Allergic reactions to antibiotics are common in daily clinical allergy practice. Oral drug provocation tests (ODPT) are used to determine safe alternative antibiotics in addition to diagnostic purposes. In one of our previous studies, we have shown that triple test was a safe, time-saving and cost-effective method for determining safe alternatives for patients with non-steroidal anti-inflammatory drug (NSAID) hypersensitivity.
ObjectiveOur aim was to investigate the safety of one day two or three antibiotic ODPT performed to find safe alternative antibiotics in antibiotic/NSAID hypersensitive patients, as a cost effective and time saving alternative to conventional one day one antibiotic ODPT.
MethodsFifty-three patients were enrolled into this survey between 1 September 2005 and 31 December 2006. Double and triple tests are defined as performing ODPT with two and three antibiotics consecutively on the same day.
ResultsMean age of the patients was 41.3±11.7 years and 71.7 % were females. Beta-lactams (41.5 %) were the antibiotics most commonly causing reactions and the most common reaction was urticaria (68.8 %). Double test was performed in 26 (ciprofloxacin + clarithromycin, ciprofloxacin + tetracyline, clarithromycin + tetracycline, ciprofloxacin + ampicillin and ciprofloxacin + roxithromycin) and triple test in 27 patients (ciprofloxacin + tetracycline + clarithromycin, ciprofloxacin + tetracycline + ampicillin, clarithromycin + tetracycline + clindamycin and clarithromycin + ciprofloxacin + ampicillin). Only four patients had positive reactions during triple and double tests. There were no serious adverse reactions. Sixty-five days have been spent with tripledouble tests where it would be 136 days with the conventional method.
ConclusionThe triple-double ODPT performed with antibiotics in antibiotic/NSAID hypersensitive patients with the purpose of determining a safe alternative antibiotic could be a safe, cost-effective and time-saving alternative to conventional one day one antibiotic ODPT.
Allergic reactions to antibiotics cause substantial morbidity in addition to mortality and increase health care costs (1). Although the prevalence of reactions due to antibiotic hypersensitivity varies, the most common reactions to antibiotics are maculopapular skin eruption, urticaria, pruritus, angiooedema, and rarely anaphylaxis. The reactions occur within minutes to hours generally on second exposure to the drug after the development of sensitisation during the initial exposure1. Medical history is the most important step in the evaluation of antibiotic hypersensitivity and in differential diagnosis of other adverse reactions2. Skin, patch and provocation tests; measurement of serum tryptase level and in vitro lymphocyte transformation test may be used for diagnosing drug hypersensitivity1,3,4.
Provocation test, which includes administration of increasing doses of a drug up to maximum daily dose, can be used both for confirming the diagnosis and for determining safe alternatives in antibiotic hypersensitivity as well as in other drug hypersensitivities including non-steroidal anti-inflammatory drugs (NSAID)1,3,4. Although provocation tests can be administered in many different routes, the oral route is the most favoured one when possible3. The absorption of the drug is slower by oral route which gives the chance to treat reactions earlier and easier, compared to the parenteral one5.
One-day single-blind oral drug provocation test (SBODPT) with one drug has been used to be performed in order to determine safe alternatives in addition to confirming drug hypersensitivities in our clinic6. Different allergy clinics use various test protocols. The duration of the test may vary from a few hours to a few days3. Since generally about two thirds of our patients are referred to our clinic by physicians from other cities of Turkey, they have to pay for accommodation at least for about a week, which seems to be a hidden cost. Work/school day losses adds to this hidden cost, since most of them are actively working people or students. There is a limited number of allergy clinics in our country, so most of the patients do not have the opportunity to undergo an allergic evaluation in their home town. Because of this we have to present them safe, alternative drugs besides diagnosing drug allergy in a short time. In a previous study, we have shown that the method of triple testing to find safe alternative NSAIDs for NSAID hypersensitive patients was safe, time-saving and cost-effective7. Since two or three antibiotics are used simultaneously in many infections in clinical practice, by using two or three antibiotics consecutively on the same day to find out safe alternatives in antibiotic hypersensitive patients or to convince the ones with NSAID hypersensitivity, who can not use any drug due to their anxiety, that they do not have antibiotic hypersensitivity, we wanted to investigate the safety of one day two or three antibiotics SBODPT as a cost effective and time saving alternative to conventional one day one antibiotic SBODPT.
PATIENTS AND METHODSA total of 53 patients, 15 who had only antibiotic hypersensitivity, 17 both antibiotic and NSAID hypersensitivity, and 21 only NSAID hypersensitivity who could not use antibiotics due to fear that they could have reactions with antibiotics similar to the ones they had previously had with NSAIDs, were enrolled to the study between 1 September 2005 and 31 December 2006. The diagnosis of drug hypersensitivity was determined by history and/or skin/provocation tests as is described in the position papers by the ENDA/EAACI3–5. SBODPTs were also performed for determining safe alternative antibiotics. Double and triple tests are defined as performing the oral provocation tests with two and three antibiotics consecutively on the same day. These tests are performed in our outpatient clinic under careful observation and urgent treatment. Informed consent was obtained from each patient.
Each patient had to meet the following criteria: absence of an urticaria or angiooedema attack in the last week; stable asthma (forced expiratory volume in 1 s at least 70 % of the predicted value), and continuation of normal asthma treatment, if the patient had asthma; the time interval between the test and the suspected drug reaction was at least 4–6 weeks. Exclusion criteria were history of treatment with short-acting antihistamines during the last 24 h, long acting antihistamines up to 20 days and beta-blockers in 48 h before the test; patients with positive skin test results with the suspected antibiotic; any cardiac, haematologic, renal and gastrointestinal disorder; having one of the other contraindicated drug reactions as mentioned before3; and pregnancy or lactation.
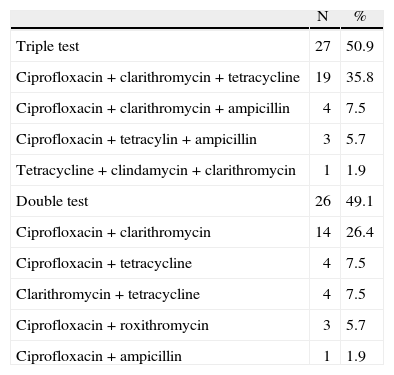
The antibiotics used during the triple-double tests were chosen depending mainly on our experience and also on the data given in the literature on the safe-considered antibiotics. Roxithromycin, tetracyline, ciprofloxacin, ampicillin, clindamycin and clarithromycin have been used in their marketed form. The combinations of drugs are shown in Table I.
Combinations of the drugs used
| N | % | |
| Triple test | 27 | 50.9 |
| Ciprofloxacin + clarithromycin + tetracycline | 19 | 35.8 |
| Ciprofloxacin + clarithromycin + ampicillin | 4 | 7.5 |
| Ciprofloxacin + tetracylin + ampicillin | 3 | 5.7 |
| Tetracycline + clindamycin + clarithromycin | 1 | 1.9 |
| Double test | 26 | 49.1 |
| Ciprofloxacin + clarithromycin | 14 | 26.4 |
| Ciprofloxacin + tetracycline | 4 | 7.5 |
| Clarithromycin + tetracycline | 4 | 7.5 |
| Ciprofloxacin + roxithromycin | 3 | 5.7 |
| Ciprofloxacin + ampicillin | 1 | 1.9 |
Drugs were administered between 9:00 and 12:00 a.m. All the patients were examined, and their basal peak expiratory flow (PEF), pulse and blood pressure values were recorded before the test. The drugs were administered in 30 min intervals beginning with placebo. The doses were 500 and 500 mg, total 1000 mg for clarithromycin, ciprofloxacin, tetracycline and ampicillin; 300 and 300 mg, total 600 mg for roxithromycin, and 150 and 150 mg, total 300 mg for clindamycin. The patients had a lunch including a simple sandwich with cheese and water and they were observed till 17:00 after the last dose of the last drug, at one hour intervals. The test was ended when the patient tolerated the planned number and doses of tested oral antibotics, or when any reaction occurred: Bronchospasm (at least 15 % drop in the PEF value), naso-ocular reactions (sneezing, nasal discharge, nasal obstruction and conjunctival irritation), urticaria (itching and erythematous lesions raise on the skin), pruritus, angiooedema (swelling of the skin and/or external mucosa) and/or systemic anaphylaxis (in addition to urticaria and/or angiooedema with more than a 30 mmHg drop in blood pressure and/or upper airway obstruction). If the test was positive, each antibiotic was administered one by one on two or three separate days. If the patients had the side effect of vomiting before 12.00 am, the tests were also repeated for each drug on separate days. If the decision to repeat the test was taken because of positivity, the repeated test was performed after at least a week, to exclude late phase reactions and possible tolerance induction. Any possible late phase reactions were evaluated by phone calls 24 and 48 hours after the test.
Oral provocation tests with NSAIDs were performed on the patients with NSAID hypersensitivity for determining safe alternatives or testing culprit drugs, or to the ones with antibiotic hypersensitivity who feared using any other drug as described before3,6,7.
Method of demonstration of time spared:
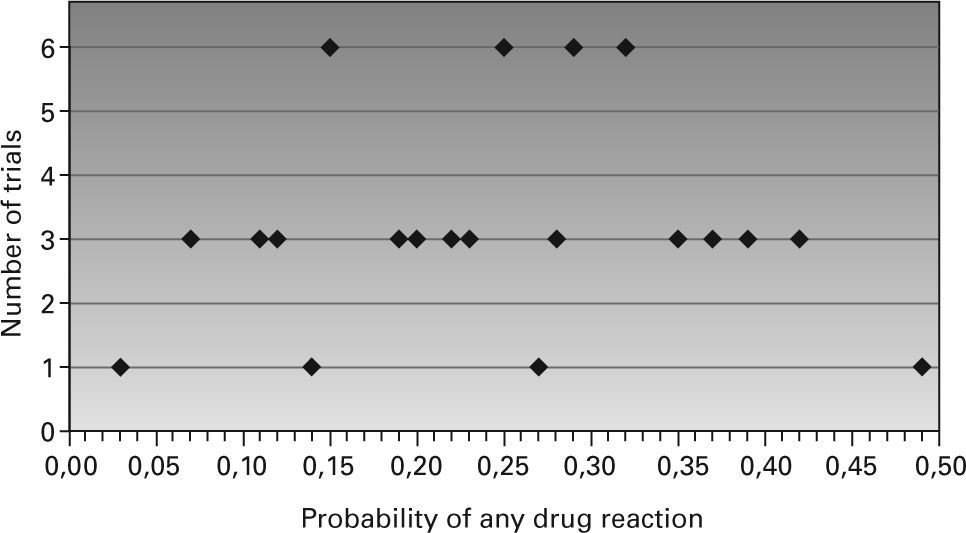
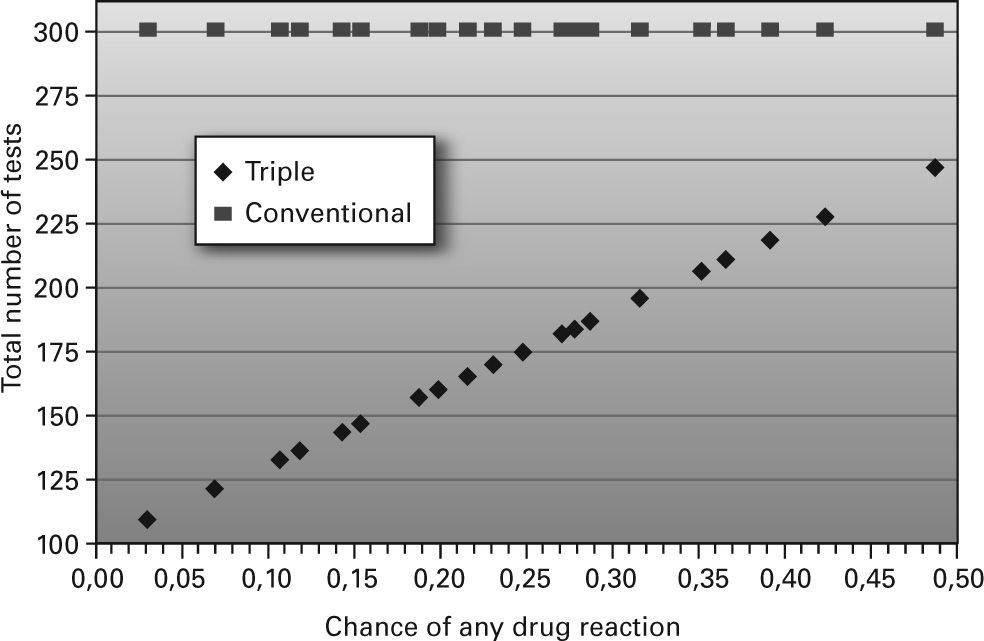
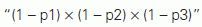
The number of the test required in triple test depends on the probability of drug reaction in the test. To have a prediction about the possibilities in the triple test we assumed that in a group of 100 patients three antibiotics were tested in each patient, and the primary testing included 300 tests in the conventional testing and 100 testing in the triple test. In the triple test there would be an additional test for each trial, if a drug reaction ensues. We calculated the number of additional tests according to the assumptions below:
- 1.
Each drug has 4 levels of risk for the drug reaction: 0.01, 0.05, 0.10 and 0.20.
- 2.
There are 64 combinations of probability for the drug reaction (4 risk levels for each drug in a row).
- 3.
For each combination, the chance of no drug reaction was calculated as:
with p1, p2, p3 as the probability of any reaction for the 3 drugs, respectively. - 4.
For each combination the chance of any drug reaction was calculated as: “1-probability of no reaction”. Probability of no reaction is calculated in the 3rd step.
- 5.
In the case of any drug reaction the tests will be repeated separately for the three drugs. The number of additional tests is calculated as: “chance of any drug reaction × 100 × 3”, as there are 100 trials, and the test will be repeated for each of the three drugs. Chance of any drug reaction is calculated in the 4th step.
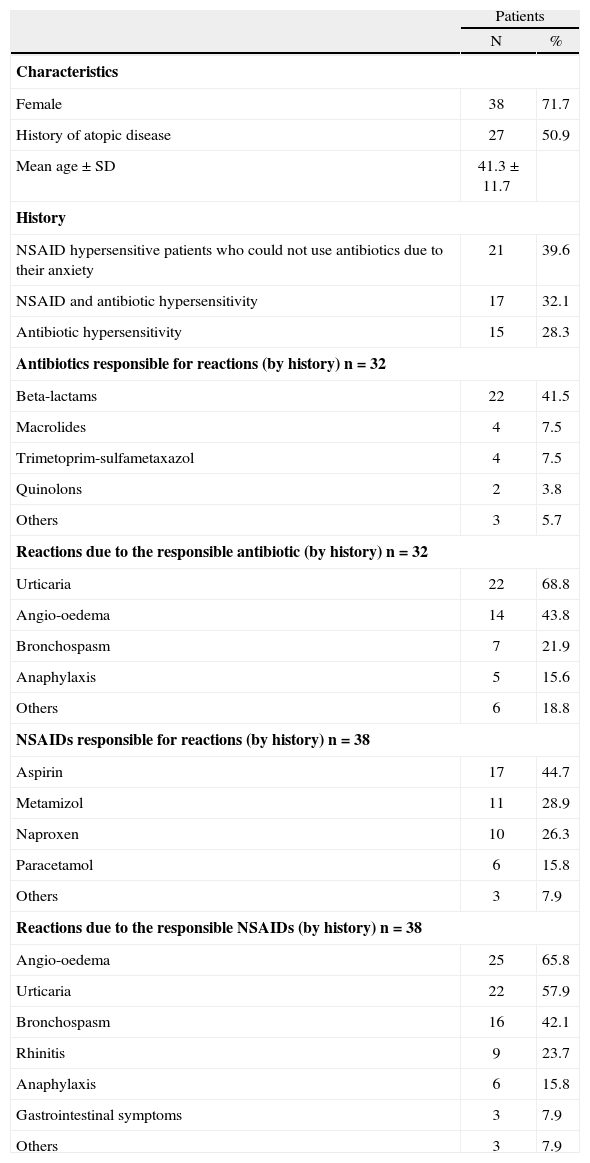
The demographic data, clinical characteristics of the patients, the drugs causing hypersensitivity and the reactions by history are shown in Table II. The most common antibiotics responsible for the reactions by history and/or skin/provocation tests were beta-lactams (41.5 %) and the most common reaction was urticaria (68.8 %).
Demographic data and clinical characteristics of the patients
| Patients | ||
| N | % | |
| Characteristics | ||
| Female | 38 | 71.7 |
| History of atopic disease | 27 | 50.9 |
| Mean age ± SD | 41.3 ± 11.7 | |
| History | ||
| NSAID hypersensitive patients who could not use antibiotics due to their anxiety | 21 | 39.6 |
| NSAID and antibiotic hypersensitivity | 17 | 32.1 |
| Antibiotic hypersensitivity | 15 | 28.3 |
| Antibiotics responsible for reactions (by history) n = 32 | ||
| Beta-lactams | 22 | 41.5 |
| Macrolides | 4 | 7.5 |
| Trimetoprim-sulfametaxazol | 4 | 7.5 |
| Quinolons | 2 | 3.8 |
| Others | 3 | 5.7 |
| Reactions due to the responsible antibiotic (by history) n = 32 | ||
| Urticaria | 22 | 68.8 |
| Angio-oedema | 14 | 43.8 |
| Bronchospasm | 7 | 21.9 |
| Anaphylaxis | 5 | 15.6 |
| Others | 6 | 18.8 |
| NSAIDs responsible for reactions (by history) n = 38 | ||
| Aspirin | 17 | 44.7 |
| Metamizol | 11 | 28.9 |
| Naproxen | 10 | 26.3 |
| Paracetamol | 6 | 15.8 |
| Others | 3 | 7.9 |
| Reactions due to the responsible NSAIDs (by history) n = 38 | ||
| Angio-oedema | 25 | 65.8 |
| Urticaria | 22 | 57.9 |
| Bronchospasm | 16 | 42.1 |
| Rhinitis | 9 | 23.7 |
| Anaphylaxis | 6 | 15.8 |
| Gastrointestinal symptoms | 3 | 7.9 |
| Others | 3 | 7.9 |
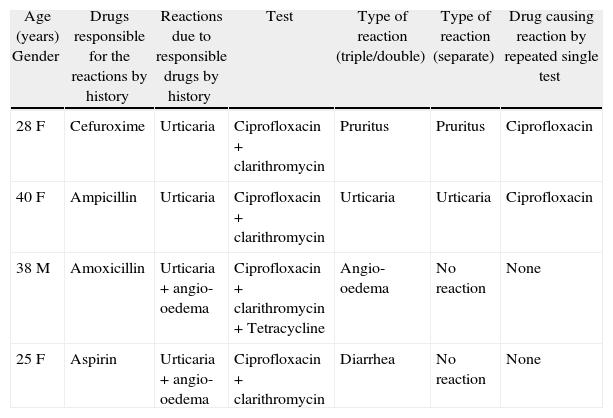
While 27 triple tests have been performed with clarithromycin, ciprofloxacin, ampicillin, roxithromycin and tetracycline, 26 double tests were performed with clarithromycin, ciprofloxacin, roxithromycin, tetracycline and ampicillin (Table I) in various combinations. The reactions appearing during triple or double tests are shown in Table III. There were no delayed reactions. Of 53 patients, only 4 patients had hypersensitivity reactions [one with triple (ciprofloxacin + clarithromycin + tetracycline) and three with double test (ciprofloxacin + clarithromycin)]. When the tests were repeated one by one on separate days two of them did not cause any reactions, whilst two of them did.
Reactions during triple or double tests
| Age (years) Gender | Drugs responsible for the reactions by history | Reactions due to responsible drugs by history | Test | Type of reaction (triple/double) | Type of reaction (separate) | Drug causing reaction by repeated single test |
| 28 F | Cefuroxime | Urticaria | Ciprofloxacin + clarithromycin | Pruritus | Pruritus | Ciprofloxacin |
| 40 F | Ampicillin | Urticaria | Ciprofloxacin + clarithromycin | Urticaria | Urticaria | Ciprofloxacin |
| 38 M | Amoxicillin | Urticaria + angio-oedema | Ciprofloxacin + clarithromycin + Tetracycline | Angio-oedema | No reaction | None |
| 25 F | Aspirin | Urticaria + angio-oedema | Ciprofloxacin + clarithromycin | Diarrhea | No reaction | None |
Ten patients had adverse reactions: nausea in six cases (additional vomiting in two and gastric pain in one of these) by ciprofloxacin + clarithromycin + tetracycline; gastric pain in one; vomiting in one; and other mild side effects in two by tetracycline + clindamycin + clarithromycin, ciprofloxacin + tetracycline, ciprofloxacin + clarithromycin + tetracycline and ciprofloxacin + clarithromycin, respectively. The antibiotics were administered separately in one of the patients who had vomitted immediately after the last dose of the triple test with ciprofloxacin + clarithromycin + tetracycline, and no reaction was observed in the repeated one.
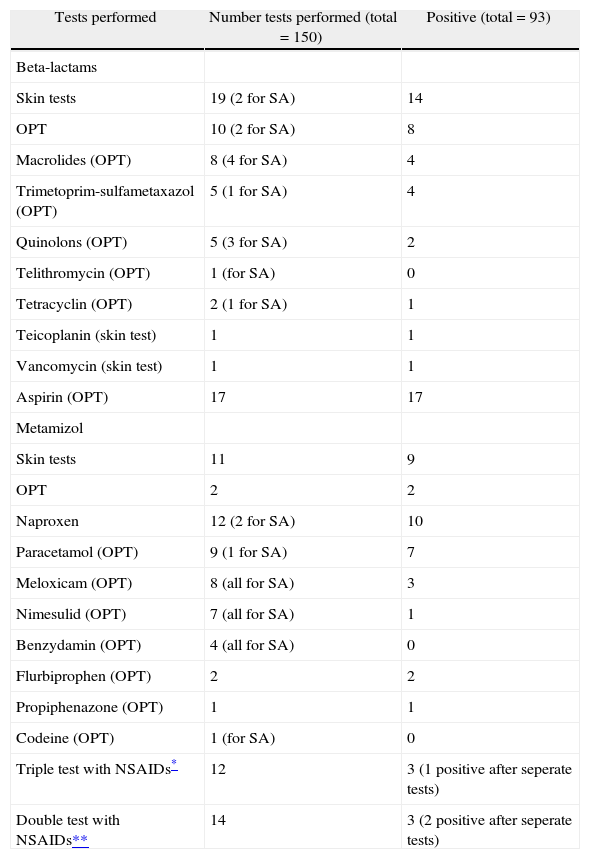
The results of skin (prick, intradermal) tests and oral provocation tests with antibiotics and NSAIDs performed with the aim of diagnosing or finding safe alternatives excluding triple-double antibiotic tests are shown in Table IV. A total (repeated tests for positive double-triple NSAID tests not included) of 150 provocation tests were performed among which 63 were for finding safe drugs including the double-triple NSAID tests. Ninety-three tests were positive of which eleven were among those performed with the aim of finding safe alternative drugs.
Results of skin and oral provocation tests with antibiotics and NSAIDs performed with the aim of diagnosing or finding safe alternatives excluding triple-double antibiotic tests
| Tests performed | Number tests performed (total = 150) | Positive (total = 93) |
| Beta-lactams | ||
| Skin tests | 19 (2 for SA) | 14 |
| OPT | 10 (2 for SA) | 8 |
| Macrolides (OPT) | 8 (4 for SA) | 4 |
| Trimetoprim-sulfametaxazol (OPT) | 5 (1 for SA) | 4 |
| Quinolons (OPT) | 5 (3 for SA) | 2 |
| Telithromycin (OPT) | 1 (for SA) | 0 |
| Tetracyclin (OPT) | 2 (1 for SA) | 1 |
| Teicoplanin (skin test) | 1 | 1 |
| Vancomycin (skin test) | 1 | 1 |
| Aspirin (OPT) | 17 | 17 |
| Metamizol | ||
| Skin tests | 11 | 9 |
| OPT | 2 | 2 |
| Naproxen | 12 (2 for SA) | 10 |
| Paracetamol (OPT) | 9 (1 for SA) | 7 |
| Meloxicam (OPT) | 8 (all for SA) | 3 |
| Nimesulid (OPT) | 7 (all for SA) | 1 |
| Benzydamin (OPT) | 4 (all for SA) | 0 |
| Flurbiprophen (OPT) | 2 | 2 |
| Propiphenazone (OPT) | 1 | 1 |
| Codeine (OPT) | 1 (for SA) | 0 |
| Triple test with NSAIDs* | 12 | 3 (1 positive after seperate tests) |
| Double test with NSAIDs** | 14 | 3 (2 positive after seperate tests) |
OPT: oral provocation test; SA: safe alternative.
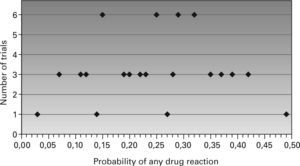
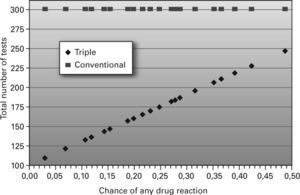
Frequency plot of the probabilities and Scatterplot graph of the number of the tests for triple and conventional test are shown in Figures 1 and 2, respectively. The number of conventional tests is fixed as 300, which is not related to these probabilities. From the graphs, it is evident that in the worst case, the chance of any drug reaction in the triple test is 0.49, giving rise to a total of 246 tests, which is still below that of the conventional test (n: 300). This is a generalised equation showing the time spared by triple-double tests clearly. When we show it by the exact numbers of our survey:
- –
Fifty-three patients have undergone triple or double tests and four of them had allergic reactions.
- –
With the conventional one day one drug single-blind oral provocation test, we needed (27 × 3 = 84; 26 × 2 = 52; 84 + 52 = 136) 136 days to perform these tests.
- –
With triple-double tests; we have spent (27 days for 27 triple tests + 26 days for 26 double tests + 3 days for one repeated triple test due to hypersensitivity reaction + 6 days for 3 repeated double tests due to hypersensitivity reactions + 3 days for one repeated triple test due to vomitting = 65 days) 65 days. Thus, we have a time spared of 71 days.
The diagnosis of drug hypersensitivity needs skin and in vitro tests, and drug provocation test (DPT) besides a detailed medical history. A DPT, which is the controlled administration of a drug, is used to diagnose drug hypersensitivity reactions or to determine the safe alternative drugs in diagnosed drug hypersensitivitoes3,4. DPT is accepted as the gold standard to determine drug hypersensitivity, and can be performed in an outpatient setting. There are different routes of administration such as oral, parenteral, topical, bronchial, etc3. ODPT is the favoured one as the absorption of drug is slower. In antibiotic hypersensitivity ODPTs can be used for determining safe alternative drugs and should be performed in allergy clinics by experienced staff. As in most other countries, there are not many allergy clinics; and all allergy clinics are not interested and experienced in drug allergy in our country. Although there are no international or national standards for ODPTs, in a classical method the test for each antibiotic lasts 1–3 days3–8. The time interval between two tests is at least two days, which is 1–2 weeks after a positive test.
SBODPTs have been performed in our clinic since 1991. We have been performing triple or double tests for determining safe alternatives in NSAID hypersensitive patients since 2002. Our clinical practice with NSAID hypersensitivity has shown that this is a safe, time and manpower-saving, and cost-effective method9. In eradication of Helicobacter pylori infections, treatment of pneumonias with co-morbidity, tuberculosis and brucellosis two or more antibiotics can be used simultaneously10–13. Depending on our experience with triple tests in NSAID hypersensitive patients and the knowledge of using more than one antibiotic in some infectious diseases, we performed double or triple tests with antibiotics. The doses used in our tests were the maximum daily, non-toxic doses.
Four double/triple tests were positive where the reactions were angiooedema, urticaria, pruritus and diarrhoea and only two separately repeated ones were positive, which were the same during the double and separate tests. These two seem to be allergic reactions, since they appeared both during the double and separate tests. There were no reactions in the other two where one of them was triple. These might be false positive reactions due to additive effects of two/three antibiotics. Although there was a time interval of a week between the positive double/triple tests and the separately repeated ones, the other possible explanation might be the tolerance induction. These reactions might also be the result of the stress due to the tests. But this is our point of view, which is open to speculation.
Among the whole group, 10 and among the antibiotic hypersensitive ones seven had gastrointestinal side effects such as nausea, vomiting, gastric pain and others. The most common one was nausea and it was generally with triple test. The reactions seem to be the result of pharmacological toxicity of drugs and dose related, which are rarely seen with the antibiotics we used14,15. Although all were mild and acceptable, these gastrointestinal side effects may be the limitation of our study, since the side effect rate is 21.9 (7 in 32 antibiotic hypersensitive patients) and 8.3 (10 in 84 NSAID hypersensitive patients) % in our current and previous surveys9, respectively.
In the triple and double test, the test has to be repeated for each drug separately if a problem is observed. The number of these additional tests depended on the probability if a reaction in the double and triple test occurred. The calculation using the exact numbers of this survey has shown that a huge amount of time (71 days) has been saved, in addition to the calculation of the total number of tests according to the different probabilities of drug reactions. As most of our patients are working adults or students coming from other cities, this shortening in the duration of the tests was very important for them.
In conclusion, although with a higher, but nonlifethreatening adverse effect rate, the triple or double oral provocation test with antibiotics seems to be a safe, time and manpower saving, and cost-effective method for finding safe, alternative antibiotics for drug hypersensitive patients as the triple test with NSAIDs in NSAID hypersensitive ones.