Lesions of triangular fibrocartilage (TFC) are associated with distal radioulnar joint instability. Arthroscopic treatment of these lesions improves functional outcome of affected patients. The aim of the present work is to evaluate functional and occupational outcome of TCF repair using an arthroscopic knotless anchor device in patients with associated distal radius fracture.
Material and methodsAn observational, descriptive study was carried out between November 2011 and January 2014 including 21 patients with distal radius fracture and Palmer 1B lesions of TCF (Atzei class 2 and 3) that were treated by arthroscopic knotless anchor (PopLok® 2.8mm, ConMed, USA). Mean follow-up was 18 months. Functional (Mayo Wrist Score) and occupational outcome results were analyzed. Mean age of the group was 43.0±8.8 years, with 19% of the patients being female. There was an associated scapholunate lesion in 5 cases.
ResultsFunctional results reached a mean of 83.4±16.1 points on Mayo Wrist Score. Mean sick-leave time was 153.16±48.5 days. Complete occupational reintegration was reached in 89.5% of the cases. There were no postoperative complications.
ConclusionsArthroscopic knotless anchor repair of 1B TFC tears is a minimally invasive method of treatment that improves tension of fixation, avoiding subsequent loosening, in our experience, with few complications and good functional and occupational results.
Las lesiones del fibrocartílago triangular (FCT) están asociadas en muchas ocasiones con inestabilidad de la articulación radiocubital distal. El tratamiento artroscópico de estas lesiones mejora el pronóstico funcional de los pacientes afectados. El objetivo del presente trabajo es evaluar los resultados funcionales y laborales de la reparación artroscópica con anclaje óseo sin nudo de lesiones del FCT asociadas a fracturas de extremidad distal del radio.
Material y métodoEstudio observacional, descriptivo entre noviembre de 2011 y enero de 2014 de 21 pacientes con fractura de radio distal asociada a lesiones tipo IB de Palmer (clases 2 y 3 de Atzei) del FCT tratados mediante reparación artroscópica con anclaje óseo sin nudo (PopLok® 2,8mm, ConMed, EE. UU.). El tiempo medio de seguimiento fue de 18 meses. Analizamos los resultados funcionales (Mayo Wrist Score) y laborales. La edad media fue de 43,0±8,8 años, con un 19% de mujeres. Se hallaron 5 casos con lesión escafolunar asociada.
ResultadosLa media obtenida en la escala funcional de Mayo Wrist Score fue de 83,4±16,1 puntos. El tiempo de baja medio fue de 153,16±48,5 días. La recuperación laboral sin limitaciones fue posible en el 89,5% de los casos. No se recogieron complicaciones postoperatorias.
ConclusionesLa reparación artroscópica con anclaje óseo sin nudo de lesiones IB del FCT en pacientes con fractura de radio distal supone un método de tratamiento mínimamente invasivo, que mejora la tensión en la reparación y evita el posterior destensado, en nuestra experiencia, con baja tasa de complicaciones y buenos resultados funcionales y laborales.
Lesions of the triangular fibrocartilage (TFC) are often associated to instability of the distal radioulnar joint. Their prevalence is approximately 59%1 of distal radius fractures, regardless of the type of fracture, and in these cases, it represents a proven cause of worse functional result of the fracture. Arthroscopic treatment can obtain an improvement of the functional prognosis for these patients.
In these cases arthroscopy is not only the most reliable method to diagnose the lesions, but is also used for their treatment, allowing us to extend their classification, as done by Atzei.2
Arthroscopy in distal radius (DR) fractures can diagnose the lesions and differentiate whether they are peripheral lesions (Atzei type 1), which do not involve instability of the distal radioulnar joint (DRUJ), or foveal disinsertions (Atzei 2 and 3), which do involve it.
At present, surgical treatment of these lesions can be carried out through arthroscopic techniques. Improvements in the instrumentation used in this mode of treatment have been gradually introduced. The current option is knotless anchor systems, the object of our work (PopLok, ConMed®, USA).
The objective of our study was to provide a detailed clinical description of the functional results obtained in a series of patients suffering DR fracture, in whom a lesion of the peripheral TFC (Atzei type 2 and 3) associated to DRUJ instability was identified.
Material and methodsWe conducted an observational, descriptive study of patients suffering Palmer3 IB lesion of the TFC (Atzei 2 and 3), confirmed by arthroscopy and treated through knotless bone anchor with a PopLok system (ConMed®, USA). We included 21 patients suffering this pathology who were treated at our center between November 2011 and January 2014. This represented approximately 15.2% of the total DR fractures treated at our center in this period.
The mean postoperative follow-up period was 18 months (with a minimum of 2 months and a maximum of 27 months). The mean age was 43.0±8.8 years, with a gender distribution of 17 males and 4 females. We analyzed 11 right wrists and 10 left, of which 57.1% corresponded to the dominant limb and 42.9% to the non-dominant. We found 1 case of combined Palmer IB and IA lesion, which was included in the study, as well as 5 cases suffering an associated ulnar lesion and 3 cases with affected DRUJ.
Out of the 21 patients included in the study, 52.4% presented a type III fracture of the distal radius according to the classification by Fernández.4 All the patients with DR fracture were treated by orthopedic reduction and initial immobilization and posterior reconstruction using a plate osteosynthesis through a volar route; in 57.1% of the cases it was with a DVR® plate (Johnson & Johnson) and in 19% with a RIM® volar plate (Synthes).
The period that elapsed between the trauma and the intervention ranged between 2 and 24 days, with a median of 10 days (mean: 10.62±4.8 days).
The preoperative evaluation of patients consisted of a clinical examination conducted by an experienced surgeon, and at least 2 radiographic wrist projections (anteroposterior and lateral). The radiographic study allowed us to classify the DR fracture, as well as to rule out other lesions. We evaluated ulnar variance and radial tilt. We also obtained a computed tomography (CT) scan in those cases requiring an extension of the imaging study.
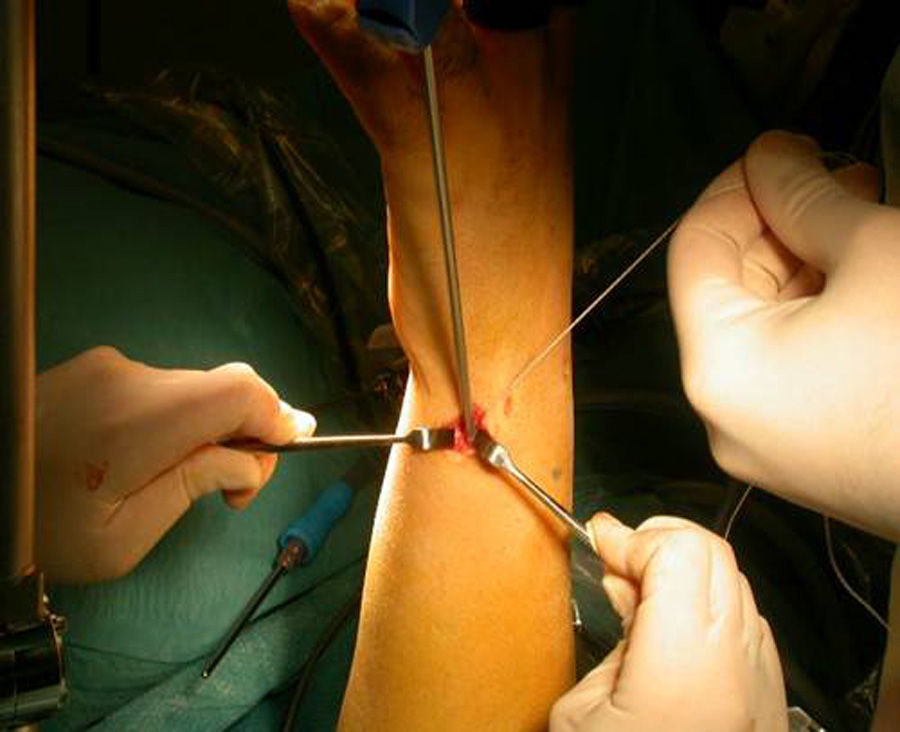
Surgical techniqueUnder general and regional anesthesia and applying ischemia we proceeded to carry out a volar approach to the DR fracture and synthesis with a screw plate. Following the osteosynthesis we carried out a clinical exploration of DRUJ stability, through volar and dorsal displacement of the radius with a stabilized ulna. All the patients in our series presented clinical DRUJ instability upon exploration, so our team considers this to be an essential criterion for indication of arthroscopy. Next, we performed a dry diagnostic and therapeutic arthroscopy using a wrist traction tower system (Acumed®, USA). The arthroscopy began with the identification of the 3–4 portal, through palpation of Lister's tubercle in the radius. We performed a skin incision and then deepened it bluntly until the radiocarpal joint was reached. We then introduced the lens and light source through it. Under direct visual control we identified the 6 R portal, in a radial position to the extensor carpi ulnaris, which allowed us to manipulate the ulnar joint surface. We then conducted a systematic visual evaluation of the radiocarpal ligamentous structures and joint surfaces in all patients. We verified the reduction of the DR fracture obtained with osteosynthesis and examined the TFC, as well as the scapholunate, radiocarpal and ulnocarpal ligaments. In this series we diagnosed 5 patients with scapholunate joint lesion during the arthroscopic evaluation, and treated it during the same surgical intervention through ligamentopexy, reinsertion or fixation with a percutaneous osteosynthesis, with no associated dorsal pathway in 95.2% of the cases. We continued the examination verifying the stability and resistance of the TFC.
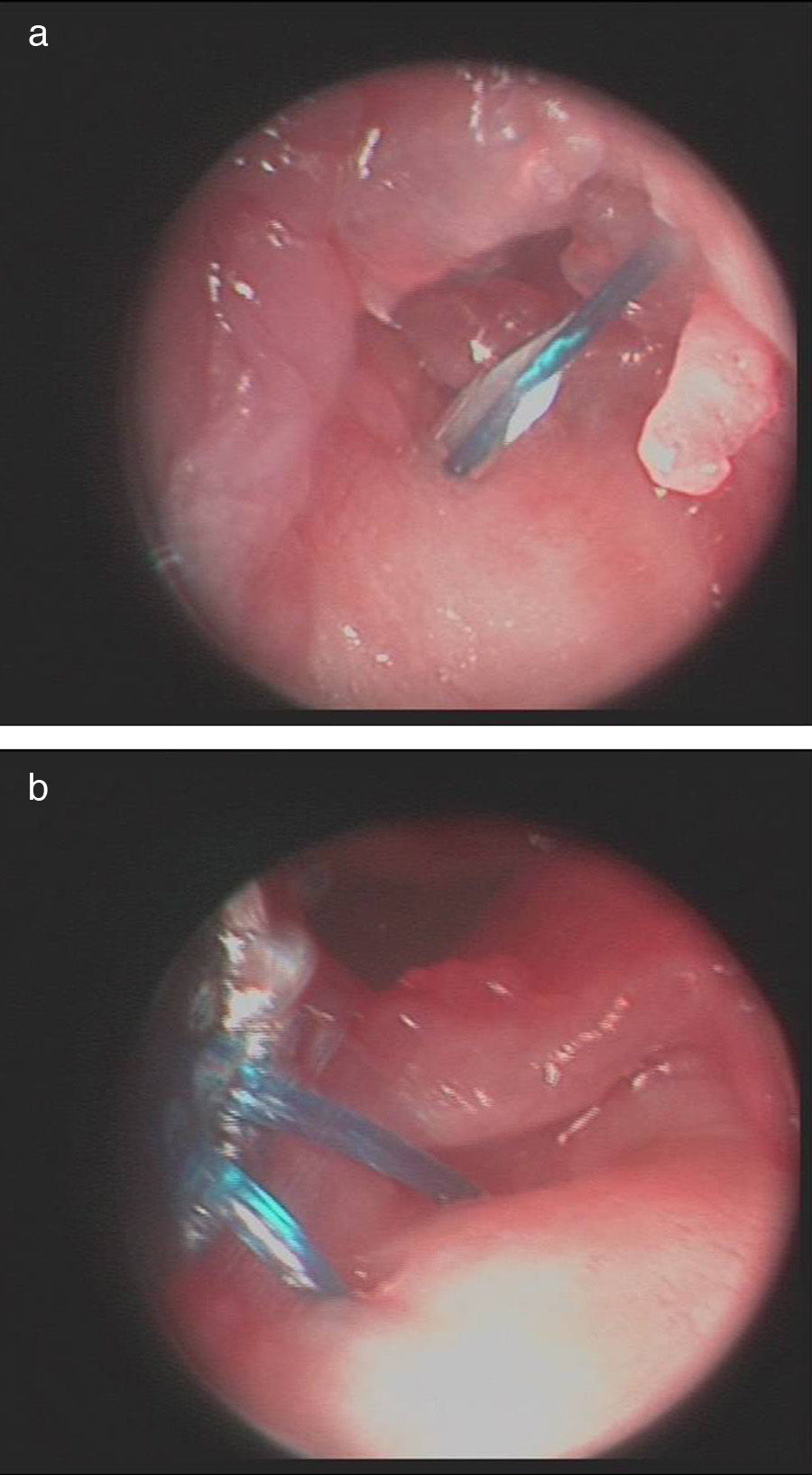
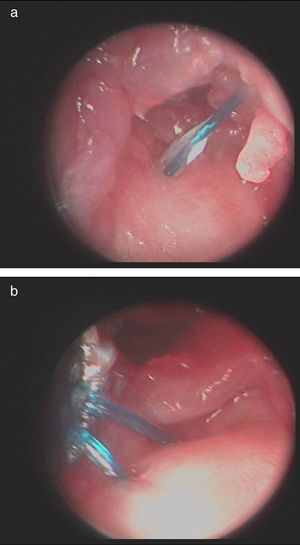
This was basically assessed through 2 tests: the “Trampoline test”, which evaluates tension and texture, and the “Hook test”, which evaluates foveal disinsertion. The TFC was affected in its ulnar side in all cases in this study.
Once the diagnosis and therapeutic indication had been established, we created an accessory portal to 6 R, between the anterior and posterior ulnar tendons (Fig. 1). We introduced the instrumentation through this portal and, under direct visual control, identified the point selected to reanchor the TFC in the ulnar fovea. This point was first marked with a guide needle, then drilled with the drill bit of the device, and then verified radiographically. We also used the same approach to pass a monofilament 3/0 thread by the TFC (Fig. 2a and b) following the outside-in technique (Fig. 3). This thread was subsequently replaced by the 0/0 thread of the anchor system. We loaded the 2.8mm PopLok implant (ConMed®, USA) (Fig. 4), placed in its foveal location and tensed without traction (Fig. 5) and verified the stability of the reanchor. We then proceeded to close the volar incision but left open the arthroscopy portals, covered with sterile gauzes. We placed a cushioned bandage in all patients with a forearm cast to fix it for 3 weeks or extend immobilization depending on the associated lesions present.
The time of immobilization varied between 2 and 24 days, with a mean value of 24.35±11 days. In cases suffering lesion of the scapholunate ligament the immobilization was maintained for a period of 6 weeks. The mean time at the start of active rehabilitation was of 29.85±11.35 days.
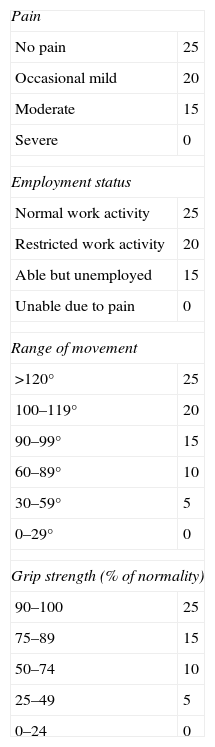
The postoperative evaluation was carried out through serial clinical examinations and radiographic controls. Upon discharge we evaluated the functional and work results, after a median period of 143.5 days. The objective evaluation of the functional results was carried out using the Mayo Wrist Score5 (Table 1), which examined residual pain, work status, range of motion and grip strength compared to the healthy contralateral wrist, to return a score between 0 and 100. The measurement of grip strength was carried out through isokinetic tests using a dynamometer. DRUJ instability was clinically assessed using the Moritomo classification.6 The duration of work leaves was defined as the period elapsed between the date of the trauma and the date of discharge. The work results were assessed based on the type of discharge, in terms of healing, improvement, partial or total disability. In total, in 6 of the patients included in the study we contemplated a variable level of disability due to other, unrelated lesions.
Modified Mayo scale.
| Pain | |
| No pain | 25 |
| Occasional mild | 20 |
| Moderate | 15 |
| Severe | 0 |
| Employment status | |
| Normal work activity | 25 |
| Restricted work activity | 20 |
| Able but unemployed | 15 |
| Unable due to pain | 0 |
| Range of movement | |
| >120° | 25 |
| 100–119° | 20 |
| 90–99° | 15 |
| 60–89° | 10 |
| 30–59° | 5 |
| 0–29° | 0 |
| Grip strength (% of normality) | |
| 90–100 | 25 |
| 75–89 | 15 |
| 50–74 | 10 |
| 25–49 | 5 |
| 0–24 | 0 |
Score: Excellent >90, good 75–89, average 60–74, poor <60.
The mean final functional result according to the Mayo Wrist Score was 83.42±16.16 points, with 84.2% excellent or very good results. In this group there were 89.5% discharges due to healing or improvement (17 patients), with a mean duration of medical leave of 153.16±48.53 days.
No long-term complications or recurrences were registered. A reintervention was required in 6 cases, all of them for removal of osteosynthesis material unrelated to the TFC repair.
DiscussionThe triangular fibrocartilage (CTF) complex is a ligamentous structure that stabilizes the ulnar side of the wrist, acting as an extension of the joint surface of the radius to support the first carpal row, and it also underpins the distal radioulnar joint. The TFC is damaged in up to 59% of DR fractures. In these cases, repair and treatment of the DRUJ instability provides an improvement of the clinical results.
TFC lesions are one of the main causes of ulnar pain in the wrist and instability of that joint. According to the classification established by Palmer,7 these can be classified into acute (traumatic) and chronic (degenerative), and in turn be subdivided according to their location and associated lesions, with significant prognostic implications. Type IB lesions involve traumatic avulsions in the periphery of the ulna which can be associated to a fracture of the styloid and, due to their scarring potential,8,9 are firm candidates for anatomical reanchoring.
Atzei3 established a more operative classification of peripheral TFC complex lesions, based on clinical, radiographic and arthroscopic findings, and proposed a treatment for each type of lesion. Types 2 and 3 in this classification would correspond to acute lesions (time under 3 months), of the peripheral portion of the proximal TFC, associated or not to fractures of the styloid, and corresponding to type IB in the Palmer classification.
The diagnosis of this complex pathology is mainly based on clinical suspicion, based on medical history and physical exploration. Wrist arthroscopy is considered as a reliable diagnostic test, which provides a direct and magnified visualization of all the structures,10 whilst also representing a minimally invasive therapeutic method.
Arthroscopic repairs of the TFC through various suture mechanisms and transosseous fixations have been described in recent years,11–13 along with the latest fully-arthroscopic techniques using knotless anchor systems.14–16 The latter make it possible to repair both the superficial and deep (ligamentum subcruetum) planes of the TFC, returning them to their anatomical insertion, and are biomechanically more resistant than capsular repairs17 and avoid irritation of the surrounding tissues by the knots. In addition, purely arthroscopic techniques preserve the extensor carpi ulnaris tendon and minimize the risk of damaging the dorsal sensory branch of the ulnar nerve.
Reinsertion can be carried out with simple and knotted bone anchors. From our point of view, except when knotless anchor systems are used, the difficulty lies in correctly adjusting the tension of the knot.
Geissler16 describes the knotless arthroscopic repair of peripheral ulnar avulsions of the TFC joint disk through the Fast-Fix anchor system (Arthrex®, USA), as does Yao,18 although without providing functional results.
In a multicenter study using the Whipple technique to repair the TFC, Coso et al.19 presented 41 patients out of a total of 45 with good or excellent results according to the Mayo Wrist Score. Also, Estrella et al.20 found 74% of good or excellent results according to the Mayo Wrist Score in their review of 35 patients treated with the Whipple or Tuohy techniques.
In a series of 12 patients, Yao18 presented 11 cases with excellent results according to the QuickDash questionnaire, with a return to work in 5 months, although there was an overall decrease in the strength and movement range of the wrist joint.
These results can be objectively compared with those obtained in our work and allow us to reaffirm the value of arthroscopy for the repair of peripheral TFC lesions, with good functional results, a minimum rate of complications and a rapid recovery. Nevertheless, there are currently no studies with level I scientific evidence that prove the benefits of wrist arthroscopy in this kind of pathology.
Our study presents several limitations since it is a retrospective study including different types of DR fracture, with associated scapholunate joint lesions and a relatively small number of patients. However, in spite of these limitations, the results of our study show that the arthroscopic repair of peripheral lesions of the TFC in case of DR fracture, using a PopLok knotless bone anchor system (Conmed®, USA), provides good functional results and in terms of return to work, with a low rate of complications, so we recommend the use of this technique in any candidate patient.
ConclusionsIn our experience, the arthroscopic repair with knotless bone anchors of peripheral ulnar lesions of the TFC associated to DR fracture represents a minimally invasive method of treatment, which improves tension during the repair, with a low rate of complications and good results.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García-Ruano ÁA, Najarro-Cid F, Jiménez-Martín A, Gómez de los Infantes-Troncoso JG, Sicre-González M. Resultados de la reparación artroscópica mediante anclaje óseo sin nudo de lesiones del fibrocartílago triangular asociadas a fractura de extremidad distal de radio. Rev Esp Cir Ortop Traumatol. 2015;59:260–265.