Medicines delivered directly to systemic circulation have saved many lives from life-threatening conditions, but also can impart undesirable effects.
Materials and methodsA prospective observational study was performed for 10 months in the tertiary care hospital to identify and evaluate cannula induced phlebitis in our study population. The data collection form retrieved demographic details, diseases and cannulation particulars of each patient. Moreover, a patient feedback questionnaire (Cronbach's alpha=0.70) retrieved their concerns toward cannulation.
ResultsPhlebitis was identified in 96 patients out of 146 subjects enrolled in the study; 52% had the first sign of phlebitis. Female patients were more prone, and the complication occurred irrespective of age (p>0.05). On the other hand, those on IV cefoperazone-sulbactam (n=13, 13.5%) followed by amoxicillin clavulanic acid (n=6, 6%) had significant cannulation complication (p<0.01). The cannula indwells time (p=0.001) and vein assessment (p=0.001) were statistically associated with incidence of phlebitis. Half of our samples had pain lasting about five minutes (χ2=9.2, p<0.05). Nevertheless, limited patients (n = 35, 36.5%) were prescribed topical Heparin Benzyl Nitrate, and none preferred to self-medicate nor opted for other home remedies.
ConclusionsThe study depicted high prevalence of phlebitis factored in by poor vein assessment and increase in indwelling time. We recommend proper awareness with on-site skill improvement program for health professionals on administration techniques and monitoring principles in order to lower cannulation related complications.
Los medicamentos suministrados directamente a la circulación sistémica han salvado muchas vidas en situaciones potencialmente mortales, sin embargo, pueden ocasionar también efectos no deseados.
Materiales y métodosSe realizó un estudio observacional prospectivo durante 10 meses en el hospital de atención terciaria, para identificar y evaluar la incidencia de flebitis relacionada con una cánula específica. Los datos recopilados incluyeron características demográficas, enfermedades y detalles sobre canulación de cada paciente. Además, un sistema de retroinformación del paciente (alfa de Cronbach=0,70) preguntó sobre la preocupación de las muestras sobre la canulación.
ResultadosSe identificó flebitis en 96 pacientes de entre 146 sujetos incluidos en el estudio, de los cuales, el 52% tuvo un primer signo de flebitis. Las mujeres reflejaron mayor propensión y las complicaciones se produjeron con independencia de la edad (p>0,05). Por otro lado, los sujetos tratados con cefoperazona-sulbactam i.v. (n=13, 13,5%) seguidos de los pacientes tratados con amoxicilina-ácido clavulánico (n=6, 6%) tuvieron una complicación de canulación significativa (p<0,01). El tiempo de permanencia de la cánula (p=0,001) y la valoración de la vena (p=0,001) estuvieron estadísticamente asociados a la incidencia de flebitis. La mitad de nuestras muestras tuvo dolor, que duró unos cinco minutos (χ2= 9,2, p<0,05). Sin embargo, a pocos pacientes (n=35, 36,5%) se les prescribió nitrato bencílico de heparina tópico, y ninguno de ellos optó por automedicaciones, u otros remedios.
ConclusionesEl estudio mostró una alta prevalencia de flebitis, determinada por la mala valoración de la vena y el incremento del tiempo de permanencia. Recomendamos una concienciación adecuada, con un programa para profesionales sanitarios que mejore la técnica in situ sobre técnicas de administración y principios de monitoreo, a fin de reducir las complicaciones relacionadas con la canulación.
Intravenous formulations are the inevitable forms of drug class that serves to treat various disease conditions. Dehydration, surgeries, severe infections, and complications of major diseases gain advantage of such agents. The straight, distal, and non-branching vein is the most preferred site for cannulation ensuring instant high drug bioavailability to impart the desired effect.1,2 The medical professionals should ensure the patient is on the required dose supplied in a standard rate and frequency.3 Their risk-benefit ratios are estimated, and is corresponded to the patient's requisite. In the pandemic era, steroid therapy is widely enrooted intravenously to impede cytokine storm for tackling the multi-organ dysfunctions; meanwhile, it can also induce hyperglycemia and diabetes mellitus.4 In these circumstances, the focus should be on preventing the disease related complications and minor ailment happening because of the drug can be easily managed later.5,6
The cannulation can generate vascular and extravascular complications.7 One of the other common adverse event encountered with IV administration is phlebitis.8 Painful irritation of the vein, tenderness on palpitation, erythema, warmth, swelling, induration, or palpable cord (thrombosis) of the cannulated vein would interrupt the ongoing therapy. When a patient experiences two or more of the above-mentioned signs and symptoms, it is said to be a case of phlebitis.9 Apart from that, infiltration, the incidence of occlusion and catheter dislodgement can also happen.10 These problems should be in a medical professional's mind while treating a patient. Meanwhile, patient's satisfaction is always the prime concern for bring out success to a treatment, and it can be enhanced by considering their opinion and addressing their physical and psychological problems. Alloubani et al., in their study, recommended inspecting the inserted cannula after a minimum of 12h.11 This would preserve the patients entrust on the gained treatment. Accordingly, we assessed the incidences of cannulation complications in the hospital and the patient's perspective on the experienced adverse event during the IV administration.
Materials and methodologyA prospective observational study was conducted for 10 months in a tertiary care referral hospital at Perinthalmanna, Malappuram district, Kerala, to investigate the incidence of phlebitis among in-patients. The Institutional Ethics Committee approval and official consent to carry out the research in the hospital was granted as per the letter No. IEC/KAS/2015/7. Moreover, the study adhered to the World Medical Association Declaration of Helsinki, 2013.
Inclusion and exclusion criteriaWe recruited both male and female patients with age ≥18 years admitted to neurology, nephrology, cardiology, and general medicine departments. While, psychiatric patients and those with pre-existing skin rashes, laceration and trauma at the insertion site were excluded.
Study toolsPharmacist's documentation form was designed to collect demographic details, co-morbidities, reasons for admission, diagnosis, past medical history and recommended therapy for the study population. Cannula-related characteristics such as its size, administration site, indwell time, vein assessment concerning each sample was also retrieved. Moreover, a self-prepared patient feedback questionnaire formulated in local language gave us their concerns on cannulation. Its nineteen questions evaluated their health status, indwelling pain, and other symptoms related to IV administration and previous history of cannulation complications. The Cronbach's alpha coefficient depicted the feedback questionnaire to have good internal consistency, and the confirmatory factor analysis is presented in Table 1.
Confirmatory factor analysis and internal consistency of the questionnaire (patient's feedback tool).
| 0 | Items | Factor loadings | Ranks | Cronbach's alpha co-efficient |
|---|---|---|---|---|
| Health | What is your current health condition? | 4.310 | 1 | 0.701 |
| Can you convey the span of pain? | 1.478 | 2 | ||
| Do you have any pain when the cannula is in use? | 1.042 | 3 | ||
| Occurrence | If you feel pain, how many times? | 0.983 | 4 | |
| Do you experience any difficulties rather than pain? | 0.834 | 5 | ||
| Where you been cannulated before | 0.562 | 6 | ||
| Strategies | When was the cannula previously inserted? | 0.305 | 7 | |
| Did you feel any difficulties as that of before when currently cannulated? | 0.258 | 8 | ||
| Did you discuss the problem with the physician? | 0.128 | 9 | ||
| Did the doctor prescribed any medicine for the difficulties? | 0.100 | 10 |
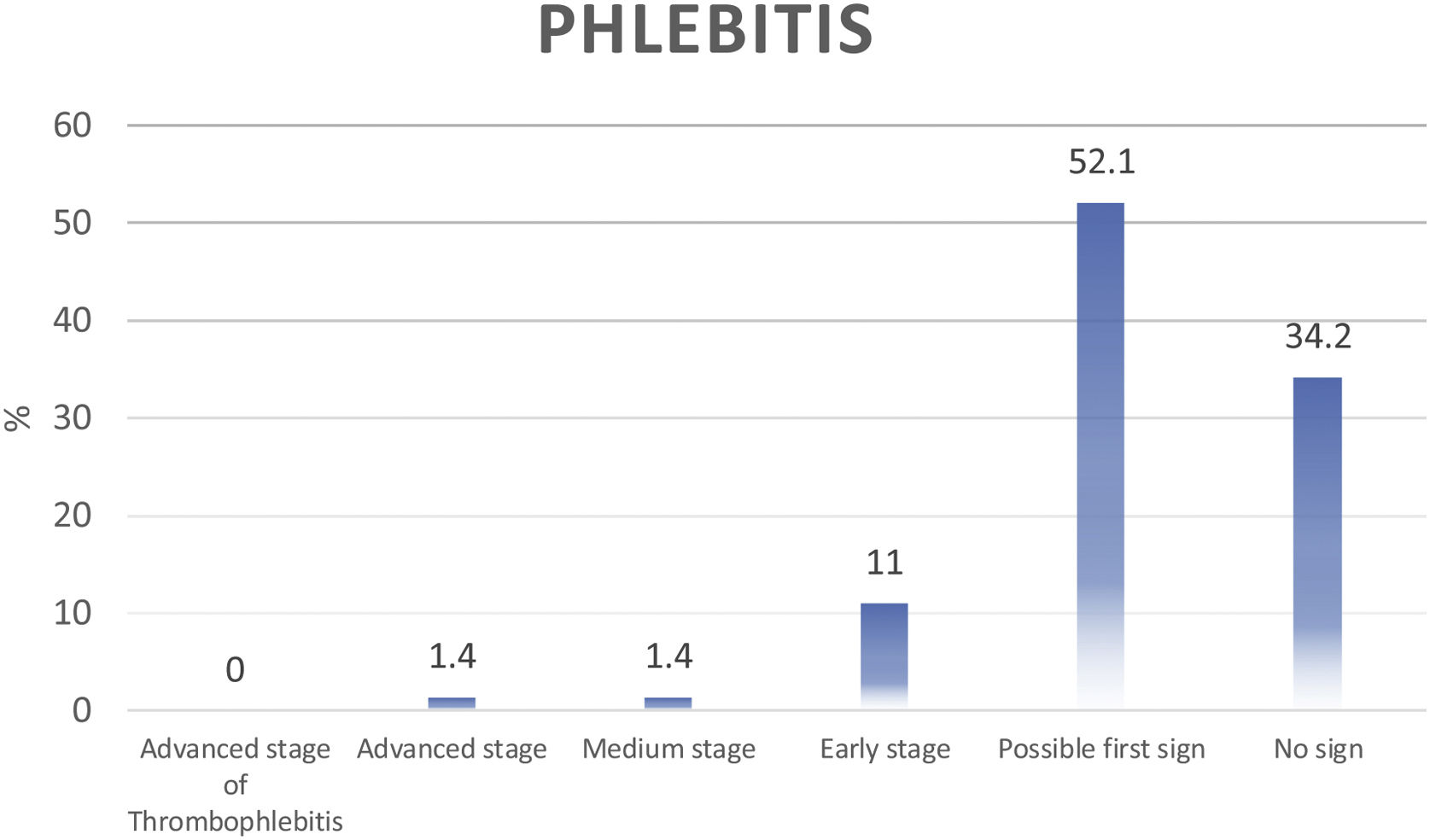
We have utilized the visual infusion phlebitis (VIP) score to analyze the incidence of phlebitis. The VIP scale of the infusion therapy standards (3rd Edition) is an internationally adopted tool observed in literature and preferred in clinical settings, worldwide.12 The readings in the scale can be zero (no sign), one (possible first signs of phlebitis), two (early stage of phlebitis), three (medium stage of phlebitis), four (advance stage of phlebitis) and five (advanced stage of thrombophlebitis).
Study procedureThe purpose and workflow of the study was explained to each patient, and written informed consent was documented. The medical case file and patient interview served as the prime sources of information. Further, clarifications were sought from physicians and nurses. The pharmacist collected all the data relevant to the study, and each patient's VIP scale score was calculated. According to the hospital policy, a cannula inserted into a patient should be replaced after three days regardless of any adverse events. The nurse has to document the reason and time of its removal. We ensured all the patients were closely followed up until they were discharged from the hospital.
OutcomesThe primary outcome was measured by the incidence of phlebitis in the hospital during the study period. While, the patients’ concern and practice following phlebitis served for the secondary outcome of this research.
Sample size calculationThe sample size (N) was determined with the equation of estimation of prevalence and it is presented below:
Zα/2=normal deviate for two tailed hypothesis=1.96, p=proportion from previous studies=44%, D=design effect=1, E=margin of error=10% and hence, the desired sample size was 95. However, we were able to collect a data set of 146 samples because of the prospective study design.
Statistical analysisThe statistical analysis was carried out using a statistical package for social sciences (SPSS) software version 20.0 (IBM SPSS, Chicago, IL, USA). The chi-square test was computed to find the association between categorical dependent variables concerning various groups, and p<0.05 portrayed the observations to be statistically significant.
ResultsThe study had more male (n=79, 54%) samples and non-medical professionals (n=145, 99%). The majority were identified to be having greater than 60 years of age (n=98, 67%). Predominant patients stayed in the hospital for 5–9 days (n=56, 38%), and few (n=8, 20%) were retained for more than 14 days. Moreover, those in the general medicine discipline (41.8%) were plentiful than those in neurology (37%), cardiology (12%), and nephrology (9%). There was an equal frequency of patients (n=46, 31.5%) with and without co-morbidities. The hospital utilized cannulas with 16(G), 18(G), 20(G), and 22(G) gauge sizes. Among them, 20(G) with pink color code was the most preferred (n=94, 64%) device. The dominated intravenous administration site was the Metacarpal vein (n=91, 62.3%) of the hand and the least supplies were in the upper arm (n=5, 3.4%).
The study put forward 65.8% (n=96) of phlebitis during the study period. The participants’ VIP score is represented in Fig. 1 that depicted 52% of our samples had first sign of phlebitis (VIP score=1) followed by those without any signs (VIP score=0, 34%). Few patients (n=16, 11%) experienced its early symptoms (stages) that constituted pain and swelling (n=9, 55%), erythema and swelling (n=5, 35%) and pain and erythema (n=2, 10%). There were limited medium and advanced stage of phlebitis (n=4) and none had severe thrombophlebitis (VIP score 5). On further analysis, the prevalence of phlebitis was more profound in female patients (n=66, 45%) than in males (n=80). The chi-square test (χ2=7.73) stated that there were differences in occurrence of phlebitis based on gender (p<0.05). The socio-demographic features and cannulation-related information are presented in Table 2.
The socio-demographic features and cannulation related information of the samples in the study.
| Particulars | Frequency | % |
|---|---|---|
| Gender | ||
| Male | 79 | 54.1 |
| Female | 67 | 45.9 |
| Age | ||
| 15–40 | 15 | 10.3 |
| 40–60 | 33 | 22.6 |
| >60 | 98 | 67.1 |
| Occupation | ||
| Medical | 1 | 0.7 |
| Non-medical | 145 | 99.3 |
| Incidence of phlebitis | ||
| Yes | 96 | 65.8 |
| No | 50 | 34.2 |
| Length of hospital stay (days) | ||
| <5 | 53 | 36.4 |
| 5–9 | 56 | 38.4 |
| 10–14 | 29 | 19.9 |
| >14 | 8 | 5.5 |
| Number of co-morbidities | ||
| 0 | 46 | 31.5 |
| 1 | 46 | 31.5 |
| 2 | 41 | 28.1 |
| 3 | 13 | 8.9 |
| IV cannula guage (G) utilized | ||
| 16 | 1 | 0.7 |
| 18 | 16 | 11.0 |
| 20 | 94 | 64.4 |
| 22 | 35 | 24.0 |
| Administration site | ||
| Upper arm | 5 | 3.4 |
| Cubital fossa | 16 | 11.0 |
| Forearm | 9 | 6.2 |
| Wrist | 15 | 10.3 |
| Radial vein | 10 | 6.8 |
| Metacarpal vein | 91 | 62.3 |
| Antibiotics (IV) administered | ||
| Present | 58 | 39.7 |
| Absent | 88 | 60.3 |
| Other medicines administered | ||
| Present | 14 | 9.4 |
| Absent | 132 | 90.4 |
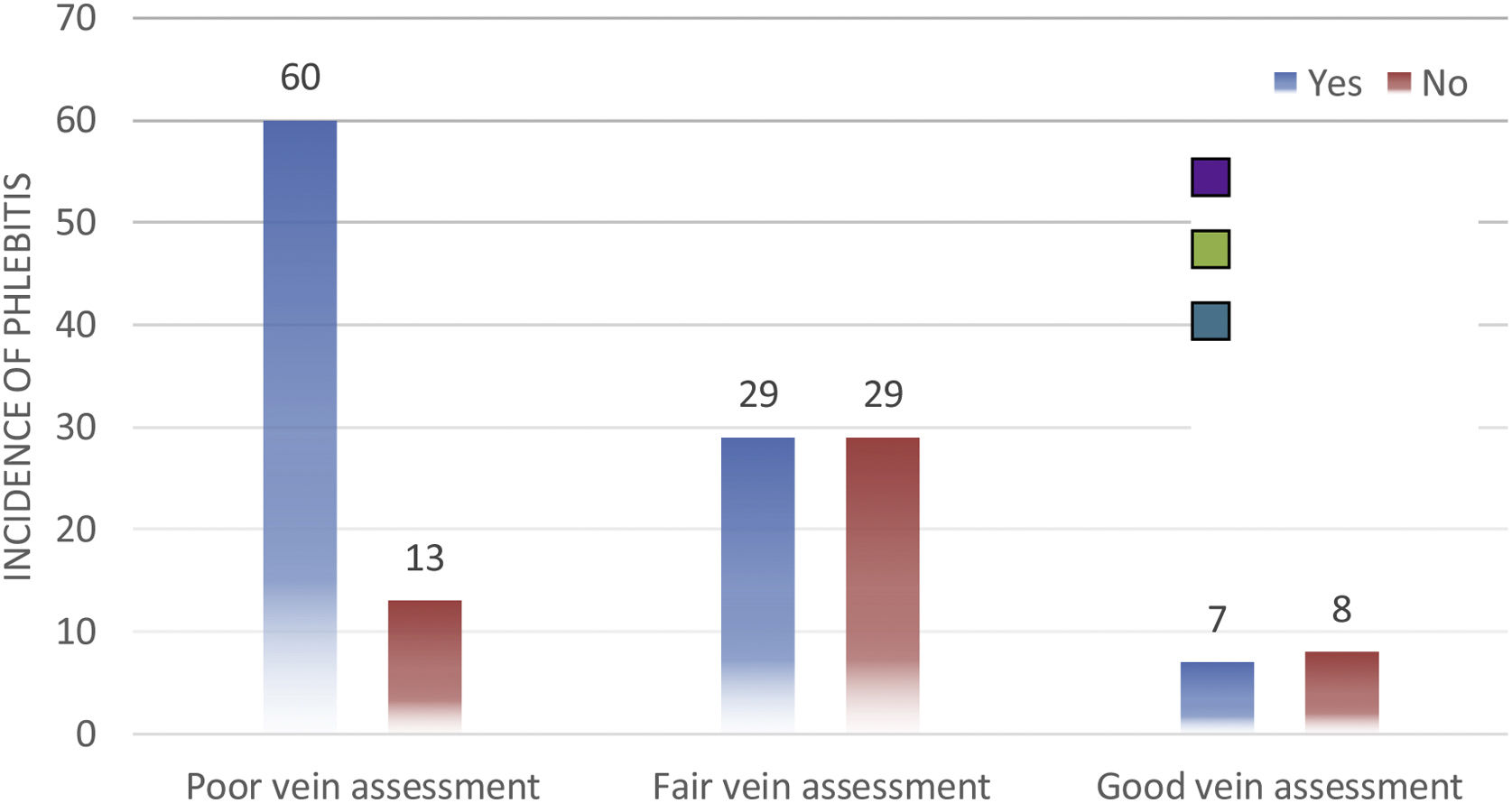
We identified 50% (n=73) patients with poor vein assessment followed by those with good (n=58, 40%) and fair (n=15, 10%) vein assessment during cannulation. The occurrences of phlebitis were reported prominently in those with (n=60) poor vein assessment (Fig. 2). This observation was statistically significant at p<0.001 (χ2=15.58).
Patients with good health status admitted in the hospital were lesser invaded by any cannula-induced complications (p<0.01). Nevertheless, phlebitis was insignificant and observed to be the same among those patients with varying lengths of hospital stay and IV cannula gauge size (p>0.05). But the cannula indwelling time did influence phlebitis (χ2=27.72, p<0.01), and patients with 3 days of cannula indwell had greater occurrences.
Even though patients with co-morbidities experienced cannulation complications, there was no significant difference among those with hypertension, kidney diseases, diabetes mellitus, cardiac disease, and stroke. However, there were cases of phlebitis in patients without any infection and not on antibiotics (p<0.05). Despite that, few of our samples on IV cefoperazone sulbactam (n=13, 13.5%) followed by amoxicillin clavulanic acid (n=6, 6%) had cannulation complication (χ2=32.47, p<0.01). In contrast, moxifloxacin, ciprofloxacin, fozidine, levofloxacin did not induce phlebitis (Table 3). Other intravenous drugs administered to the patient did not statistically lead to cannulation complication (p>0.05).
The incidences of phlebitis among patients concerning co-morbidities, antibiotics administered and cannula indwelling period.
| Particulars | Incidence of phlebitis | Chi square/likelihood ratio# | p value | |||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Frequency | % | Frequency | % | |||
| Hypertension | ||||||
| Present | 51 | 53.1 | 27 | 54 | 0.010 | 0.920 |
| Absent | 45 | 46.9 | 23 | 46 | ||
| Kidney disease | ||||||
| Present | 7 | 7.3 | 6 | 12 | 0.864# | 0.353 |
| Absent | 89 | 92.7 | 44 | 88 | ||
| Diabetes mellitus | ||||||
| Present | 34 | 35.4 | 24 | 48 | 2.174 | 0.140 |
| Absent | 62 | 64.6 | 26 | 52 | ||
| Cardiac disease | ||||||
| Present | 13 | 13.5 | 13 | 26 | 3.486 | 0.062 |
| Absent | 83 | 86.5 | 37 | 74 | ||
| Stroke | ||||||
| Present | 16 | 16.7 | 8 | 16 | 0.011 | 0.918 |
| Absent | 80 | 83.3 | 42 | 84 | ||
| Infections | ||||||
| Bedsore | 1 | 1.0 | 0 | 0 | 14.042# | 0.007* |
| Respiratory | 4 | 4.2 | 10 | 20 | ||
| Urinary tract | 8 | 8.3 | 8 | 16 | ||
| Wound | 2 | 2.1 | 0 | 0 | ||
| Absent | 81 | 84.4 | 32 | 64 | ||
| Name of IV antibiotics | ||||||
| Amoxicillin | 2 | 2.1 | 0 | 0 | 32.468 | 0.002* |
| Amoxicillin+clavulanic acid | 5 | 5.2 | 0 | 0 | ||
| Azithromycin | 1 | 1.0 | 0 | 0 | ||
| Cefoperazone+sulbactam | 13 | 13.5 | 7 | 14 | ||
| Cefoperazone+sulbactam, moxifloxacin | 0 | 0.0 | 3 | 6 | ||
| Cefuroxime | 3 | 3.1 | 0 | 0 | ||
| Ciprofloxacin | 0 | 0.0 | 1 | 2 | ||
| Fozidine | 0 | 0.0 | 2 | 4 | ||
| Levofloxacin | 0 | 0.0 | 2 | 4 | ||
| Meropenem | 3 | 3.1 | 0 | 0 | ||
| Metronidazole | 1 | 1.0 | 0 | 0 | ||
| Moxifloxacin | 6 | 6.3 | 1 | 2 | ||
| Nil | 61 | 63.5 | 32 | 64 | ||
| Ofloxacin | 1 | 1.0 | 2 | 4 | ||
| Cannula indwell time (days) | ||||||
| <2 | 36 | 37.7 | 0 | 0 | 27.72 | 0.001 |
| 3 | 57 | 59.4 | 50 | 100 | ||
| 4 | 3 | 3.1 | 0 | 0 | ||
In our study, more patients (n=46, 48%) with phlebitis had pain lasting about 5min. The observation was statistically significant at p<0.05 (χ2=9.2). Moreover, we observed 53.7% (n=77) of our samples to be devoid of any history of cannulation that was followed by those on IV line before 6 months (n=30, 20.5%), more than before 6 months (n=27, 18.5%), and before 1 month (n=12, 8.2%).
Thirty percent (n=29) patients complained of cannula-induced difficulty in their previous hospitalization, and among them, 63.5% (n=61) had re-occurrence (χ2=9.2, p<0.01). Our study portrayed limited patients (n=35, 36.5%) prescribed with topical heparin benzyl nitrate for phlebitis, and none preferred to self-medicate nor opted for home remedies. Moreover, we noticed that the cannulation complication did not affect their underlying disease condition (Table 4).
The patient's experiences and complaints confined to phlebitis in our study.
| Particulars | Incidence of phlebitis | Chi square value | p value | |||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| n | % | n | % | |||
| Health condition | ||||||
| Good | 6 | 6.3 | 7 | 14 | 11.965 | 0.003* |
| Average | 53 | 55.2 | 37 | 74 | ||
| Bad | 37 | 38.5 | 6 | 12 | ||
| Did you used cannulae here before | ||||||
| Yes | 61 | 63.5 | 8 | 16 | 27.936 | <0.001* |
| No | 35 | 36.5 | 42 | 84 | ||
| Does you felt such difficulties, when you used cannula before | ||||||
| Yes | 29 | 30.2 | 0 | 0 | 18.848 | <0.001* |
| No | 67 | 69.8 | 50 | 100 | ||
| Can you say the span of pain (min) | ||||||
| 1 | 3 | 3.1 | 1 | 2 | 9.202 | 0.027* |
| 2 | 31 | 32.3 | 21 | 42 | ||
| 5 | 46 | 47.9 | 27 | 54 | ||
| >5 | 16 | 16.7 | 1 | 2 | ||
| If prescribed which are the medicines | ||||||
| Heparin and benzyl nitrate | 35 | 36.5 | 0 | 0 | 23.977 | <0.001* |
| No treatment | 61 | 63.5 | 50 | 100 | ||
| Any pain when cannula is in use | Likelihood ratio | p value | ||||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| n | % | n | % | |||
| Difficulties because of cannulation | ||||||
| Block | 1 | 0.7 | 0 | 0 | 150.863 | <0.001* |
| Erythema | 8 | 5.8 | 0 | 0 | ||
| Itching | 21 | 15.2 | 0 | 0 | ||
| Exudation | 5 | 3.6 | 0 | 0 | ||
| Mild redness | 3 | 2.2 | 0 | 0 | ||
| Nil | 16 | 11.6 | 53 | 100 | ||
| Pain | 1 | 0.7 | 0 | 0 | ||
| Redness | 32 | 23.2 | 0 | 0 | ||
| Swelling | 49 | 35.5 | 0 | 0 | ||
| Yes, but could not explain | 2 | 1.4 | 0 | 0 | ||
A wide range of iatrogenic complications ranging from phlebitis to sepsis and later to morbidities and mortality had dragged patients to financial crisis. Phlebitis is a preventable and most common complication of intravenous administration, and we observed such events in our study.
Initially, we sorted out 96 patients (66%) with cannula-induced phlebitis. Katarina et al. stated in their cross-sectional study that the highest phlebitis cases were reported through severity rating system and scoring system.9 This could have resulted in greater identification of events in our study than that those claimed (30.7%) by Lv et al.’s meta-analysis of 35 studies.13 On the other hand, most of the patients affected with phlebitis were in the age group above 60 years (67.1%). The vein of the geriatric population has weak muscles surrounding the blood vessels causing them to roll when vein puncture is attempted. Reduction in vein stability while introducing the needle into the blood stream would create difficulty in the older compared to younger patients. Thus, special care should be initiated for the geriatric population.14,15 But, because the observation was statistically insignificant, we can state that phlebitis can occur irrespective of age. Additionally, female patients were the primary victims of phlebitis; however, some studies claimed the males suffered more.16,17 Hence, we can state that both genders can dominate in its occurrences depending on the study site and population. Moreover, phlebitis was higher in patients with five to nine days of hospital stay. Expanded hospitalization means longer indwell time or multiple cannulations, which would potentiate the risk. Braga et al. considered the length of hospital stay, a factor for cannulation complication.18
The present study reveals that the most frequently opted cannula gauge was 20G and the preferred site was the hand's metacarpal vein. Urbanetto et al. observed no significant association between cannula insertion site and phlebitis. Moreover, the forearm puncture was considered by most nurses due to the thickness of the vein.19 Easy viability of the injection sites and enhanced patient compliance directed them to opt for the site. We are aware that the recommended indwelling time according to the National Health Surveillance Agency (ANVISA) and the Royal College of Nursing is 72h. However, some studies preferred shorter indwell time, i.e., <48h.20 This may be favorable as the prolongation of cannula in-site can influence the occurrence of phlebitis.21 Moreover, we noticed the pain persist for 5min in majority of our patients, which might have been generated due to poor vein assessment. The observation of phlebitis and vein assessment was statistically significant.
The first sign of phlebitis was predominant in other investigations, so as ours.22 Swelling (35%), redness (23%), and itching (15%) was the prominent complaints raised by our patients. Atay et al. found a statistical association between chronic diseases and incidence of phlebitis and they noticed the majority of such patients were not presented with cutaneous inflammation. But, our study had the observation with statistical insignificance in this perspective.
The healthcare providers are closely and frequently in contact with patients, among them, nurses serve as the prime identifier of phlebitis than physicians. On the other hand, it was noticed that those with average to bad health conditions during their hospital stay had greater incidences (p<0.01). Hence, nurse's adherence to monitoring requisite can reduce phlebitis and thereby elevate patient satisfaction, depicted by a questionnaire-based survey of Osti et al.23 Enquiring on the previous cannulation complication is mandatory because we noticed 30% of patients with the event had history of phlebitis. In the Indian settings, the majority of the staff are new with contractual appointees, and they are not experts in cannulation skills.24 A proper training with onsite skill development and establishing a standard protocol on IV cannulation can alleviate any complication associated with improver administration.25,26 This was supported by a quasi-experimental study on nurses’ alertness that stated enhanced professional quality diminished the fatal events of cannulation.27 On the other hand, there are other factors contributing to the decline in patient care. A review by Kooli has picturized the authorities’ negligence in allocating the desired facilities and medical professionals in a health setting. This has to be changed, as the scenario will get worsened when a health crisis is born and the workforce cannot meet the requirement directing to infelicitous treatment outcomes. Such circumstances can also lower the people's trust in the healthcare discipline.28
A case report published by Obteene and Andrew observed an atopic vermiform ascending rash through the venous supply of antibiotic that was said to be phlebitis.29 In our study, IV cefoperazone and amoxicillin administration have complicated patients with cutaneous reactions. Additionally, Sheikhi et al. also reported greater incidence of phlebitis among antibiotic-treated individuals.30 Such patients can be recommended with suitable agents that can suppress their pain and inflammation. Jaimin et al. underwent a prospective study with topical solution 1000IU/ml heparin sodium wherein the every 8h application reduced the first signs of phlebitis when compared to the non-treated group (p<0.5).31 In our study, those with phlebitis (36.5%) were recommended with topical Heparin Nitrate, but larger samples were devoid of the treatment. Some studies quote the advantage of natural oils being effective in preventing phlebitis32; however, our patients did not opt for any home remedies nor prefer to self-medicate, when they have encountered a cannula induced vascular inflammation.
Improper cannula insertion and inadequate monitoring can develop phlebitis. Prior to insertion, the attending should ensure a clear indication for its use. The date and time of insertion should be appropriately documented. The cannula site should be visually inspected and palpated for evidence and possible risk for phlebitis. The compromised cannula should be removed immediately and re-sited if still required. It is essential to have proper hand hygiene practices when handling cannula. Moreover, nurses, physicians and other healthcare providers should separately check the inserted cannula site for preventing further harm occurring to patients.
The study picturized greater incidence of phlebitis that was related to poor vein assessment and increase in indwelling time. Even though majority had first sign of phlebitis, the pain persisted for about five minutes. It was astonishing that limited patients were only recommended with topical Heparin creams. Thus, considering the prevalence of cannulation complication in our study, there should be periodical awareness program and patient feedback system to improvise the possible error and complications associated with intravenous supply.
Source of fundingNo fund from any source has been received.
Author contributionsConceptualization, T. Nikhila, Linu Mohan P.; methodology, Mohammed Salim K.T., T. Nikhila, Linu Mohan P., Aravind R.S.; formal analysis, Mohammed Salim K.T., T. Nikhila, Linu Mohan P., Aravind R.S.; data curation, Mohammed Salim K.T., T. Nikhila, Linu Mohan P., Aravind R.S.; writing—original draft preparation, Mohammed Salim K.T., T. Nikhila, Linu Mohan P., Aravind R.S.; writing—review and editing, Mohammed Salim K.T., T. Nikhila, Linu Mohan P., Aravind R.S.; supervision, Mohammed Salim K.T., T. Nikhila, Linu Mohan P., Aravind R.S.
Availability of data and materialsAuthors are ready to supply the data upon request.
Consent to participateInformed consent was obtained from all subjects involved in the study.
Institutional review board statementCertified by the Institutional Ethics Committee and approved the proposal of the study as per letter no: IEC/KAS/2015/7 dated on 17-11-15.
Competing interestsAuthors have none to declare.
We acknowledge the valuable comments and suggestions by Dr. Dilip C. during this project. The authors would like to thank the staff of the department of nephrology, general medicine, nephrology, and cardiology of KIMS Al Shifa Hospital and also to the Department of Pharmacy Practice, Al Shifa College of Pharmacy, for all the support provided in finalizing the research work.