. The primary outcome measures were use of curative treatments and survival. A Cox-regression model was constructed utilizing factors associated with survival in univariate analysis.
Results. 58% of subjects underwent surveillance and MDC review of HCC. These patients were more likely to have received treatment with ablation or resection (16 vs. 3%, P = 0.006) and transplantation (23 vs. 4%, P = 0.001), and were less likely to develop tumor progression (45 vs. 68%, P = 0.005) or metastases (0 vs. 19%, P < 0.001). In multivariate analysis, surveillance and MDC review (P = 0.034, HR 0.520, 95% CI 0.284–0.952), tumor meeting Milan criteria (P < 0.001, HR 0.329, 95% CI 0.178–0.607), curative therapy application (P = 0.048, HR 0.130, 95% CI 0.017–0.979), and transplantation (P = 0.004, HR 0.236, 95% CI 0.088–0.632) were associated with survival.
Conclusion. In conclusion, imaging surveillance and MDC review is associated with detection of early stage HCC, increased access to curative therapies and transplantation, and prolonged survival.
Hepatocellular carcinoma (HCC) is an aggressive malignancy and a significant cause of morbidity and mortality in the setting of chronic liver disease. The incidence of HCC in the United States has tripled over the past three decades, and prognosis remains dismal despite continued improvements in diagnosis and treatment; 5-year survival is less than 15%.1,2 The standard curative therapies for HCC include ra-diofrequency ablation (RFA) for small lesions, surgical resection, and orthotopic liver transplantation (OLT).3 Although resection and transplantation achieve 5-year survival rates approximating 50 and 70%, respectively, less than 15% of patients qualify for these procedures.3–5 Resection is generally precluded in patients with infiltrative or multifocal HCC, evidence of vascular invasion, or inadequate hepatic reserve, while transplantation is typically reserved for the small subset of patients who meet the Milan criteria and have no evidence of vascular invasion or extra-hepatic disease.6,7 Access to transplantation is further limited by donor organ availability and prolonged wait times. Sadly, waitlist dropout due to disease progression is not un-common,8 and transarterial therapies, including chemoembolization and yttrium-90 microsphere ra-dioembolization, have been used to bridge patients to transplantation.9
The American Association for the Study of Liver Disease (AASLD) recommends HCC surveillance in at-risk populations in order to identify early-stage tumors that are amenable to curative treatment.3 The combination of imaging surveillance and multi-disciplinary conference (MDC) review has been shown to improve both quality of life and overall survival in patients with HCC.10–16 Multidisciplinary teams typically consist of specialists in the fields of hepatology, transplant surgery, interventional radiology (IR), medical oncology, and surgical oncology who meet at regular intervals to review and coordinate patient care.17 Ideally, this paradigm may optimize outcomes by fostering a coordinated and consensus-based approach to diagnosis and management. However, it is conceivable that such a program may be less likely to prolong survival and increase transplant rates in regions where transplantation occurs at higher Model for End Stage Liver Disease (MELD) scores and after longer waiting periods. The current study was performed at a liver transplant center in region 7 where, in 2010, 31.4% of transplants within the organ provider organization (OPO) serving the transplant center occurred at a MELD ≥ 31. In contrast, nationally, only 20% of transplants occurred at a MELD ≥ 31,18 and a previous study10 evaluating the impact of HCC surveillance occurred in an area where only 9.1% of transplants occurred at a MELD ≥ 31.18 With this in mind, the current investigation was undertaken with the aim of assessing the impact of an imaging surveillance and MDC review program on access to curative therapy as well as survival outcomes in a large singlecenter cohort of HCC patients in a region with relatively limited donor organ availability.
Material and MethodsThis retrospective investigation received institutional review board approval with waiver of informed consent, and was conducted in compliance with the Health Information Portability and Accountability Act.
Clinical setting, study design, and patient cohort193 consecutive patients who were diagnosed with HCC between August 2007 and November 2011 were identified. Patients originated from either the hepatology clinic at our institution, a tertiary care academic hospital located in a large metropolitan area, or from outside referral sources. The hospital electronic medical record system was reviewed in order to collect patient demographic factors (age, gender, ethnicity, body mass index or BMI, history of alcohol use, type of insurance), laboratory parameters at the time of diagnosis (total bilirubin, creatinine, international normalized ratio or INR, alpha-fetoprotein or AFP levels), and disease characteristics (etiology, presence of ascites, hepatic encephalopathy, variceal bleeding). MELD scores were calculated based on laboratory values as opposed to MELD exception points in order to reflect the degree of hepatic dysfunction.
Subjects were dichotomized based on their prior history of HCC surveillance imaging and inclusion in MDC review. Surveillance was defined as a history of more than one imaging study to screen for HCC, including one study within the year prior to diagnosis. MDC review consisted of a weekly meeting of hepatologists, transplant surgeons, IRs, and medical oncologists who reviewed patient imaging and made consensus management decisions. Fourteen patients were excluded from the study because the indications for the relevant imaging studies were not discernible from chart review. An additional 12 patients were excluded due to lack of follow-up. HCC was diagnosed based on imaging criteria proposed by the AASLD practice guidelines3 or by percutaneous biopsy. All index radiographic studies were reviewed by a single radiologist (R.G.) who was blinded to clinical data. Patients were characterized as meeting or exceeding the Milan criteria based on the size and number of lesions.7 Subsequent imaging was reviewed to assess for tumor progression, which was based on enlarging areas of enhancement on dynamic imaging.
Measured outcomes and clinical follow-upThe outcome measures in this study included receipt of potentially curative therapy (radiofrequency ablation or RFA administered with curative intent, surgical resection, or OLT) and patient survival. Outcomes were evaluated until February 2011. The majority of patients (n = 128) underwent one or more locoregional therapies (such as transarterial chemoembolization, yttrium-90 radioembolization, and percutaneous ablation for local disease control) in order to reduce tumor burden and slow disease progression rather than cure, either as a primary treatment or as an adjuvant treatment while awaiting transplantation. Given their ubiquity in the study population, these interventions were not considered relevant endpoints. RFA was categorized as curative therapy in patients with T1 lesions, or based on the presence of contraindications to liver transplantation in patients with T2 lesions.3 Patients referred for OLT evaluation were assessed to determine whether they were listed, removed from the transplant list, or transplanted. Blood group was recorded for transplanted patients. Mortality data were obtained by review of the hospital electronic medical record and the Social Security Death Index. For each subject, the total time of follow-up began with the imaging diagnosis of HCC and ended at the date of death, last clinical follow-up, or the end of the data collection period.
Statistical analysisCategorical variables were assessed using Pearson’s chi-square, while normally distributed continuous variables were compared using the Student’s t-test. Survival was analyzed according to the Kaplan-Meier method and comparisons were made using the log-rank test. Multivariate analysis was performed with Cox-regression, in which factors associated with survival in univariate analysis (P < 0.10) were entered into the model and the results displayed with hazard ratio (HR) and 95% confidence intervals (CIs). Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 19 (IBM Corporation, Somers NY). P-values ≤ 0.05 were considered statistically significant.
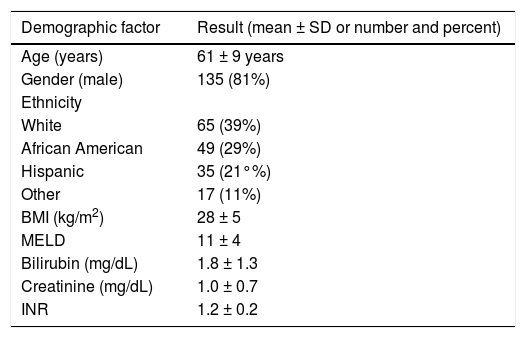
ResultsPatients and liver diseaseA total of 167 patients were included in the study cohort. Baseline demographic and laboratory data are presented in table 1. Causes of underlying liver disease included hepatitis C (n = 111) and hepatitis B (n = 20), non-alcoholic steatohepatitis (n = 29), autoimmune diseases (n = 8), and hereditary hemochromatosis (n = 2). In addition, 103 (62%) subjects reported a period of excessive alcohol use at some point in their life. Ascites, hepatic encephalopathy, and variceal bleeding were present in 43% (71/167), 26% (43/167), and 14% (24/167) of patients, respectively.
Clinical and laboratory data for the entire cohort of patients.
| Demographic factor | Result (mean ± SD or number and percent) |
|---|---|
| Age (years) | 61 ± 9 years |
| Gender (male) | 135 (81%) |
| Ethnicity | |
| White | 65 (39%) |
| African American | 49 (29%) |
| Hispanic | 35 (21°%) |
| Other | 17 (11%) |
| BMI (kg/m2) | 28 ± 5 |
| MELD | 11 ± 4 |
| Bilirubin (mg/dL) | 1.8 ± 1.3 |
| Creatinine (mg/dL) | 1.0 ± 0.7 |
| INR | 1.2 ± 0.2 |
SD: standard deviation. BMI: body mass index. INR: international normalized ratio.
The imaging surveillance and MDC review group had a higher BMI (29 ± 6 kg/m2vs. 27 ± 4 kg/m2, P = 0.003) and a higher rate of hepatic encephalopathy (37 vs. 22%, P = 0.050) than the no imaging surveillance group. There were no statistically significant differences in age, gender, ethnicity, liver disease etiology, excessive alcohol use, history of ascites or gastrointestinal bleeding, or MELD score between the two groups. Overall, the mean length of follow-up after HCC diagnosis was 451 ± 350 days. Mean follow-up was similar between the imaging surveillance and MDC review (457 ± 348 days) and the no imaging surveillance (442 ± 357 days) groups.
Surveillance and MDC review dataThe imaging surveillance and MDC review group consisted of 97 patients found to have evidence of HCC during follow-up, while the no imaging surveil lance group consisted of 70 patients diagnosed with HCC who had not undergone imaging for the purpose of HCC surveillance. Compared to the no surveil lance group, patients in the imaging surveillance and MDC review group were more likely have originated from the hepatology clinic at our tertiary care center versus outside referral sources (86 vs. 42%, P < 0.001). These patients were also more likely to have commercial insurance rather than Medicare or Medicaid (72 vs. 55%, P = 0.031).
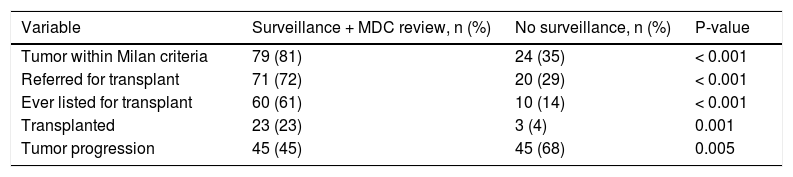
Tumor burdenPatients who underwent imaging surveillance and MDC review were more likely diagnosed with tumors within the Milan criteria as compared to those patients not undergoing surveillance (81 vs. 35%) (Table 2). Similarly, imaging surveillance patients had smaller index tumors (3.1 vs. 6.2 cm, P < 0.001) and were more likely to have unifocal instead of multifocal or infiltrative disease (62 vs. 38%, P = 0.002). Patients who adhered to imaging surveillance and MDC review were less likely to demonstrate tumor progression (45 vs. 68%, P = 0.005) (Table 2) and metastatic disease (0 vs. 19%, P < 0.001).
Transplant and tumor data dichotomized based on surveillance status prior to diagnosis.
| Variable | Surveillance + MDC review, n (%) | No surveillance, n (%) | P-value |
|---|---|---|---|
| Tumor within Milan criteria | 79 (81) | 24 (35) | < 0.001 |
| Referred for transplant | 71 (72) | 20 (29) | < 0.001 |
| Ever listed for transplant | 60 (61) | 10 (14) | < 0.001 |
| Transplanted | 23 (23) | 3 (4) | 0.001 |
| Tumor progression | 45 (45) | 45 (68) | 0.005 |
MDC: multidisciplinary conference.
Of note, nineteen patients in the imaging surveil lance and MDC review group had a tumor burden that exceeded the Milan criteria at the time of diagnosis. These patients were distinguished by a trend towards a higher rate of obesity (59 vs. 34%, P = 0.065) and a significantly higher rate of radiographic tumor progression compared to those patients in the imaging surveillance and MDC review group who fell within the Milan criteria (79 vs. 38%, P = 0.001).
Access to locoregional and curative therapiesAfter HCC diagnosis, both surveillance and nonsurveillance patients had similar access to non-curative locoregional therapies, including transarterial chemoembolization and yttrium-90 radioembolization (78 vs. 81%, P = 0.573) for local disease control. Notably, those patients in the no imaging surveillance group more frequently received salvage therapy with systemic sorafenib (Nexavar; Bayer Pharmaceuticals, Leverkusen Germany) (68 vs. 45%, P = 0.005).
When all potentially curative therapies (RFA, surgical resection, and OLT) were considered together, patients undergoing imaging surveillance and MDC review were more likely to have received a potentially curative treatment (40 vs. 7%, P < 0.001). Notably, there were no statistically significant differences in access to curative therapy based on major etiologies of underlying liver disease (viral versus non-viral and alcoholic versus non-alcoholic liver disease). In total, 18 patients received non-transplant curative therapies: 15 underwent RFA and 3 underwent surgical resection. Of the 15 subjects who were treated with RFA, nine had T1 lesions (tumor < 2 cm) and the remainder had T2 lesions within the Milan criteria with contraindications to transplantation. In the RFA group, two patients were subsequently listed for transplantation; one with cirrhosis and a T2 tumor later completed substance abuse counseling and the other developed HCC recurrence after ablation of a T1 lesion. At the completion of the study period, both patients were still awaiting liver transplantation.
Overall, evaluation for liver transplantation was performed in 55% (91/167) of subjects; 42% (70/167) were listed and 16% (26/167) underwent OLT. Eighteen patients received a donor liver with a MELD score based on tumor exception criteria; these individuals waited a mean of 188 ± 82 days for transplantation. The remaining patients either underwent live donor transplant (n = 2), or had a calculated MELD score that exceeded their score based on exception criteria (n = 6). Nine patients were dropped from the waitlist due to tumor progression, which occurred at a mean of 174 ± 116 days after listing with MELD exception criteria. At the time of data analysis, 12 patients were still awaiting OLT. The remaining patients were removed from the transplant waiting list due to medical instability (n = 7) or for such reasons as transfer of care, substance relapse, or patient decision. As shown in table 2, because those patients undergoing imaging surveillance more frequently met the Milan criteria, these individuals were significantly more often referred for transplantation, listed for transplantation, and transplanted.
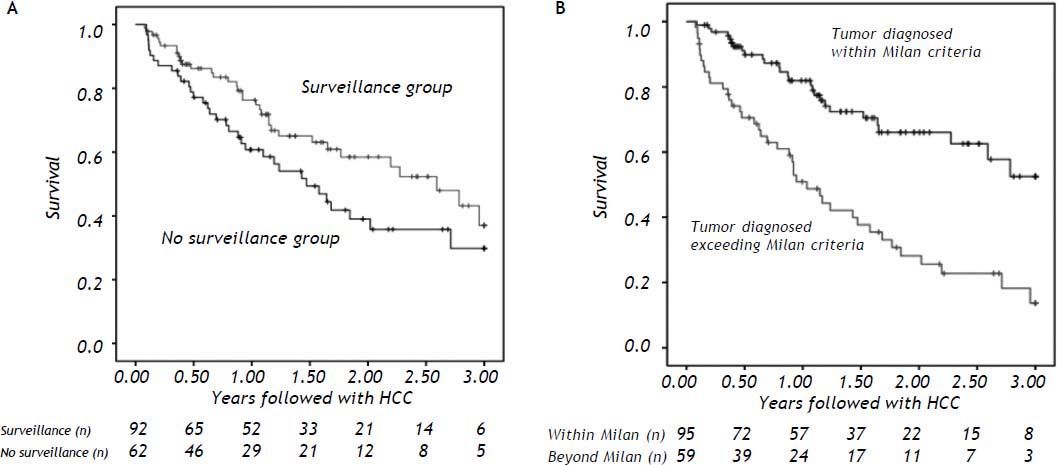
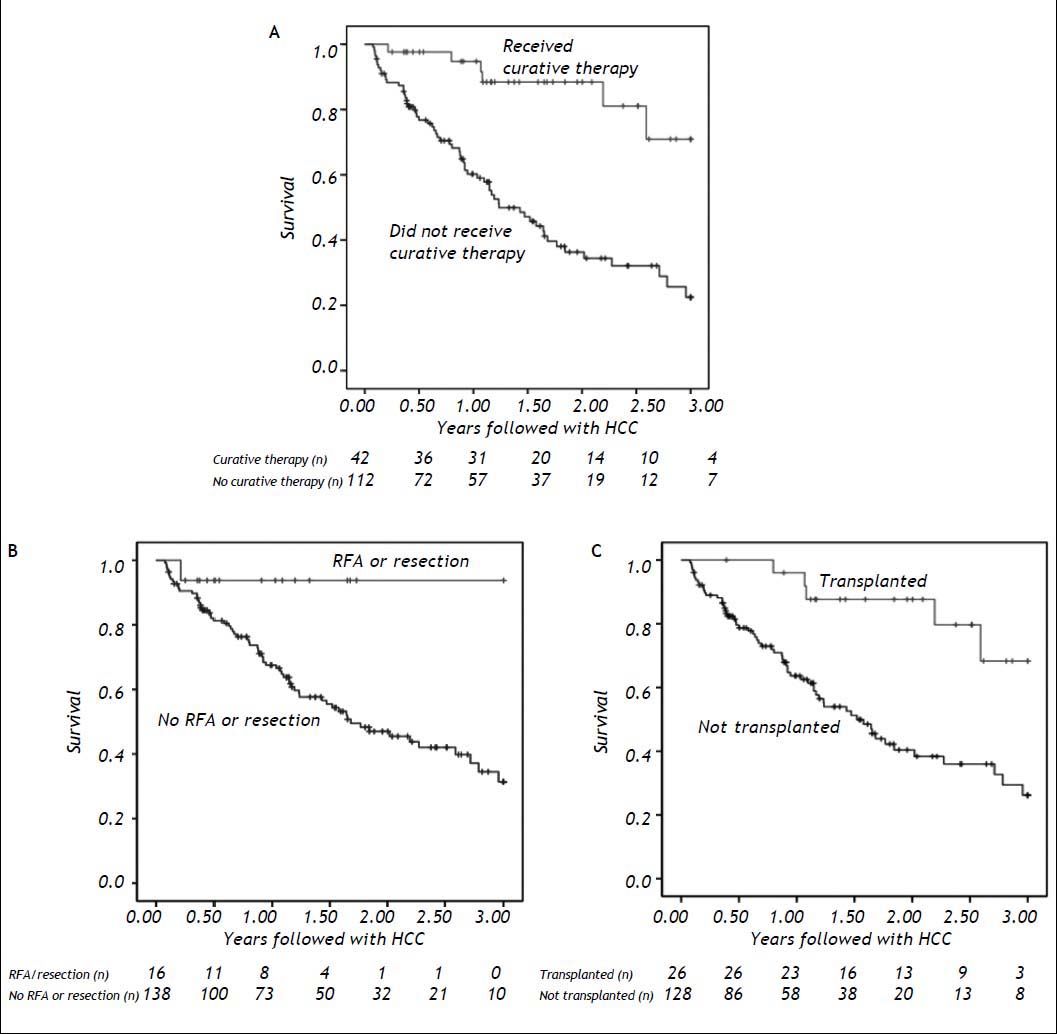
SurvivalSurvival data were available for 92% (154/167) of subjects. Of these, 53% (81/154) remained alive at the end of the study period. On univariate analysis, survival was associated with higher BMI and the absence of prior excess alcohol use (both P = 0.045). Gender, ethnicity, viral liver disease etiology, MELD score, complications of portal hypertension, and source of initial clinical follow-up (gastroenterology vs. hepatology practice) were not associated with survival. The patients who survived were less likely to have radiographic progression (41 vs. 73%, P < 0.001) or to have received sorafenib chemotherapy (22 vs. 42%, P = 0.010). Comparisons of KaplanMeier curves indicated higher survival rates in patients undergoing imaging surveillance and MDC review (Figure 1A) and in those with tumors within the Milan criteria (Figure 1B). Survival was also enhanced for individuals receiving any curative therapy (Figure 2A), RFA with curative intent or resection (Figure 2B), or OLT (Figure 2C).
Three-year survival curves with total number of subjects remaining at each time point shown in years. Survival benefit demonstrated for (A) patients receiving any curative therapy (P < 0.001), (B) patients who underwent resection or RFA with curative intent (P = 0.033), and (C) patients who had liver transplantation (P = 0.001).
Multivariate analysis revealed a significant association between survival and imaging surveillance and MDC review history (P = 0.034, HR 0.520, 95% CI 0.284-0.952), tumor within the Milan criteria (P < 0.001, HR 0.329, 95% CI 0.178–0.607), application of other curative therapies (P = 0.048, HR 0.130, 95% CI 0.017–0.979), and transplantation (P = 0.004, HR 0.236, 95% CI 0.088–0.632).
DiscussionIn this investigation, the use of imaging surveil lance and MDC review was associated with a significant survival benefit in patients with HCC. Patients who underwent imaging surveillance and MDC review were more likely to have tumors within the Milan criteria, to be referred for transplant evaluation and added to the transplant list, and to undergo potentially curative therapy. While HCC tended to be identified at an earlier stage in the surveillance group, the survival benefit identified herein cannot be entirely attributed to lead time bias, as the application of curative therapy was independently associated with survival. Importantly, imaging surveillance and MDC review was also associated with reduced rates of tumor progression and metastatic disease after HCC diagnosis, a finding likely related to enhanced detection of early stage HCC. The outcomes herein further validate the paradigm of imaging surveillance and MDC review in this patient population, even in a geographic region with relatively limited donor organ availability where liver transplantation routinely occurs at high MELD scores. HCC is a complex disease with an increasingly complex therapeutic algorithm that requires careful communication and coordination of care between a multifaceted network of specialists. The use of imaging surveillance and MDC review may facilitate the implementation and interpretation of standardized screening procedures, and thereby optimize the diagnosis, management, and outcomes of patients with HCC.
Geographic disparities in the availability of liver transplants pose a continued problem. In the current study, only one transplant occurred at a MELD < 25 and over half of transplants occurred at a MELD > 28. However, our findings are consistent with those of a previous series10 conducted in a region where transplantation occurred at lower MELD scores and after substantially shorter waiting times, thereby affirming the importance of the imaging surveillance and a MDC paradigm to prolong survival and increase access to curative therapies in areas where transplants occur routinely at higher MELD scores compared to the rest of the nation.18
Unfortunately, surveillance for HCC continues to be underutilized in the United States. In a large series of 1,873 patients with cirrhosis and HCC, only 55% had any form of screening prior to diagnosis and only 17% had adequate surveillance.11 Similarly, in this investigation only 58% of patients with HCC had previously undergone surveillance. Adherence with a surveillance imaging program was better in patients seen in a hepatology practice at a tertiary care center as compared to other medical facilities. More than twice as many patients underwent surveillance at our liver center as compared to patients referred from outside sources (86 vs. 42%). Interestingly, patients with hepatic encephalopathy were more likely to undergo surveillance, perhaps as a result of encephalopathy-related medical attention or hospitalization.
This investigation did not explore the reasons underlying low surveillance rates. However, the data represent the experience of a typical tertiary care practice where new HCC cases include patients referred for evaluation of a liver mass, as well as patients found to have HCC during the diagnoses and evaluation of cirrhosis or through surveillance during routine follow-up. Factors contributing to low surveillance rates may include under diagnosis of cirrhosis, patient non-adherence to a screening protocol, and insufficient physician awareness of the benefit of surveillance. The current study clearly indicates the importance of educating health care providers and patients about the value of imaging surveillance linked with a MDC review.
There were several limitations to the current investigation. First, this study was retrospective and non-randomized in nature. Second, the study was conducted at a single institution. Third, the utility of surveillance in the diagnosis of early stage tumors may result in lead-time bias. Although such bias would favor survival with small tumors, the Milan criteria is accepted by the United Network for Organ Sharing as providing the limit of tumor size for transplant exception criteria. Therefore, patients with tumors within the Milan criteria are more likely to receive curative therapy leading to long-term survival. Furthermore, imaging surveillance was strongly associated with the application of curative treatments, and the improved survival of patients undergoing curative therapy further supports this notion. Fourth, the overall duration of follow-up was relatively short in this retrospective study. However, we note that the follow-up time was sufficient to observe mortality events in more than 45% of cases. Finally, given the large proportion of subjects from outside referral sources, it was not possible to analyze the overall quality of surveillance.
In summary, this investigation further validates the survival benefit and increased access to curative treatment associated with surveillance and multidisciplinary review in patients at risk for HCC. Surveil lance and MDC also was associated with lower rates of HCC progression and metastatic disease. This paradigm may be especially important in areas served by OPOs with long waiting times. It is likely that the utility and necessity for surveillance with multi-disciplinary care will continue to increase as HCC therapy evolves.
Abbreviations
- •
HCC: hepatocellular carcinoma.
- •
RFA: radiofrequency ablation.
- •
OLT: orthotopic liver transplantation.
- •
AASLD: American Association for the Study of Liver Disease.
- •
MDC: multidisciplinary conference.
- •
IR: interventional radiology.
- •
MELD: Model for End Stage Liver Disease.
- •
OPO: organ provider organization.
- •
INR: international normalized ratio.
- •
AFP: alpha-fetoprotein.
- •
HR: hazard ratio.
- •
CI: confidence interval.
- •
SPSS: Statistical Package for the Social Sciences.
None.