Surgical site infection (SSI) represents 30% of all causes of health care-associated infection (HAI) and is one of the most dreaded complications in surgical patients. We estimated the excess direct costs of SSI using a matched nested case–control study in acute-term care at Ramon y Cajal University Hospital in Spain.
Material and methodCases were patients who developed a first episode of SSI according to the criteria established by the CDC's National Healthcare Safety Network. Controls were matched to cases in 1:1 ratio taking into account the American Society of Anaesthesiologists score, age, sex, surgery date, and principal diagnosis.
ResultsThis study found that infection in hip replacement increased direct costs by 134%. Likewise, the excess cost due to the infections caused by methicillin resistant Staphylococcus aureus was 69% higher than the excess cost attributable to infections caused by other microorganisms.
ConclusionsSSI after hip replacement continues to be a costly complication from the hospital perspective. Costs due to SSI can be used to prioritise preventive interventions to monitor and control HAI.
La infección de localización quirúrgica (ILQ) representa el 30% de todas las causas de infecciones relacionadas con la atención sanitaria (IRAS), siendo una de las complicaciones más temidas en pacientes quirúrgicos. Se estimó el exceso de costes directos de la ILQ mediante un estudio de casos y controles emparejado y anidado en una cohorte, en un hospital de agudos en España (Hospital Universitario Ramón y Cajal).
Material y métodoLos casos fueron pacientes que desarrollaron un primer episodio de ILQ según los criterios establecidos por el National Healthcare Safety Network de los CDC. Los controles fueron emparejados a los casos en una razón de 1:1, teniendo en cuenta la clasificación de la American Society of Anesthesiologists, la edad, el sexo, la fecha de la cirugía y el diagnóstico principal.
ResultadosEste estudio encontró que la infección en reemplazo de cadera incrementó los costes directos en un 134%. Asimismo, el exceso de costes debido a la infección causada por Staphylococcus aureus resistente a la meticilina fue 69% mayor que el exceso de costes debido a las infecciones causadas por otros microorganismos.
ConclusionesLa ILQ después de reemplazo de cadera sigue siendo una complicación costosa desde la perspectiva del hospital. Los costes debidos a la ILQ pueden ser utilizados para priorizar intervenciones preventivas de vigilancia y control de las infecciones relacionadas con la atención sanitaria.
In Spain, hospital-acquired (HAI) or nosocomial infection is the second cause of adverse events attributable to hospitalisation, and surgical site infections (SSI) amount to 30% of all of the causes of HAI.1 SSI is one of the most worrying complications in surgical patients. Rates of infection vary widely, depending on the type of procedure analysed,2,3 and it affects 3.5% of hip arthroplasty patients in Spain.4 According to a recent revision, and depending on the type of surgical procedure, the average cost attributable to SSI ranges from 2342 US$ to 38,554 US$ per admission, while hospitalisation time is prolonged by from 6 to 14 days, on average.5 Alfonso et al.6 estimated that the cost of SSI was 10,232 US$ per patient in a Spanish hospital, of which 37% was due to the prolongation of hospitalisation. This study aims to quantify the excess direct costs due to surgical wound infection in hip arthroplasty, using cases with matched controls.
Material and methodsStudy context and designThis study was undertaken in Ramón y Cajal University Hospital, a public hospital in Madrid (Spain). It has 1090 working beds, receives approximately 34,000 admissions and performs 32,000 surgical operations per year. From 1 January 2005 to 31 December 2011 the patients admitted to the Traumatology and Orthopaedic Surgery Department for hip replacement, identified in the ninth revision of the International Disease Classification by codes: 00.70–00.73, 00.85–00.87, 81.51–81.53, were followed up prospectively by the nosocomial infection monitoring system Continuous clinical quality improvement indicators.
Sources of data and variablesThe nosocomial infection monitoring system Continuous clinical quality improvement indicators is composed of a work team in the preventative medicine department of the hospital, with at least one epidemiologist doctor and one or more nurses specialising in this area. They visit trauma units at least once every 2 days to gather data, from the day surgery takes place until patients are discharged, including any re-admission during the first year after implantation. The system has its own data-gathering format for this, linked to a program created for processing and analysis. Clinical histories were used as the source of information, together with information supplied directly by the doctors and nursing staff, the surgical report and the results of cultures and microbiological laboratory analyses.
Data was gathered on each patient regarding their age, sex, main diagnosis at admission, type of surgery (emergency vs planned), type of arthroplasty, American Society of Anaesthesiologists (ASA) classification, duration of the procedure, degree of surgical contamination, the suitability of pre-surgical antibiotic prophylaxis, the etiological agent, depth of infection, days of hospitalisation, costs and mortality. Antibiotic prophylaxis was considered to be suitable if the antimicrobial agent used was recommended in the hospital guides (cephazolin, amoxycillin/clavulanic acid or vancomycin in patients allergic to beta-lactam antibiotics) and when it lasted no longer than 24h after surgery, according to hospital infection committee protocols.
ParticipantsThe cases were those patients within the cohort who developed a SSI, defined according to the criteria proposed by the NHSN.7 Only the first episode of infection was considered eligible. Control cases were selected from among those patients in whom no SSI was detected during admission, and who were not re-admitted for any reason. They were matched 1:1 with each one of the cases, taking into account the factors that may influence the prolongation of hospitalisation and costs. Matching was ranked in the following order, and taking into account the fact that only the first selection criterion was obligatory: ASA classification, age ±5 years, sex, date of surgery ±2 weeks and main diagnosis at admission. The study excluded those patients for whom revision arthroplasty due to septic loosening was prescribed, given that this complication may mask a latent infection that had yet to become clinically evident. Selection of cases and controls was not restricted to survivors. If after selection more than one control was obtained for a case, one of them was selected at random.
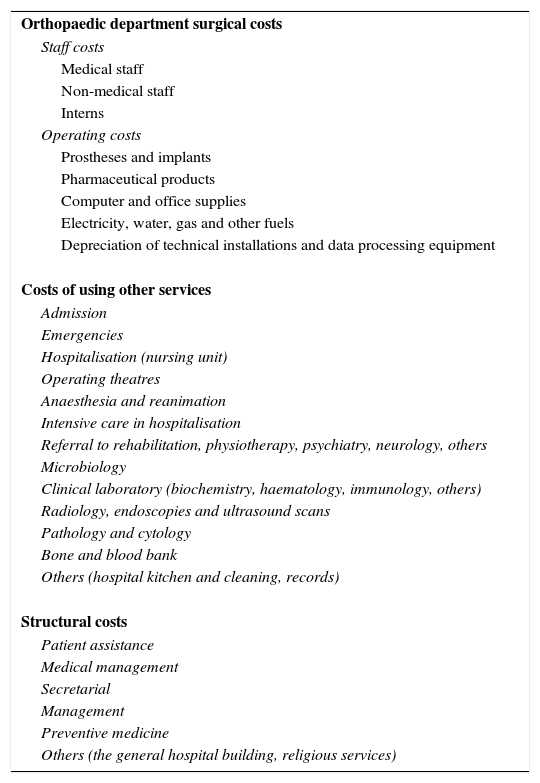
Costs and hospitalisationCosts were calculated from the point-of-view of the hospital. Direct costs were those generated by each patient during the time they were admitted, including re-admission due to infection. The resources considered covered the costs of the orthopaedic surgery department and the costs of using other hospital services and structural costs (Table 1). Costs were expressed in Euros (€) and corrected for inflation using the retail price index of the Spanish National Statistics Institute,8 taking into account the date of surgery of the last patient included. The excess cost attributable to SSI was calculated as the median of the differences for each case and control pair. Finally, the excess cost was converted into US$ using the purchasing power parity published by the Organisation for Economic Co-operation and Development for 2011.9 The source of information on costs was the hospital Analytic Accounting Unit. As was the case for excess costs, calculation of excess hospitalisation considered re-admission due to infection. It was obtained by calculating the median of the difference in stay between each pair of matched case and control. The measurements included total hospitalisation as well as postoperative hospitalisation attributable to SSI.
Direct costs structure, orthopaedic surgery hospitalisation.
| Orthopaedic department surgical costs |
| Staff costs |
| Medical staff |
| Non-medical staff |
| Interns |
| Operating costs |
| Prostheses and implants |
| Pharmaceutical products |
| Computer and office supplies |
| Electricity, water, gas and other fuels |
| Depreciation of technical installations and data processing equipment |
| Costs of using other services |
| Admission |
| Emergencies |
| Hospitalisation (nursing unit) |
| Operating theatres |
| Anaesthesia and reanimation |
| Intensive care in hospitalisation |
| Referral to rehabilitation, physiotherapy, psychiatry, neurology, others |
| Microbiology |
| Clinical laboratory (biochemistry, haematology, immunology, others) |
| Radiology, endoscopies and ultrasound scans |
| Pathology and cytology |
| Bone and blood bank |
| Others (hospital kitchen and cleaning, records) |
| Structural costs |
| Patient assistance |
| Medical management |
| Secretarial |
| Management |
| Preventive medicine |
| Others (the general hospital building, religious services) |
The variables were described by first classifying them as numerical or categorical. The median was calculated for the first type, together with the 25 and 75 percentiles (p25 and p75). Absolute frequencies and percentages were obtained for the categorical variables in each one of their categories. Cases and controls were compared by using the non-parametric Wilcoxon signed rank test for numerical variables, and by the Mantel–Haenszel test for paired data in the categorical variables. All statistical analysis was undertaken with a significance of 5% using the Stata statistical program, version 11.0.
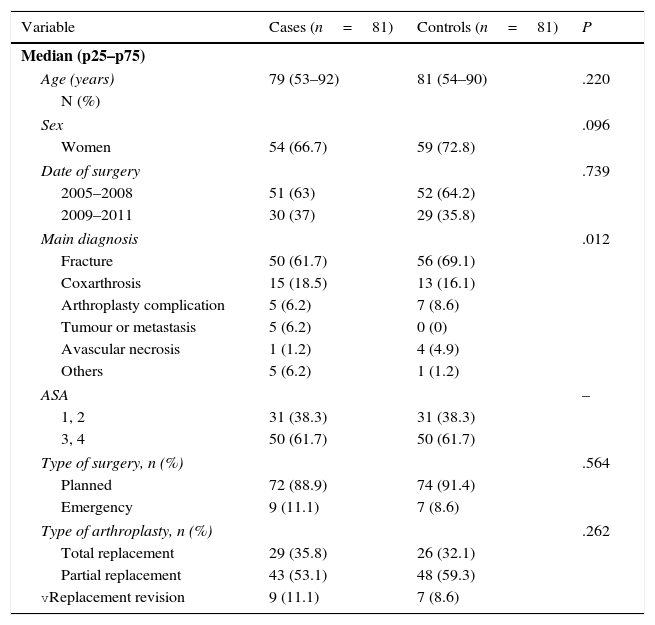
ResultsParticipantsFrom 1 January 2005 to 31 December 2011 86 SSI occurred in 85 (3.6%) of the 2378 patients operated for hip arthroplasty in our hospital. 2582 procedures were performed, with an infection rate of 3.3%. Four patients with infection were operated for septic loosening; 81 cases and 81 controls were therefore included in the analysis. The sociodemographic characteristics of the cases and controls are shown in Table 2. Hip fracture was the most frequent reason for joint replacement in both groups, while the most frequent type of implant was partial arthroplasty. 4.9% of cases and 3.7% of controls died during admission.
Sociodemographic variables and those used to match cases and controls.
| Variable | Cases (n=81) | Controls (n=81) | P |
|---|---|---|---|
| Median (p25–p75) | |||
| Age (years) | 79 (53–92) | 81 (54–90) | .220 |
| N (%) | |||
| Sex | .096 | ||
| Women | 54 (66.7) | 59 (72.8) | |
| Date of surgery | .739 | ||
| 2005–2008 | 51 (63) | 52 (64.2) | |
| 2009–2011 | 30 (37) | 29 (35.8) | |
| Main diagnosis | .012 | ||
| Fracture | 50 (61.7) | 56 (69.1) | |
| Coxarthrosis | 15 (18.5) | 13 (16.1) | |
| Arthroplasty complication | 5 (6.2) | 7 (8.6) | |
| Tumour or metastasis | 5 (6.2) | 0 (0) | |
| Avascular necrosis | 1 (1.2) | 4 (4.9) | |
| Others | 5 (6.2) | 1 (1.2) | |
| ASA | – | ||
| 1, 2 | 31 (38.3) | 31 (38.3) | |
| 3, 4 | 50 (61.7) | 50 (61.7) | |
| Type of surgery, n (%) | .564 | ||
| Planned | 72 (88.9) | 74 (91.4) | |
| Emergency | 9 (11.1) | 7 (8.6) | |
| Type of arthroplasty, n (%) | .262 | ||
| Total replacement | 29 (35.8) | 26 (32.1) | |
| Partial replacement | 43 (53.1) | 48 (59.3) | |
| vReplacement revision | 9 (11.1) | 7 (8.6) | |
Matching quality was 96.3% for age, 88.9% for sex and 80.3% for the main diagnosis at admission. ASA classification was the best-matched variable (100%), while matching for the date of surgery stands at 49.4%. The median of the differences between the dates of surgery of the cases and their controls was 15 days (p25–p75: 8–202 days).
Surgical characteristicsThe median duration of surgery was 105min (p25–p75: 80–150min) for the cases and 90min (p25–p75: 60–120min) for the controls. All of the operations were clean or clean-contaminated. Pre-surgical antibiotic prophylaxis was administered in 80 (97.4%) of the cases and in the same number of controls. Selection of the antibiotic and duration of the prophylaxis were suitable in 25% of the cases and controls. The main cause of unsuitable prophylaxis was its duration; in 75% of the groups it lasted for longer than 24h after the incision was closed.
Surgical site infectionThe median length of time that passed between surgery and the diagnosis of wound infection was 16 days (p25–p75: 13–27 days). Of the 81 cases 76 (93.8%) occurred in the first 90 days after implantation of the prosthesis. The most common location was organ-space infection, in 44.4% of cases, followed by superficial infection (32.1%) and deep infection (23.5%).
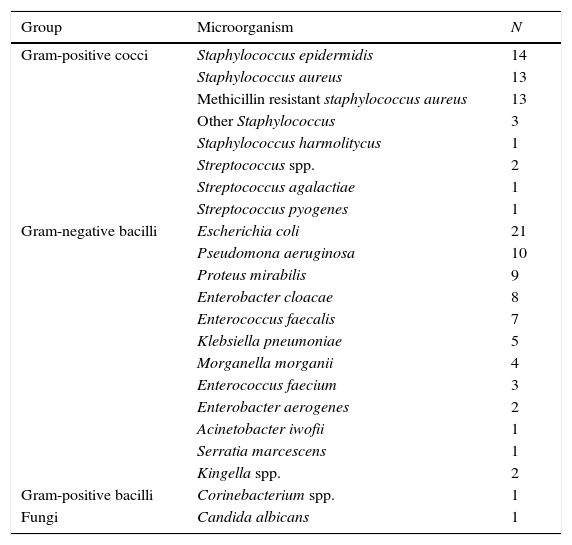
The aetiological agent was identified in 96.3% (78) of cases, and polymicrobial aetiology was the most common cause of infection (57.7%). Of the infections with a single aetiology (33), gram-positive cocci and gram-negative bacilli were the cause in 63.6% and 30.3%, respectively. Methicillin resistant Staphylococcus aureus (MRSA) was involved in 16.7% (13) of the positive cultures (Table 3).
Microorganisms identified in the 78 cases of SSI with positive cultures.
| Group | Microorganism | N |
|---|---|---|
| Gram-positive cocci | Staphylococcus epidermidis | 14 |
| Staphylococcus aureus | 13 | |
| Methicillin resistant staphylococcus aureus | 13 | |
| Other Staphylococcus | 3 | |
| Staphylococcus harmolitycus | 1 | |
| Streptococcus spp. | 2 | |
| Streptococcus agalactiae | 1 | |
| Streptococcus pyogenes | 1 | |
| Gram-negative bacilli | Escherichia coli | 21 |
| Pseudomona aeruginosa | 10 | |
| Proteus mirabilis | 9 | |
| Enterobacter cloacae | 8 | |
| Enterococcus faecalis | 7 | |
| Klebsiella pneumoniae | 5 | |
| Morganella morganii | 4 | |
| Enterococcus faecium | 3 | |
| Enterobacter aerogenes | 2 | |
| Acinetobacter iwofii | 1 | |
| Serratia marcescens | 1 | |
| Kingella spp. | 2 | |
| Gram-positive bacilli | Corinebacterium spp. | 1 |
| Fungi | Candida albicans | 1 |
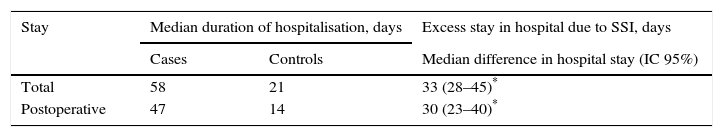
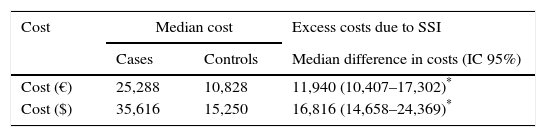
The median difference in total hospitalisation of the matched cases and controls in the 162 patients studied was 33 days. This shows that median hospitalisation of the cases was 33 days longer than it was for the controls (Table 4). Likewise, the median difference between the direct hospital costs for the cases and controls was 16,816 US$, indicating that the median cost of the cases was higher than that of the controls (Table 5).
This study confirms that SSI following hip replacement increases hospitalisation and direct costs. Compared with the controls, hospitalisation of the cases was 176% longer, while costs increased by 134%.
The excess costs detected may be explained by several factors. These include the type of microorganism which caused infection, the depth of the same and the design of the study. This research found that MRSA was an important cause of SSI in hip replacement patients, with 69% higher costs due to infection by this microorganism than was the case for costs attributable to infection by other microorganisms. Previous studies observed that some micro-organisms such as MRSA that cause surgical wound infections have been associated with longer hospitalisation and higher costs than other microorganisms, regardless of the type of surgery.10–12 In the same way, deep and organ-space infections have also been associated with higher costs.11 The latter location is the most common in our study, representing almost half of the cases in the sample. Methodological aspects such as study design also seem to influence the effect of wound infection on hospitalisation and costs. In a revision of studies of the cost of SSI, those using matched groups tended to report longer hospitalisation and higher costs than studies of independent groups.13
A single previous study in Spain estimated the excess of direct costs caused by SSI in hip replacement at 20,573 US$, based on the average cost of a bed per day in an orthopaedic unit.14 Our study, which is based on the analytical accounting of the hospital, found a lower excess cost due to infection of 16,816 US$. Nevertheless, the length of total excess hospitalisation attributable to infection was the same in both studies (33 days). Similar findings were observed previously by Broex et al.,13 who found greater consistency between studies that evaluated additional cost due to wound infection in orthopaedic surgery, in comparison with those who evaluated the costs of this type of infection following cardiothoracic surgery.
Few studies evaluating excess hospitalisation and costs due to SSI in orthopaedic surgery have been published outside Spain, and their results also vary very widely. In 2 studies published in the USA and the United Kingdom, the median increase in hospitalisation and costs ranged from 7 to 35 days and from 12,581 US$ to 20,563 US$ per admission, respectively.11,15 The inconsistency of these results may be explained by major differences between the two studies, which took place in countries with different currencies and healthcare financing systems.
Although the matched pairs made it possible to control the influence of other factors such as age, sex, main diagnosis and ASA classification on length of hospitalisation and costs, it is not possible to state that the magnitude of the observed excess stay and costs is solely due to infection of the surgical wound, or whether other comorbidities may have influenced the results. Another restriction is that this study did not include the indirect costs of SSI, such as intangible costs. It was restricted to the costs arising due to hospitalisation of the patients, excluding those costs that arose outside the hospital due to infections. According to Graves et al., 67% of the direct costs due to SSI correspond to the period of hospitalisation, while the remaining 33% derive from the use of healthcare services independent of hospitals.16 Nevertheless, this study did consider patient readmission when calculating excess length of hospitalisation and costs.
This analysis is the first study of the costs of SSI in hip arthroplasty in Spain, calculated using hospital analytic accounting without counting other indirect costs (including intangible ones). There is increasing interest in the estimation of costs due to nosocomial infection in terms of healthcare economics. Direct costs represent the real costs of the hospital due to spending per patient, while generally the indirect costs are not included in cost analysis, leading to underestimation of the true cost of such infections. In spite of these restrictions, data on direct costs offer a useful estimation of hospital costs as a result of SSI and the potential savings that would arise from their prevention. A valuation and overall appreciation of these costs should in turn lead to the assignation of resources to programs designed to prevent and control SSI. Our study illustrates the magnitude of the personal and financial costs associated with SSI, as well as the benefits for patients and the potential savings for hospitals that could arise from the implementation and maintenance of infection vigilance and control.
There are now few resources, and in a situation like the current one, in which healthcare costs are increasing continuously, studies of this type become more important. This information should make it possible for healthcare resources to be allocated more efficiently, while also encouraging similar studies in other hospitals. This will add to knowledge about the economic impact of infections, as well as confirming the need to reinforce actions with systems and programs to guard against and control infections, thereby effectively reducing SSI rates.
These findings make it possible to conclude that surgical wound infection following hip replacement is still a major cause of prolonged hospitalisation. It is also a costly complication for hospitals. Excess patient stay and the costs of SSI may be used to prioritise preventative work to monitor and control nosocomial infections. They are also indicators of the impact of the said interventions on the consumption of resources in connection with infections of this type.
Level of evidenceLevel III.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments took place with human beings or animals for this research.
Data confidentialityThe authors declare that they followed the protocols of their centre of work governing the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: González-Vélez AE, Romero-Martín M, Villanueva-Orbaiz R, Díaz-Agero-Pérez C, Robustillo-Rodela A, Monge-Jodra V. El coste de la infección en artroplastia de cadera: estudio de casos y controles emparejado. Rev Esp Cir Ortop Traumatol. 2016;60:227–233.