A descriptive analysis of day-case laparoscopic cholecystectomy (ALC) in a cohort of 1600 consecutive patients performed in Instituto de Cirugía y Aparato Digestivo (ICAD), Clínica Quirón de Valencia in the period 1997–2010.
Patients and methodsProspective observational study of 1601 consecutive patients undergoing elective laparoscopic cholecystectomy (LC) provided by the regional health service and private health companies.
Main measuresConversion rate, non-planned admissions, readmissions, surgery duration and demographics.
ResultsALC was successfully performed in 80.8% of cases. LC with over-night (ON) stay accounted for 13.4% of patients. Admission was necessary in 4.6%. Mortality was 0.13%, 0.08 in ALC and 0.5% in ON LC. Readmissions occurred in 2.1%, 1.6% in ALC group, 5.4% in ON stay and 4.2% in admission group.
ConclusionsALC is a reliable and safe procedure. Minimization of admission rates is the key for cost-effective optimization in the management of cholelithiasis. ALC should be considered as the reference standard in gallbladder stone disease treatment.
Describir la experiencia de nuestro grupo en colecistectomía laparoscópica ambulatoria en una cohorte de 1.600 casos consecutivos realizados en el Instituto de Cirugía y Aparato (CLA) Digestivo (ICAD) en la Clínica Quirón de Valencia durante el período 1997-2010.
Pacientes y métodoEstudio prospectivo, observacional de 1.601 pacientes consecutivos remitidos para colecistectomía laparoscópica, procedentes de la Agencia Valenciana de Salud (AVS) y compañías aseguradoras privadas (CAP).
Principales medidas de resultados: se evalúan los resultados con el análisis de índice de sustitución, tasa de ingresos no planeados, reingresos, estancia postoperatoria, duración de intervención y factores demográficos.
ResultadosEl índice de sustitución de la serie fue de 80,8% con un porcentaje de pacientes intervenidos en régimen de estancia over-night (EON) de 13,4% y un porcentaje de ingresos en hospitalización convencional de 4,6%. La mortalidad de la serie fue de 0,13%, 0,08 en el grupo de CLA y 0,5% en el grupo de CL con EON. El índice de reingresos fue de 2,1% en la serie global, 1,6% en los pacientes ambulatorios, 5,4% en los pacientes con EON y 4,2% en los pacientes ingresados.
ConclusionesLa CLA es un procedimiento seguro y fiable. La reducción en la necesidad de ingreso de los pacientes es fundamental en la optimización coste efectividad del procedimiento de colecistectomía. La CLA debería ser considerada como el patrón oro del tratamiento de la colelitiasis sintomática.
Cholecystectomy is the most common major surgery performed in a general surgery department. It is considered a “tracer” process due to its prevalence, population impact, high clinical variability and substantial use of resources while representing the overall quality of a surgery department.1 In our country, the number of annual laparoscopic cholecystectomies (LC) is approximately 31000 cases, equal to the number of inguinal hernioplasties.2
After the introduction of LC by Muhe3 and the controversy that it caused,4 in only 4 years laparoscopic cholecystectomy was developed as an ambulatory procedure (ALC)5,6 and introduced in 1990. This sparked a new debate about its appropriateness as an ambulatory procedure7 despite its progressive extension.
Increased healthcare expenses as well as social and political pressure to improve surgical efficiency make ALC attractive but challenging. In 1977, the economic crisis propelled major ambulatory surgery (MOS) as a treatment that united quality care with cost rationalization.8 Today's economic situation is another opportunity for the healthcare system9 to promote ALC in order to lower costs while raising healthcare quality and maintaining services, contributing to sustainability.
The objective of this study is to describe the experience accumulated by our group over the course of 14 years practicing ALC in a series of 1600 consecutive patients.
Materials and MethodsThis prospective, observational, controlled, descriptive, non-randomized study included 1601 consecutive patients who underwent ALC during a 14-year period (1997–2010). The patients came from the Valencian Healthcare Agency (VHA) (plan of action to reduce waiting lists) and private healthcare providers.
The surgical interventions were performed without specific infrastructure in a day surgery unit, using the area adjacent to the operating room as a post-anesthesia recovery area and the day hospital as the recovery room; in this manner, MOS is integrated into the surgical block with day hospitalization.
Seven surgeons were included during the period analyzed with different levels of experience in LC, although they were combined homogenously.
The patients included had been referred for elective cholecystectomy, regardless of the prior existence of complicated cholelithiasis (acute cholecystitis, biliary pancreatitis or jaundice-choledocholithiasis previously treated with endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy [ERCP-ES]). The preoperative exam included liver function tests and a recent abdominal ultrasound. In patients with alterations suggestive of choledocholithiasis,10 preoperative magnetic resonance cholangiography (MRC) was mandatory. The indication of intraoperative cholangiography was based on uncertain findings in the MRC. Preoperative ERCP-ES was considered only in cases of choledocholithiasis documented by MRC. Postoperative ERCP-ES was performed in cases with symptoms of residual choledocholithiasis (RCDL), once diagnosis was established by MRC or when intraoperative cholangiography was diagnostic for choledocholithiasis.
The patients were admitted on the morning of the surgery. The anesthesia procedure included minimization of opioids, selective use of antiemetics in cases of GERD/hiatal hernia and systemic nasogastric intubation, which was withdrawn at the end of the procedure.
The surgical technique included 4 trocars and different types of nerve-block anesthesia to prevent surgical (parietal block) and intraperitoneal (visceral block) wounds with local anesthetics in order to reach optimal somato-visceral block.11
Hilar dissection was carried out in accordance with the principles of critical view safety (CVS) by Strasberg12 and the systematic identification of Rouviere's sulcus.13 Before the clamping and dividing, we proceeded with cholecystectomy at the neck to leave the hilar elements hanging for maximum safety (hanging maneuver). At the end of the procedure, the subhepatic and subphrenic area was thoroughly washed and suctioned, flooded with saline for the under-water inspection of the hepatic bed and hilum in order to find evidence of even minimal hemorrhage or bile leak. The use of local hemostatic agents and drainage was minimized.
Extraction was carried out without a bag except in cases of cholecystitis, empyema, and polypoid gallbladder lesions larger than 0.5cm or a gallbladder wall with suspected neoplasm. The umbilical port was closed with standard nonabsorbable suture.
The patients were then taken to a recovery area adjacent to the operating room. After reaching a satisfactory level of consciousness (30min), patients were given a sweetened soda (Coca-Cola®) based on the fast post-surgery recovery principles of Kehlet14 and publications from the past 111 years.15 Patients were then instructed to sit up and transferred to the day hospital with the venous catheter heparinized where they were encouraged to walk around freely, start oral intake and request analgesia as necessary. In cases of postoperative nausea and vomiting, treatment was begun with metoclopramide and, in persistent cases, ondansetron was administered.
At 3pm, the patients were reviewed and given home postoperative instructions, with special emphasis on alarm symptoms that require immediate contact with the surgical team. Patients were discharged by the surgeons between 4 and 7pm. At the beginning of our experience with this system, it was mandatory for patients to communicate with the surgeon at 9:30pm, but this was substituted for telephone follow-up the day after the surgery at case number 700, which was also suppressed by case number 850.
The patients were visited 72h later; the staples were removed and the surveys about patient perception of quality of care were filled out. Subsequent follow-up visits included: after one week (review of the pathology results), 14 days, 30 days and periodically during the first year (the patients have free access to the consultation). This enabled us to evaluate the development of RCDL, subhepatic collections, need for emergency home or hospital care, and development of trocar hernia and the usefulness of the procedure as determined by the Gastrointestinal Quality of Life Index (GIQLI).
The possibility of RCDL was contemplated when patients presented biliary colic and enzyme changes. If the ultrasound showed dilated bile duct (BD) or RCDL, the patient was studied with MRC; if confirmed, and depending on the clinical–analytical evolution and the size and number of stones, ERCP-ES was used or treatment with ursodeoxycholic acid (UDCA) was administered for a variable period of time.
ALC was defined as post-op stay of less than 12h (time limit of discharge was 7pm), compared with overnight (ON) stay, defined as overnight stay with discharge in the morning (less than 24h). Hospitalized patients were those who were treated under the conventional hospitalization regimen.
The statistical study was performed with the SPSS program. The continuous variables were analyzed with the Student's t-test and the categorical variables with the Chi squared test. A P<.05 was considered statistically significant.
ResultsThe sample was made up of a total of 1601 consecutive patients, out of which 20 outpatients without complications were excluded (1.2%) due to inadequate compliance of the follow-up within the first 30 days post-op. ALC was done in 1313 cases (82.0%), ON-LC in 214 (13.4%) and 74 with hospitalization (4.6%). Therefore, the index of non-programmed hospitalizations (INP) was 18.0%.
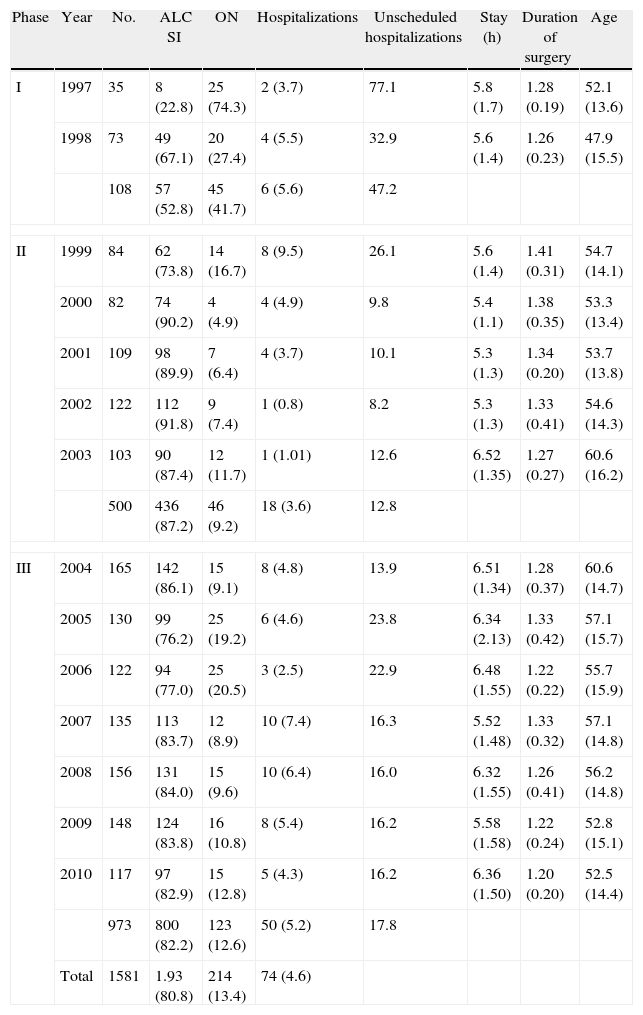
Table 1 shows the evolution of the series (substitution index [SI], INP, ON-LC, and hospitalization, together with mean age, mean surgery duration and postoperative stay in hours of the outpatients) according to the 3 periods defined: the first, project planning and assay modification (1997–1998); the second, evaluation of the process, implementation, monitoring and standardization (1999–2003); and the third, continuous reevaluation (2004–2010).
Cases.
| Phase | Year | No. | ALC SI | ON | Hospitalizations | Unscheduled hospitalizations | Stay (h) | Duration of surgery | Age |
| I | 1997 | 35 | 8 (22.8) | 25 (74.3) | 2 (3.7) | 77.1 | 5.8 (1.7) | 1.28 (0.19) | 52.1 (13.6) |
| 1998 | 73 | 49 (67.1) | 20 (27.4) | 4 (5.5) | 32.9 | 5.6 (1.4) | 1.26 (0.23) | 47.9 (15.5) | |
| 108 | 57 (52.8) | 45 (41.7) | 6 (5.6) | 47.2 | |||||
| II | 1999 | 84 | 62 (73.8) | 14 (16.7) | 8 (9.5) | 26.1 | 5.6 (1.4) | 1.41 (0.31) | 54.7 (14.1) |
| 2000 | 82 | 74 (90.2) | 4 (4.9) | 4 (4.9) | 9.8 | 5.4 (1.1) | 1.38 (0.35) | 53.3 (13.4) | |
| 2001 | 109 | 98 (89.9) | 7 (6.4) | 4 (3.7) | 10.1 | 5.3 (1.3) | 1.34 (0.20) | 53.7 (13.8) | |
| 2002 | 122 | 112 (91.8) | 9 (7.4) | 1 (0.8) | 8.2 | 5.3 (1.3) | 1.33 (0.41) | 54.6 (14.3) | |
| 2003 | 103 | 90 (87.4) | 12 (11.7) | 1 (1.01) | 12.6 | 6.52 (1.35) | 1.27 (0.27) | 60.6 (16.2) | |
| 500 | 436 (87.2) | 46 (9.2) | 18 (3.6) | 12.8 | |||||
| III | 2004 | 165 | 142 (86.1) | 15 (9.1) | 8 (4.8) | 13.9 | 6.51 (1.34) | 1.28 (0.37) | 60.6 (14.7) |
| 2005 | 130 | 99 (76.2) | 25 (19.2) | 6 (4.6) | 23.8 | 6.34 (2.13) | 1.33 (0.42) | 57.1 (15.7) | |
| 2006 | 122 | 94 (77.0) | 25 (20.5) | 3 (2.5) | 22.9 | 6.48 (1.55) | 1.22 (0.22) | 55.7 (15.9) | |
| 2007 | 135 | 113 (83.7) | 12 (8.9) | 10 (7.4) | 16.3 | 5.52 (1.48) | 1.33 (0.32) | 57.1 (14.8) | |
| 2008 | 156 | 131 (84.0) | 15 (9.6) | 10 (6.4) | 16.0 | 6.32 (1.55) | 1.26 (0.41) | 56.2 (14.8) | |
| 2009 | 148 | 124 (83.8) | 16 (10.8) | 8 (5.4) | 16.2 | 5.58 (1.58) | 1.22 (0.24) | 52.8 (15.1) | |
| 2010 | 117 | 97 (82.9) | 15 (12.8) | 5 (4.3) | 16.2 | 6.36 (1.50) | 1.20 (0.20) | 52.5 (14.4) | |
| 973 | 800 (82.2) | 123 (12.6) | 50 (5.2) | 17.8 | |||||
| Total | 1581 | 1.93 (80.8) | 214 (13.4) | 74 (4.6) | |||||
ALC, ambulatory laparoscopic cholecystectomy; ON, overnight stay; SI, substitution index.
The SI and INP in these three periods changed from 52.8 to 87.2 and 82.2% for the former and from 47.2 to 12.8 and 17.8% for the latter. In the first period (1997–1998), the SI went from 22.8% to 67.1% and the percentage of ON stay dropped from 74.3% to 27.4%, while hospitalizations were reduced to 3.7%–5.5% as the shortened postoperative system was learnt and the team gained in confidence. From 1999 to 2002, the SI increased, reaching a maximum of 91.8%, reducing ON stay to 7.4% and hospitalizations to 0.8%. In the period from 2005 to 2006, there was an increase in ON to 19.2%–20.5% due to the incorporation of new surgeons who needed to learn the fast post-op system. An SI plateau of around 80% was then reached, which continues to persist until now, while a stable INP percentage has been maintained at 16%, with a hospitalization rate between 4.3% and 7%.
Mean age was 55.5 (52.1–60.6) and the mean operating room time per patient was 1.3 (1.2–1.4)h. No significant variations were observed during the period analyzed, except for the period 2003–2004 (60.6 years).
The mean postoperative stay in outpatients of 5.5h (5.3–6.5) was stable throughout the period with slight oscillations that showed no statistical significance. 20% of patients were discharged in 4h or less, 70.1% between 5 and 8h and 22% required stays of 8h or more.
The conversion rate of the series was 16 cases (0.99%).
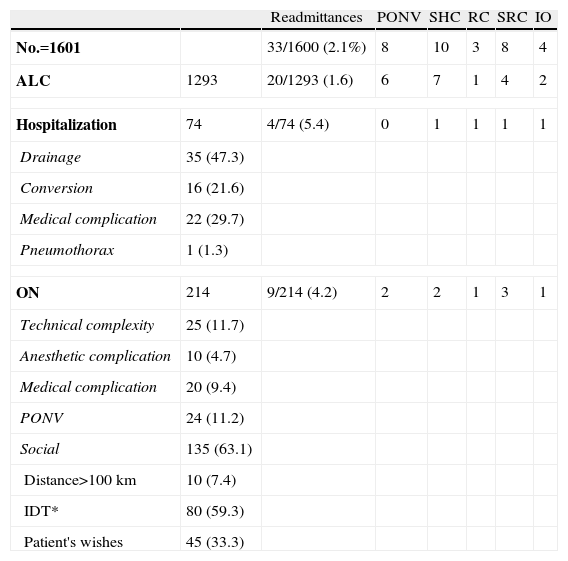
Table 2 shows the case distribution according to type of stay (ALC, ON-LC, and hospitalization), their causes and the readmittance rate, both overall and by hospitalization modality. The overall rate of readmittances was 2.1%: 1.6% in the ALC group, 4.2% in the ON group and 5.4% in the hospitalization group. The most frequent causes of readmittance were subhepatic collection and suspicion of RCDL.
Unplanned Hospitalizations/Readmittances.
| Readmittances | PONV | SHC | RC | SRC | IO | ||
| No.=1601 | 33/1600 (2.1%) | 8 | 10 | 3 | 8 | 4 | |
| ALC | 1293 | 20/1293 (1.6) | 6 | 7 | 1 | 4 | 2 |
| Hospitalization | 74 | 4/74 (5.4) | 0 | 1 | 1 | 1 | 1 |
| Drainage | 35 (47.3) | ||||||
| Conversion | 16 (21.6) | ||||||
| Medical complication | 22 (29.7) | ||||||
| Pneumothorax | 1 (1.3) | ||||||
| ON | 214 | 9/214 (4.2) | 2 | 2 | 1 | 3 | 1 |
| Technical complexity | 25 (11.7) | ||||||
| Anesthetic complication | 10 (4.7) | ||||||
| Medical complication | 20 (9.4) | ||||||
| PONV | 24 (11.2) | ||||||
| Social | 135 (63.1) | ||||||
| Distance>100km | 10 (7.4) | ||||||
| IDT* | 80 (59.3) | ||||||
| Patient's wishes | 45 (33.3) | ||||||
ALC, ambulatory laparoscopic cholecystectomy; CR, residual choledocholithiasis; SHC, sub hepatic collection; ON, overnight stay; IDT, inappropriate discharge time; PONV, postoperative nauseas/vomiting; IO, intestinal obstruction; SRC, suspected residual choledocholithiasis.
Out of the 10 cases with subhepatic collection, 3 were secondary to duct of Luschka biliary fistula (biloma with negative MRC) and 3 were due to non-biliary subhepatic collection requiring percutaneous drainage (No.=6). Another 4 cases of subhepatic collection were resolved with IV antibiotic therapy.
Out of the 11 cases (0.69%) with a suspicion of RCDL, only 3 were confirmed by means of MRC, one of which required ERCP-ES and the other 2 were resolved with dissolutive treatment with UDCA. The other 8 cases presented normal MRC and ultrasound findings, so the spontaneous passage of small-sized stones was assumed.
Overall mortality of the series was 2 cases (0.13%): one case (0.08%) in the ambulatory group (intestinal obstruction and multiple organ failure possibly secondary to Richter's hernia in the orifice of the umbilical trocar) and one case in the ON group (0.5%) (massive AMI 10h after the intervention, as established by necropsy).
BD injury was seen in one case (0.06%); Roux-en-y hepaticojejunostomy was performed with satisfactory post-op and no relevant complications.
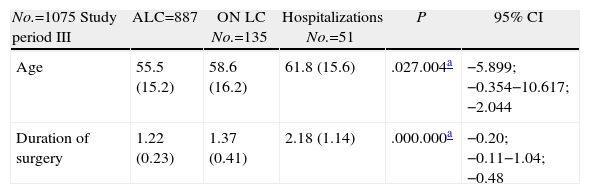
Table 3 shows the factors predicting day surgery in period III and at the end of period II,made up of 1075 cases. The univariate study showed evidence of age, surgery duration, age over 70, male sex and time of the surgical intervention as factors predicting outpatient treatment. The patients from private healthcare providers presented a higher percentage of hospitalizations (8.8% vs 1.4%) due to a higher percentage of complicated cholelithiasis and afternoon scheduling, although the percentage of ambulatory treatment was no different from the group of patients from the VHA (86.9% vs 77.7%), nor was there any difference in ON stay (13.5 vs 11.8). Afternoon surgery was a significant factor in outpatient surgery compared with morning surgery (37.7% vs 86.2%, respectively).
Predictive Factors for Ambulatory Surgery.
| No.=1075 Study period III | ALC=887 | ON LC No.=135 | Hospitalizations No.=51 | P | 95% CI |
| Age | 55.5 (15.2) | 58.6 (16.2) | 61.8 (15.6) | .027.004a | −5.899;−0.354−10.617; −2.044 |
| Duration of surgery | 1.22 (0.23) | 1.37 (0.41) | 2.18 (1.14) | .000.000a | −0.20; −0.11−1.04; −0.48 |
| Variable | ALC | ON LC | Hospitalizations | Chi S | P |
| Duration >90min (446) | 336 (75.3) | 67 (15.1) | 43 (9.6) | 47.35 | .000 |
| Duration <90min (630) | 554 (87.9) | 68 (10.8) | 8 (1.3) | ||
| Duration >120min (134) | 75 (56.0) | 32 (23.9) | 27 (20.1) | 105.6 | .000 |
| Duration <120min (942) | 815 (86.2) | 103 (10.9) | 24 (2.5) | ||
| Age≥70 (247) | 188 (76.1) | 41 (16.6) | 18 (7.3) | 10.27 | .006 |
| Age<70 (829) | 702 (84.7) | 94 (11.3) | 51 (4.7) | ||
| Males (331) | 261 (78.9) | 43 (13.0) | 27 (8.2) | 12.7 | .002 |
| Females (744) | 628 (84.4) | 92 (12.4) | 24 (3.2) | ||
| VHA (587) | 510 (86.9) | 69 (11.8) | 8 (1.4) | 31.4 | .000 |
| PHP (489) | 380 (77.7) | 66 (13.5) | 43 (8.8) | ||
| Morning surgery (999) | 861 (86.2) | 108 (10.8) | 30 (3.0) | 54.3 | .000 |
| Afternoon surgery (77) | 29 (37.7) | 27 (35.0) | 21 (27.2) |
| Age≥70 (n=247) | Age<70 (n=829) | P | 95% CI | |
| Age | 76.39 (5.01) | 50.1 (11.85) | .000 | 24.767; 27.805 |
| Mean stay | 0.83 (2.98) | 0.34 (1.40) | .000 | 0.223; 0.759 |
| Duration of surgery | 1.30 (0.38) | 1.25 (0.31) | .027 | 0.00; 0.090 |
| Interval at discharge (ALC) | 4.48 (4.20) | 5.14 (3.41) | .117 | 0.59; 0.06 |
ALC: ambulatory LC; ON LC: overnight LC; VHA: Valencian Healthcare Agency; PHP: private healthcare provider.
The duration of the intervention varied according to age. Nevertheless, the interval until discharge in the outpatients showed no significant differences for age (70), implying a similar postoperative recovery interval.
The multivariate analysis (binary logistic regression) showed as independent factors predictive of day surgery: morning/afternoon surgery (F=154.4; P=.0001; coefficient [C]=23.8), surgery duration (F=71.4; P=.001; C=0.002) and age >70 (F=13.8; P=.0001; C=9.8). The percentage of correct classification of the series with the logistic regression equation was 86.7% (Chi S=164.4; P=.0001; Gl=3).
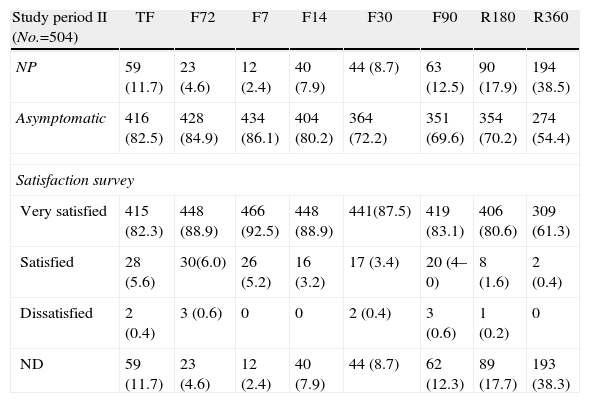
Table 4 shows the outpatient follow-up for 504 cases from the second period. There is a gradual descent in compliance with follow-up visits of up to 38.5% one year later. The degree of satisfaction expressed was either satisfactory of very satisfactory in 98% on the 7th day post-op and 100% in the patients who completed the annual follow-up visit (61.7% of the series from period II).
Postoperative Follow-up and Perceived Quality.
| Study period II (No.=504) | TF | F72 | F7 | F14 | F30 | F90 | R180 | R360 |
| NP | 59 (11.7) | 23 (4.6) | 12 (2.4) | 40 (7.9) | 44 (8.7) | 63 (12.5) | 90 (17.9) | 194 (38.5) |
| Asymptomatic | 416 (82.5) | 428 (84.9) | 434 (86.1) | 404 (80.2) | 364 (72.2) | 351 (69.6) | 354 (70.2) | 274 (54.4) |
| Satisfaction survey | ||||||||
| Very satisfied | 415 (82.3) | 448 (88.9) | 466 (92.5) | 448 (88.9) | 441(87.5) | 419 (83.1) | 406 (80.6) | 309 (61.3) |
| Satisfied | 28 (5.6) | 30(6.0) | 26 (5.2) | 16 (3.2) | 17 (3.4) | 20 (4–0) | 8 (1.6) | 2 (0.4) |
| Dissatisfied | 2 (0.4) | 3 (0.6) | 0 | 0 | 2 (0.4) | 3 (0.6) | 1 (0.2) | 0 |
| ND | 59 (11.7) | 23 (4.6) | 12 (2.4) | 40 (7.9) | 44 (8.7) | 62 (12.3) | 89 (17.7) | 193 (38.3) |
F72, 72-h follow-up; F7, 7th day post-op follow-up; F14, 14th day post-op follow-op; F30, 30th day post-op follow-up; F90, 3-month post-op follow-up; F180, 6-month post-op follow-up; F360, annual follow-up; TF, telephone follow-up; NP, not performed; ND, not declared.
Since the introduction of ALC by Reddick and Arregui in the 1990s,5,6 its feasibility, effectiveness and safety have been demonstrated16 with lower costs and a high level of patient satisfaction.17 It is therefore a procedure that is attractive to both surgeons and healthcare administrators,18 with a SI of nearly 70%19 that is progressively reaching a greater number of centers.
The recent Cochrane review obtained equivalent results between ALC and ALC-ON in terms of safety, complications and satisfaction.20 A meta-analysis by Gurusamy of 569 RCT on ALC vs ON-LC concluded that post-op abdominal pain (POAP) and post-op nausea/vomiting are the factors that most influence ambulatory surgery.
In economic terms, ALC reduces costs by 11% compared with ON-LC21 due to the reduction in postoperative costs (approximately 20%), 31% of which are nursing costs.
In Catalonia, Spain in 2005–2006, mean hospital stay of LC ranged between 2.9 and 8.1 days22; a SI of 70% would mean a savings of 46200 hospitalizations and 18 million euros. In 2009 in Spain, 31131 LC were performed, with a mean stay of 2.1–3.5 days (108370 hospitalizations)2; and a SI of 70% would mean a savings of 76 million euros, without including the minimized treatment and postoperative care.
In terms of cost-effectiveness, LC with hospitalization is more expensive and shows no greater clinical utility than minilaparotomy/small-incision cholecystectomy (SIC)23 (difference in costs 432 vs 826 euros and similar quality of life [EuroQol-5DVAS] at 7 and 30 days). The Cochrane analysis shows no differences in results (mortality and complication) between the 3 variations of cholecystectomy: open, SIC and LC.24 There was, however, a greater cost for LC; therefore, in terms of cost-effectiveness, SIC would be the technique of choice from a hospital/social/economic perspective, and the only way to increase the cost-effectiveness of LC, justifying this type of care compared with its alternatives, is ambulatory surgery.
In our country, the initial communications about ALC appeared in 1998,25 together with the publication by Martin.26 Subsequently, series descriptions,27–30 predictive factor analyses,31 selection criteria32 and perceived quality analyses33 have been published.
Unfortunately, the implementation and extension of the procedure are limited and, what is worse, some groups have interrupted their activity34 due to, among other causes, the peace of mind of surgeons and patients’ families as well as afternoon scheduling. Nevertheless, the greatest impediments are: organizing the scheduling of anesthetists and surgeons in day surgery units, little or no consideration given to ambulatory surgery by laparoscopic surgeons, as they consider MOS a residual activity, the lack of economic or professional incentives, legal insecurity and, the lack of interest (or manifest ignorance) of the public and private healthcare systems.35 Although the cause may be multifactorial, the concept of anesthetic-surgical optimization that minimizes the impact on patients and provides outpatient care and, therefore, maximum efficacy and efficiency continue to be underrated in favor of numerical productivity without evaluating the continued improvement in quality and results.
The objective argument against the implementation of ALC is the potential development of BD hemorrhage or damage, and most surgeons prefer 24-h observation for this reason. This is not supported by clinical evidence, as serious postoperative hemorrhage is uncommon (1/2000 cases) but symptomatic and detectable during the immediate post-op period.36 Meanwhile, BD injury becomes symptomatic after 24–48h.37 Thus, a post-op period of observation of 6–10h or less is safe and reliable.36,37
The acceptance of ALC mainly depends on the control of postoperative abdominal pain and nausea/vomiting, but it also depends on cultural and social expectations of patients and family members, as well as the medical culture (primary and specialized) they are in contact with.35 In this context, the most common cause for unscheduled hospitalizations in our series was social, related with the cultural factor.
The incidence of POAP is almost 30% of patients on the first post-op day,12 including: pain in the trocar wounds (especially in the navel area), visceral pain and omalgia (incidence from 30% to 50%).11 The most relevant factor that influences the degree of visceral POAP is the surgical technique since exquisite dissection and absence of residual bile or blood in the abdominal cavity minimize it.37,38
It is vital to reduce POAP.11 The use of local intraperitoneal anesthesia is safe, significantly reducing POAP and increasing day surgery rates. It is most effective in greater concentration and if instilled before initiating dissection, so somato-visceral nerve block is essential for the success of ALC.11
It is fundamental that the continuous care during the immediate postoperative day surgery period be provided by the same surgical team39 and directed by surgeons trained in the shortened post-op recovery principles of this procedure, avoiding the heterogeneity of clinical practice, which can have disastrous effects in ALC.
The implications of the implementation of ALC in Spain would entail a savings of some 70 million euros (in reduced hospital stay costs),2 without taking into account the costs eliminated from healthcare during hospitalization. This means that ALC should be a key objective in surgical units, especially now when so many measures are being proposed and it is uncertain whether they can actually sustain the system.
In conclusion, our study supports the safety, reliability and possibility for continued development, improvement and implementation of ALC, with a demonstrated high degree of patient satisfaction. Our data advocate the inclusion of ALC as a treatment of choice for symptomatic cholelithiasis that minimizes overnight stays and hospitalizations.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Planells Roig M, et al. Colecistectomía laparoscópica ambulatoria. Estudio de cohortes de 1.600 casos consecutivos. Cir Esp. 2013;91:156–62.