Food allergy is growing worldwide at an alarming rate. A group of eight foods account for over 90% of the reactions in Europe and the United States. However, little is known about the frequency of sensitization to these foods in Latin American, and if other native foods from this region are an important source of sensitization. The objective of this review was to analyse the epidemiological studies in Latin America about food allergy and to compare them with the studies in the United States and Europe.
Food is essential for life; it is also a major source of satisfaction and part of the cultural identity of each population. Adverse food reactions have been described for more than 2000 years, and their frequency is becoming an increasing public health problem in many countries.1
Currently, the term adverse food reactions (AFR) is a non-specific term meaning any undesirable reaction after ingestion or contact with food.2 It is estimated that a quarter of the population has experienced an AFR,3 with food allergy (FA) being only one type of these reactions which occurs frequently in children under three years of age (10–15%), but also in older people (6–8%).4 In most cases, these reactions are IgE mediated, and little is known about the frequency of non-IgE mediated food reactions.
Food allergies (FA) are the most studied because of their high frequency and the severity of their reactions even with small amounts of food. FA can be mediated by immunoglobulin E or cellular mechanisms and can be presented with a wide variety of symptoms in the skin, and respiratory and gastrointestinal tract.5 Although any food can potentially cause allergic symptoms, 90% of reactions occur by eight foods: in children reactions to egg and cow's milk are common, while in adults fish and shrimp are more frequent. Soy, wheat, tree nuts and peanuts are also a common cause of allergies in some countries.6
Currently, the prevalence of food allergies varies widely between studies: in self-report studies higher frequencies are found (10–15%) than when objective methods such as oral provocation are used (1–3%).7 In studies that have evaluated food sensitization by skin tests or serum IgE, it was found that 3–40% of the general population is sensitized to at least one food, this being more frequent in children under three years (5–8%) and in people with allergic diseases such as asthma (6–8%) and atopic dermatitis (30–50%).8,9 This is important because IgE sensitization is the main risk for having an allergic reaction. However, not all sensitized patients have symptoms, and when the reaction is mediated by cells, IgE sensitization is not necessary.10
Foods implicated in food allergies vary with dietary practices; while in the U.S.A. allergy to peanuts and tree nuts is high, in some regions of Spain and Portugal reactions to fish and shellfish are more common, in Israel to sesame and in France to mustard.10,11
Most studies on food allergy have been conducted in Europe and United States and little is known about food allergy in Latin America, where there is a high cultural diversity which makes dietary habits and food preparation different to European countries and the United States. In Latin America, the second most common cause of anaphylaxis reactions was associated with foods, being various fruits primarily involved.12 The tropical and subtropical climate promotes the growth of a high number of fruits in Latin America, and eating them could increase the risk of food sensitization.
Although several Latin American groups are describing allergenic proteins and trying to produce hypoallergenic foods,13,14 little is known about the frequency of sensitization to foods and possible risk factors in Latin America, so the aim of this article is to review the available information on the epidemiology of sensitization and food allergy in Latin America and see if there are important differences with the frequency reported in Europe and the United States, taking into account the main foods involved, the underlying immune mechanism, and the clinical symptoms associated with allergic reactions.
MethodologySetting the research questionThe objective of this research is to review the articles published about the epidemiology of food allergy made in Latin America.
Selection of articlesWe searched through PubMed and LILACS database, all original articles in English, Spanish or Portuguese performed with Latin Americans populations and published in scientific journals before March 31, 2013. For the search the following keywords were used: allergy, food, asthma, dermatitis, eczema, atopy, rhinitis, milk, egg, shrimp, fish, peanuts, nuts, soy, wheat, beans, corn, cohort, Latin America, Argentina, Colombia, Venezuela, Peru, Mexico, Brazil, Ecuador, Chile, Belize, Guatemala, Honduras, Salvador, Nicaragua, Costa Rica, Panama, Cuba, Haiti, Dominican Republic, Puerto Rico, Jamaica, Guyana, Bolivia, Paraguay, Uruguay.
The search included all kinds of diseases associated with a food allergic reaction (hives, otitis, etc.), with emphasis in eczema, asthma, rhinitis and gastrointestinal symptoms.
Data obtained were classified according to: (A) area where the study was conducted. (B) Frequency of sensitization to different foods sources. (C) Characteristics of the subjects (atopic/no atopic, paediatric/adult). (D) Allergic symptoms (gastrointestinal, respiratory, skin, etc.). (E) Type of test used to evaluate sensitization (intraepidermal test, intradermal, patch) and clinical relevance (diet restriction/challenge).
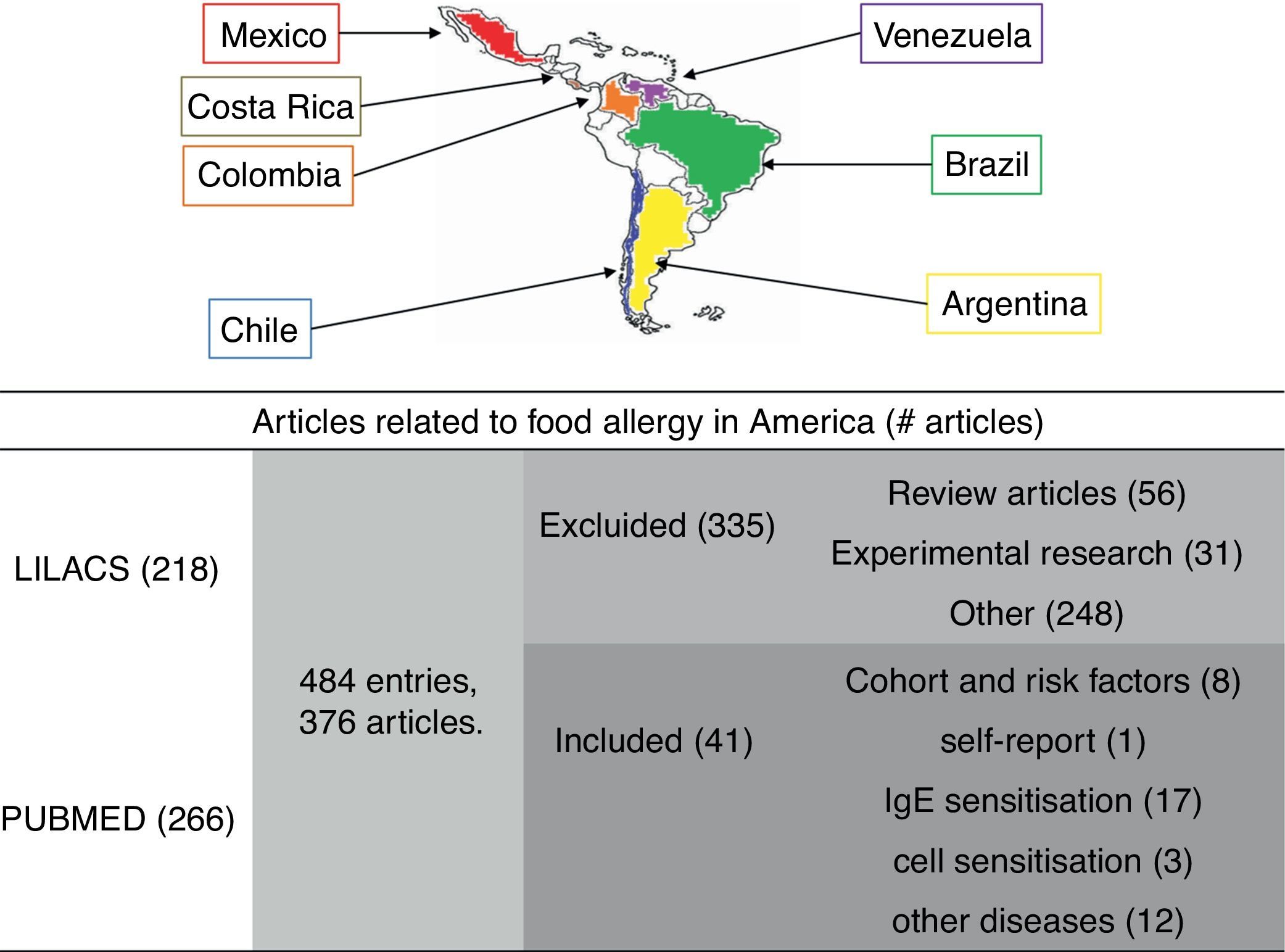
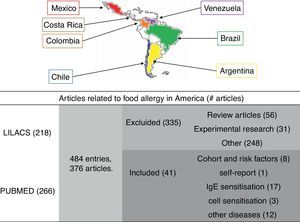
ResultsArticles includedSearch on Pubmed (218) and LILACS (266) yielded a total of 484 articles. We found with the EndNote Program that both databases shared 108 articles, so the net number was 376 articles (Fig. 1). 112 items (29.7%) had only a printed version. According to the title and abstract available online, six of them could have served in this review but we could not access the full texts.
Methodology. A systematic search of all articles about food allergy from Latin America, registered in PUBMED and LILACS. 376 articles were found, although only 41 met the selection criteria. Countries with epidemiological publications on food allergy are marked with colours: Mexico (red), Costa Rica (brown), Colombia (orange), Venezuela (purple), Brazil (green), Chile (blue), Argentina (yellow).
Only 41 articles were related to original epidemiological investigations, most of them from Mexico (58%). We found no publications on the topic in Ecuador, Belize, Guatemala, Honduras, Salvador, Nicaragua, Panama, Cuba, Haiti, Dominican Republic, Puerto Rico, Jamaica, Guyana, Bolivia, Paraguay and Uruguay.
Definition of termsWe found different definitions between articles for terms as “Allergy” and “Sensitization”. We decided to organize the results taking into account the definitions proposed by the World Allergy Association15:
Hypersensitivity: Hypersensitivity is signs or symptoms objectively reproduced after exposure to a defined stimulus at a dose tolerated by most individuals.
Allergy: Allergy is a hypersensitivity reaction initiated by a specific immune mechanism.
Allergen: Is an antigen capable of developing an allergic response.
Sensitization: IgE or cell response to an antigen.
Atopy: A personal or family tendency, usually in children and adolescents, to be sensitized and produce antibodies in response to ordinary exposure to allergens. As a result, they can develop typical symptoms of asthma, rhinitis, conjunctivitis, or eczema.
Risk factors and Latin America cohort studiesIn recent years some cohort studies of children followed from birth, are being carried out in several Latin American countries16; this has allowed a better understanding of the characteristics of allergic diseases in the tropics and to identify potential risk factors for food allergy and food sensitization. These studies have also demonstrated that food allergy is a risk factor for the development of other allergic diseases.
In Campinas, Brazil, López et al., in a prospective study of 114 infants, assessed the clinical manifestations of allergy during the first year of life.17 According to the authors, 32 (28%) patients developed atopic disease during the first year of life: 29 had recurrent wheeze (two or more episodes in less than a year), two had allergy to cow's milk and one had atopic dermatitis. Breastfeeding for less than six months and poor socio-economic conditions were the main risk factors found for the development of allergies (p<0.01), and specific IgE levels to cow's milk, egg white and mites was higher in infants with recurrent wheezing.18 In another birth cohort conducted in Brazil,19 which included 104 children from families of low socioeconomic status, they found that the frequency of recurrent wheezing (more than three times in one year) was lower in children breastfed exclusively for the first month of life (OR 0.09, 95% CI 0.01–0.51 p<0.01), perhaps due to a lower risk of viral infections. In a birth cohort of 300 children who lived in poverty (according to criteria of the World Health Organization) followed and studied by us in Colombia,20 we did not find a significant correlation between weaning and the development of skin, respiratory or gastrointestinal symptoms, despite the introduction of foods including eggs and milk which occurred in 80% of cases between two and four months. Only two cases of rash and wheals were induced by ingestion of egg and milk. However, we observed that children exclusively breastfed for at least the first three months of life, had a higher concentration of Bifidobacterium infantis in the faeces, and that the lower colonisation with Lactobacillus species was associated with wheezing.21
In Chile, Bascuñán Gamboa et al.22 observed in a case study (50 children) and controls (49 children) that family history and early weaning were strongly associated with the development of food allergy during the first year of life. The FA was defined in this study as “manifestations of allergic sensitization that improvement with restricted diets”. Chavarria et al., in Costa Rica,23 observed that weaning occurred frequently at three months with the introduction of cow's milk and egg, concluding that there is no sensitization in the general population of the importance of breastfeeding as a protective factor in infants at high risk of allergic disease and avoidance of highly allergenic foods during the first months of life. A study in the Federal District of Mexico by López Pérez et al.24 assessed risk factors for allergies in a population of 4742 patients between 1 and 98 years, of which 42% had allergic disease: 15% asthma, 20% rhinitis, 18% conjunctivitis, atopic dermatitis 19% and 4% urticaria. They found that between the allergic and non-allergic population there were no significant differences in the weaning period, but did observe that the family inheritance and early consumption of cow's milk, egg, fish, meat and legumes was associated with the onset of allergic disease. The results of this cohort suggest that rather than weaning, the type of food introduced would increase the risk of developing allergic disease. However, there may be a memory bias since these data were collected retrospectively.
In a study in Brazil paediatricians’ knowledge about food allergy was assessed25: 895 paediatricians completed the questionnaire focused on questions about the clinical symptoms of patients and FA management. The prevalence of clinical symptoms and the foods involved were similar to those reported in other studies, with cutaneous manifestations being the most frequent, with egg and milk food being the main suspects. However, in the diagnosis of FA the study concludes that paediatricians have poor information, since most do the diagnosis only with medical records (97%) and do not use confirmatory tests, performing aggressive management as extensive restriction diets are usually not necessary and they do not avoid foods with cross-reactivity.
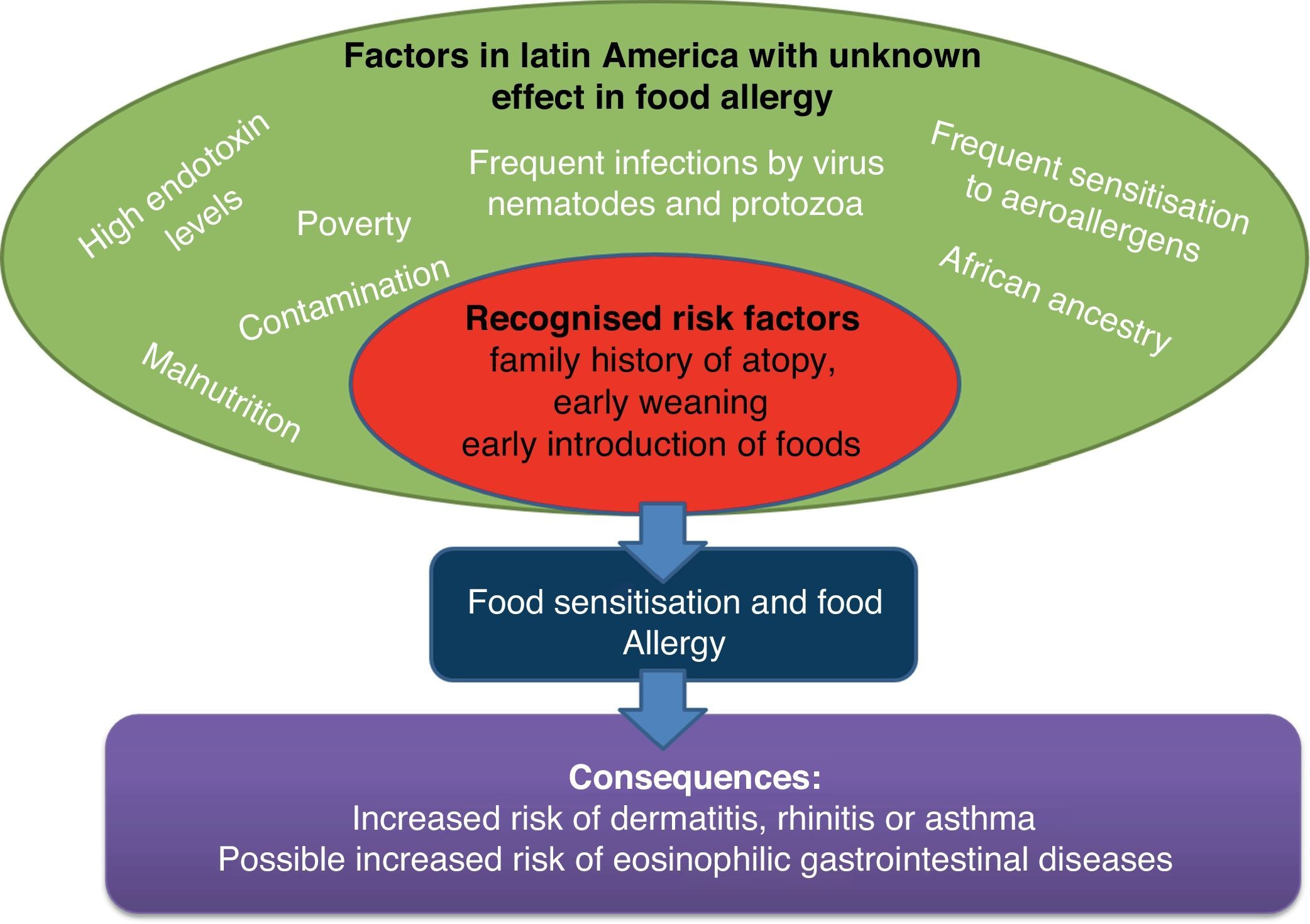
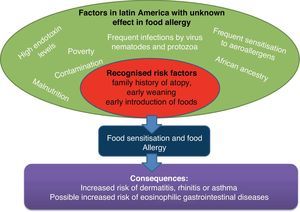
Considerations of cohort studies (Fig. 2): Currently, medical doctors in Latin America need more information about appropriate prevention measures of food allergy. The main risk factor identified in Latin American birth cohorts were a family history of atopy and early weaning especially with milk and egg. Because the risk and protective factors vary among populations, more birth cohort studies are needed.
Self-report of AFRThe only Latin American study which evaluated the frequency of AFR was conducted in Cartagena, a city on Colombia's Caribbean coast, by Marrugo et al.26 A total of 3099 individuals with an age range of 1–83 years were surveyed and it was found that the prevalence of self-reported AFR was 14.9% (461 subjects). Fruits and vegetables (41.8%), seafood (26.6%) and beef (20.8%) were the principal suspects. Interestingly, cow's milk and egg were associated in less than 10% of cases. The most frequent symptoms were in skin (61.4%) followed by gastrointestinal (29.1%) and respiratory (8.6%) symptoms. Subjects with suspicion of allergic diseases such as asthma, rhinitis or dermatitis most often reported having had an AFR (62.9% vs. 29.6% p<0.001), showing a link between these diseases and atopy.
Considerations of self-report studies: The number of patients and selecting multiple sectors in the city allows to establish the main foods associated with AFR in this population. However, it is known that self-report studies tend to have over-estimated frequencies, and do not measure the frequency of food sensitization and FA.27 To reveal the underlying mechanism of the reactions, confirmatory tests are needed.
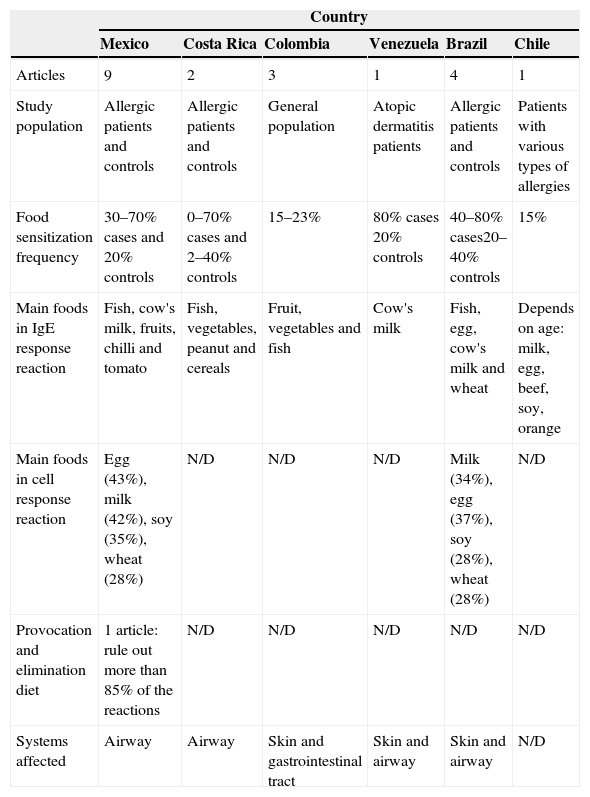
IgE-mediated sensitizationFrequency of food sensitization has been reported in some cities from six Latin American countries: Mexico, Brazil, Colombia, Costa Rica, Chile and Venezuela. Each of the articles will have different aims, different age groups, and use different methodologies, making it difficult to conduct a meta-analysis or systematic review to comprehensively present the results in Latin America, so we decided to present the results according to each country doing a detailed review of each one (Table 1).
Features of food allergy in Latin American countries. N/D: no data.
| Country | ||||||
|---|---|---|---|---|---|---|
| Mexico | Costa Rica | Colombia | Venezuela | Brazil | Chile | |
| Articles | 9 | 2 | 3 | 1 | 4 | 1 |
| Study population | Allergic patients and controls | Allergic patients and controls | General population | Atopic dermatitis patients | Allergic patients and controls | Patients with various types of allergies |
| Food sensitization frequency | 30–70% cases and 20% controls | 0–70% cases and 2–40% controls | 15–23% | 80% cases 20% controls | 40–80% cases20–40% controls | 15% |
| Main foods in IgE response reaction | Fish, cow's milk, fruits, chilli and tomato | Fish, vegetables, peanut and cereals | Fruit, vegetables and fish | Cow's milk | Fish, egg, cow's milk and wheat | Depends on age: milk, egg, beef, soy, orange |
| Main foods in cell response reaction | Egg (43%), milk (42%), soy (35%), wheat (28%) | N/D | N/D | N/D | Milk (34%), egg (37%), soy (28%), wheat (28%) | N/D |
| Provocation and elimination diet | 1 article: rule out more than 85% of the reactions | N/D | N/D | N/D | N/D | N/D |
| Systems affected | Airway | Airway | Skin and gastrointestinal tract | Skin and airway | Skin and airway | N/D |
Mexico has tropical and subtropical climates and has a high cultural diversity. Throughout its territory, several studies have been conducted to determine the prevalence of FA. Avila Castañón et al.28 reported in the Hospital Federico Gómez located in Mexico City, that 1.04% of the patients were there for suspected food allergy. In this centre, among the 1419 patients with suspected allergic disease, 442 (31%) had sensitization to one or more foods tested by skin tests and read by the method of Aas. The battery tested consisted of 33 foods, mainly fruits and vegetables; they found that the age group most affected were children aged between 4 and 7 years (49%) followed by children under three years old (24%). The most frequent foods were fish (12%), milk (7.7%), seafood (6.5%), soybeans (4.3%), beans (4.3%), orange (4.1%), onion (3.7%), tomato (3.6%), nuts (3.5%), chicken (3.5%), lettuce (2.7%) and strawberry (2%). Allergic diseases associated with food sensitization were mainly asthma and/or rhinitis (41%). There were no patients with gastrointestinal reactions. Importantly, in this study there was no sensitization to egg, and other foods of high consumption in the Mexican population such as tomato, onion and orange, were important sources of allergens. Similar results were observed in the same city by Ortega et al.29 with 356 patients with suspected of allergic asthma, rhinitis or dermatitis. Patients reported especially respiratory symptoms (85%) with a high diversity of foods: olives, avocado, cherry, plums, apricots, dates, peach, strawberry, fig, lemon, apple, mango, mamey, orange, pineapple, banana, milk, egg and shrimp. However, skin test demonstrated only sensitization in five patients with peach (1/18 patients), pineapple (2/20) and apple (2/20).
In Mexico City, with 50 randomly selected patients with rhinoconjunctivitis Ortega Cisneros et al.30 observed that food sensitization was present in 50% of patients; 10 (20%) of whom had no sensitization to aeroallergens. Foods involved were: seafood (16%), tomato (10%) and pear (8%). Other less common sources (<6%) were: rice, peanuts, carrots, casein, snapper, sierra, chicken, beans, nuts, peas, cocoa, apple, avocado, sea bass, shark, mango, wheat, beef, pork, soybeans, lentils and mango. The authors observed that serum IgE was higher, and cytology in ocular mucosa showed eosinophils increased in the food sensitization group (p=0.023) compared to patients positive to aeroallergens. All these results indicate that in a subset of patients with rhinoconjunctivitis, sensitization to food may be even more relevant in the development of symptoms than aeroallergens.
In Monterrey city, Rodríguez-Ortiz et al.31 evaluated the histories of 60 patients with FA who reported gastrointestinal symptoms (23%), cutaneous rash (38%), eczema (15%) and cough or wheezing (17%). 76% of patients had two or more sensitizations to food and only 20 patients (33.3%) were positive for a single food. Unlike Mexico City, the highest sensitization was with milk (28%) and eggs (21%), followed by fish (18%), shrimp (10%), beans (10%) and soybeans (10%). However, it was also observed sensitization to chilli (8.3%), mango (8.3%), cocoa (8.3%), strawberry (6.6%), almonds (6.6%), mustard (6.6%), cauliflower (6.6%) and peanuts (5%). In the region of Coahuila, Ramos Morín et al.32 evaluated food sensitization in 247 patients with suspected food allergy and found that wheat (21.3%) was the most allergenic source followed by milk (10.0%), seafood (10.0%), pork (8.8%) and egg yolk (7.5%). In Puebla, Mendez et al.33 reported that in 312 patients with suspected of allergies, sensitization to food was 65% (202/312) and noted that the major allergenic foods were grapes (38%), peanuts (34%), egg (33%), egg yolk (25%), pineapple (28%), chocolate (27%), beef (25%), tomato (23%), milk (23%) and plum (22%). In the same area, Orozco Suárez et al.34 found that in a group of 1101 patients with allergic symptoms, sensitization to pollen grains was high. 50% of the sensitization was with family of grasses, legumes, Rosaceae and Solanaceae. Although peanut is a legume, sensitization with it was low (<5%).
Medina Segura et al.35 evaluated the frequency of food sensitization in 119 atopic dermatitis patients from Monterrey. 48 (40%) patients had a clinical history with suspected allergic reaction to a food, and sensitization was demonstrated by skin tests in 25 (56.8%) of these patients to egg (66%), milk (10%), corn (6%), chicken (8%), pork (4%), wheat (4%) and potatoes (4%).
A case–control study was conducted in Mexico City by Rosas Vargas et al.36 in asthmatic and non-asthmatic children evaluating food sensitization. This study showed that food sensitization was 35.4% (27/74) in the case group and 20% (15/74) in the control group. They also observed that patients sensitized to a foodstuff had a 2.2 times greater risk of developing asthma.
Considerations of food IgE sensitization studies in Mexico: The results found in Mexico, show that in general, sensitization to egg and peanuts is less than that reported in the United States (U.S.) and Europe, where these sources account for almost 80% of FA.5,6 It is also important to note that other sources infrequently described in European and U.S. populations, such as corn, beans and chilli have a proportionally high prevalence in the Mexican population, perhaps because they are highly present in their diet.
It is difficult to compare frequencies in Mexico with trials in other countries because in several allergy services in Mexico intradermal tests are read with the method of Aas and this methodology is little used in other countries and has low sensitivity compared to currently used methods.8,37 Except for the study of Rosas Vargas et al., all studies in Mexico evaluating the frequency of IgE sensitization were performed in allergic patients. It is necessary to evaluate the frequency of FA and the AFR in the general population. It is also necessary to confirm the relevance of sensitization to food by eliminating tests and/or provocation test.
BrazilBrazil is the Latin American country with the highest number of articles published related to food allergy; however, only two articles were related to food allergy epidemiology.
Naspitz et al.38 evaluated sensitization to cow's milk, egg, wheat, peanuts, soybeans, corn and fish in a case–control study (457/62 children) with children under 12 years old, attending allergy services in some cities from Brazil with gastrointestinal symptoms (3.5%), atopic dermatitis (12%), respiratory symptoms (80%) and other symptoms (4%). Although no food was associated with a specific allergy, the presence of IgE to these foods was higher among patients (79%) than controls (25.8%) with the main source of allergens being fish (29.5% vs. 11.3% p<0.05), followed by eggs (24.4% vs. 4.8% p<0.05), cow's milk (23.1% vs. 3.2%, p<0.05), wheat (20% vs. 8.1% p<0.05), peanuts (14% vs. 4.8% p<0.05), soybeans (11.8% vs. 4.8% p<0.05) and corn (10.6% vs. 4.8% p<0.05). The sensitization to milk was prevalent in children below two years.
In Sao Paulo, Tassi et al.39 studied sensitization to food in 110 patients (1–66 years old) with atopic dermatitis. Only 26 (23.6%) associated exacerbation of symptoms after the consumption of one food. All patients were evaluated with egg, cow's milk, cod, almonds, wheat and soybeans, but were also tested for suspected foods from each patient (peanuts, rice, bananas, potatoes, cocoa, coffee, shrimp, fish, carrot, beans, chicken, oranges, wheat, soy, corn, olive, pork, tomato). A total of 46 (42%) patients were sensitized to at least one food; from the 26 patients with AFR 11 (46%) were sensitized with the suspect food. Due to the high frequency of sensitization among patients with no history of AFR (41%), sensitivity (42%) and specificity (58%) of the skin test and serum specific IgE was low. These results highlight the trouble for patients with atopic dermatitis to identify foods involved in cutaneous exacerbations, in part due to the severity of the underlying disease and because in the preparation of food products multiple ingredients are involved, hindering the correct identification of the causal food.
Considerations of food IgE sensitization studies in Brazil: Naspitz and collaborators, through a unified panel of foods in several cities of Brazil, showed that food sensitization is similar among the five regions of Brazil, but varies according to the patient's age. The panel was limited to six foods and did not include other specific foods in the diet of each region, which could be important, as demonstrated in Mexico. In the study of Tassi et al., there was a significant sensitization of different sources not usually described – specially fruits, however, it is unclear how many patients from the AFR group were sensitized to the suspected food because there is a contradiction between the abstract and the text (abstract and page 103). Another limitation in this study is that it the sensitization frequency of each food tested by prick test and specific IgE is not clear. Care must be taken when interpreting the results of food allergens tests, especially in patients with atopic dermatitis, to prevent unnecessary restriction diets.
ColombiaIn Colombia, two articles have been published exploring the epidemiology of AFR and FA in the general population – the first was the study from Marrugo et al., already described, and the second was performed in the city of Bogotá by Leal et al.,40 who evaluated sensitization to 10 tropical foods in 160 children under two years old: the foods proved were guava, papaya, banana, passion fruit, mango, tree tomato, corn, yellow potato, soybean and cassava. These fruits are the most frequent foods first introduced into the diet of infants in Bogota. By measurement of specific IgE (Immundot), they detected 47 (23%) children with sensitization to one food; the most common was corn (12%), banana (10%), guava (4%), yellow potato (2%) and mango (1%). The sensitization was higher in children younger than six months and none was sensitized to cassava, soybeans, tree tomato, passion fruit and papaya.
Considerations of food IgE sensitization studies in Colombia: The high frequency of sensitization reported in this study indicates the importance of testing native foods of each region. More trials are needed to evaluate the relationship between sensitization to these foods and the development of allergic symptoms.
Costa RicaSoto-Quiros et al.41 evaluated, in 98 schools of Costa Rica, food specific IgE sensitization (MAST system and Phadia) for 15 foods tested in 183 children with asthma and 275 without asthma. The food sensitization among asthmatics was 60%, and 40% among non-asthmatics. Sensitization in the asthmatic group was with fish (60%), mixed vegetables (58%), almonds (54%), garlic (53%), yeast (51%), wheat (50%), soybean (48%), egg (48%), milk (43%), peanuts (42%), corn (40%), onion (38%), orange (28%) and cereal mixture (15%). In the non-asthmatic group the sensitization rate was very similar to the asthmatic group, being significantly lower for wheat and egg but higher for peanuts (48%) and soybeans (50%). The high sensitization in the non-asthmatic group could be explained by other allergic diseases such as rhinitis and dermatitis present in 39% of those children.
In another case–control study conducted in Costa Rica by Riggioni et al.,42 with 184 patients with allergic rhinitis and 100 controls, the frequency of sensitization observed was greater than 60% for corn, sorghum, sugar cane and rice among rhinitis patients, compared to only 2% in controls. These species share a special mode of pollination that is not seasonal, which may explain its association with perennial allergic rhinitis.
Considerations of food IgE sensitization studies in Costa Rica: The case–control studies conducted in Costa Rica show the differences in food sensitization pattern among various allergic diseases. As in other countries from Latin America, there are few studies in Costa Rica about food epidemiology and there is no challenge tests evaluation, so is difficult to know if the high frequency of sensitization to foods has a real impact in the development of these diseases.
ChileMartínez et al.43 evaluated food sensitization in 408 children with allergic diseases. Foods included were chicken, beef, orange, tomato, chocolate, banana, cow's milk, egg, peanut, fish, shrimp, soy, wheat and nuts. Population was distributed according to age range in children under 3 years of age (29 patients), 3–5 years (83 patients) and over 5 years (296 patients). Sensitization to at least one food in each group was 12%, 8% and 18%, respectively. The foods most frequently found in the group of children less than two years were milk (7%) egg (7%), beef (7%) and seafood (4.6%). In the group of 3–5 years, they were milk (2%), seafood (1%), peanuts (1%) and soybeans (1%). In the group older than 5 years, milk (5.9%), orange (3%), wheat (3%) and fish (2.8%) were the main food sensitizations.
Considerations of IgE sensitization studies in Chile foods: Although the only published study in Chile has some limitations such as the lack of correlation of sensitization with clinical history, it is remarkable, that together with the eight most common allergenic foods, they included six different foods and showed a high frequency of sensitization with beef in children under two years and with orange in children over five years. These data highlight the importance of testing the suspected food for the patient and those of high consumption in each area.
VenezuelaNavarro et al.44 compared 56 patients with atopic dermatitis and 53 controls to determine the relationship of atopic dermatitis, food allergy and gastrointestinal symptoms. Among patients with dermatitis, 45 (80%) were sensitized to one food with cow's milk being the most frequent (48%). Gastrointestinal symptoms were associated with sensitization (p<0.05) and also with atopic dermatitis (p<0.0001 correlation r=0.99).
Considerations of IgE sensitization studies in Venezuela: In this study FA diagnosis was confirmed with improvement in symptoms after elimination diets which strengthen the strong association found between gastrointestinal symptoms, food sensitization and atopic dermatitis. This study contrasts with results of Tassi in Brazil, where food sensitization did not show a strong correlation with symptoms in patients with dermatitis. The discrepancy between studies highlights the need for multicentre studies that include different Latin American countries.
Cell response assessmentPatch test is a simple and secure method to confirm or rule out the suspicion of a cell-mediated reaction, especially in patients with atopic dermatitis where late reactions are common. However, there is an active debate about the utility of the patch test due to the high frequency of false positives and lack of universal standardisation of the test. In Latin America, studies evaluating FA cells mediated by patch tests are scarce. Levy et al.45 observed correlation between skin test, specific IgE levels and patch, testing foods in a group of 72 children with suspected FA between 2 and 12 years, who were divided between those who had respiratory allergies and those who had skin allergy (dermatitis), and were compared with a control group. Among 32 patients with dermatitis, 40% had a positive patch test, 34% to milk, 37% egg, 28% soy and 28% wheat. In the group of 26 patients with asthma and/or rhinitis, 19% were positive to cow's milk, 11.5% eggs, 15% soy and 11.5% to wheat. They observed that readings at 72h had higher sensitivity and specificity. These results agree with those published in Europe which shows that patients with dermatitis are at increased risk of cell-mediated reactions to food, however it is important to note the high frequency of reactions in patients with asthma and rhinitis found in Brazil.
In a study in Mexico, Estrada-Reyes et al.46 compared sensitization to milk, egg, wheat, soy, legume and fish by intraepidermal tests or patch tests (milk, egg, wheat and soy) in 28 children under three years who had atopic dermatitis and 28 children without dermatitis. They observed that the joint evaluation with the two tests was able to predict an increased risk of dermatitis (OR=4.2, 95% CI 1.3 to 13.4) which was not achieved with a single test. Sensitization evaluated by patch test was higher in patients with dermatitis, especially to egg (43% vs. 18% controls DA) followed by milk (42% vs. 18%), soybeans (35.7% vs. 18%) and wheat (28% vs. 18%). IgE-mediated sensitization to egg was also higher in the group with dermatitis (25%) followed by legumes (25%), milk (17%), fish (17%) and soybeans (17%), while in the control group, legumes (21%) and fish (14%) were most frequent.
Considerations about patch test studies: Both studies show that the patch test may be useful to detect the cellular response to food. The reading at 72h following the patch test and the combination of patch and prick test appear to reduce the false positive rate in both studies. In the Brazilian study they do not report prick test and specific IgE results, making it difficult to objectively analyse these data. It is necessary to prove if the patch test may be useful in evaluating other foods that have shown relevance in Latin America and are different from those traditionally evaluated in this test.
Challenge test and elimination dietThe oral challenge test and the elimination diet are confirmatory tests for AFR. However, because the provocation test can be risky and the elimination diet without prior confirmation is difficult to maintain, both are in the last step of the studies for AFR and FA. Madrigal et al.,47 in Guadalajara (Mexico), evaluated the medical records of children less than four years of age with a history of AFR and with a confirmation test (elimination diet and/or challenge test). Taking into account the characteristics of the episode, patients were classified according to how strong the probability was that the reaction had been due to a food. From the 291 children assessed only 22 had a high suspicion of RAA; with the provocation testing and/or the elimination diet only 11 (50%) of the 22 patients were positive which represents 3.7% of all patients; five patients with milk, two with eggs, one carrot, one meats and two to preservatives in food.
Considerations about challenge studies and elimination diet: this study provides interesting facts – a good history can rule out a large number of AFR reported by the patient without requiring extra tests. Among patients with high suspicion, confirmatory tests are necessary because patients with reaction history can generate tolerance with time. A limitation of these tests is that they do not provide information on the underlying mechanism of the reaction, but the study of Navarro in Venezuela showed a good correlation between positive skin tests and the result of the elimination diet, which shows that in AF reactions, skin tests and serum specific IgE allowed in a number of cases to avoid confirmation tests.
Food sensitization in other diseasesFood sensitization has been studied in other diseases different to asthma, dermatitis or rhinitis. A case–control study in Chile48 showed no association between peptide disease and food sensitization assessed by skin tests and specific IgE, while other gastrointestinal diseases such as irritable bowel syndrome, have been associated with increased sensitization to foods in Brazil.49 Some studies with eosinophilic oesophagitis have been made in Puerto Rico,50 showing association of the disease with food especially in the paediatric population.
In the case of urticaria, the association with food has been studied for many years with different results; although in Brazil51 a frequent association of the disease was found with some foods, in Argentina52 and Mexico53 it was not observed that sensitization to foods in patients with urticaria was higher than in the general population.
Patients with spina bifida frequently have latex sensitization and consequently cross-reactivity with fruits.54 However, a study conducted in Venezuela by Capriles-Hulett et al.55 observed that sensitization of 93 patients with spina bifida to latex was low (4.3%) compared to that reported in other studies, and tropical fruits sensitization was not present. They explain this low sensitization to latex avoidance measures being developed in surgery rooms in Venezuela.
A study in Mexico found that in 52 of 56 patients with migraine suspension of foods with IgG-mediated sensitization, led to a marked improvement of symptoms.56
Valencia Zavala et al.57 evaluated 661 Mexican people sensitization with Zea mays. A total of 171 (26.4%) people were sensitized. Of this group, 56 (32.7%) suspected allergy to this source and 50 manipulated corn in their work environment. The most frequent symptoms were asthma or rhinitis. These results highlight the importance of studying food as potential causes of occupational allergy.
Otitis media has also been found in some cases associated with food allergy. Arroyave CM58,59 checked the files of 25 Mexican children with recurrent otitis associated with food; (10/25), egg (8/25), beans (7/25), citrus (6/25), tomato (6/25), pork (3/25) and soybeans (3/25). When the suspected food was removed, clinical symptoms and tympanometry improvement occurred in 22 patients. Children who did not suspend all food had several relapses before parents became aware of the importance of the elimination diet.
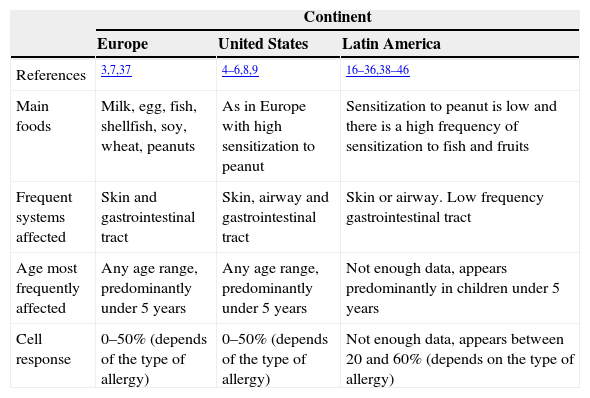
Considerations and future perspectivesGlobally, existing studies about FA are difficult to compare due to variations in the definition of FA and differences in the food panel tested27,60 (Table 2).
Comparison between the characteristics of food allergy in Europe, U.S. and Latin America.
| Continent | |||
|---|---|---|---|
| Europe | United States | Latin America | |
| References | 3,7,37 | 4–6,8,9 | 16–36,38–46 |
| Main foods | Milk, egg, fish, shellfish, soy, wheat, peanuts | As in Europe with high sensitization to peanut | Sensitization to peanut is low and there is a high frequency of sensitization to fish and fruits |
| Frequent systems affected | Skin and gastrointestinal tract | Skin, airway and gastrointestinal tract | Skin or airway. Low frequency gastrointestinal tract |
| Age most frequently affected | Any age range, predominantly under 5 years | Any age range, predominantly under 5 years | Not enough data, appears predominantly in children under 5 years |
| Cell response | 0–50% (depends of the type of allergy) | 0–50% (depends of the type of allergy) | Not enough data, appears between 20 and 60% (depends on the type of allergy) |
Recently, Boye61 carried out a review on the epidemiology of food allergy in developing countries, and noted that the current data was inadequate to perform a systematic review or meta-analysis. We found the same difficulty with the studies conducted in Latin America, the heterogeneity of the trials and the lack of uniformity in the foods tested within the same study, lead to significant errors assigning the weight of each article.62
One of the strengths of this paper is the inclusion of articles in Spanish, Portuguese and English, which are the main languages used in Central and South America. Of the total of 376 articles found, only 12 articles that seemed appropriate for this review according to their titles and abstracts could not be included because we were unable to obtain access to their printed versions.
According to our review, food allergy in Latin America seems to have points in common with studies in other regions but also distinctive features, especially with the frequency of sensitization to some fruits and vegetables. Studies with provocation tests are required to confirm the clinical relevance of these sensitizations.
From this review we can detect different fields that should be evaluated in the coming years in the study of food allergies in Latin America: it is necessary to carry out multicentre studies using the same methodology and the same panel, including a large number of fruits, vegetables and other foods of each region in Latin America.63 The impact of food allergies in other diseases different to asthma, rhinitis and dermatitis should be studied as well as the mechanisms of non-IgE mediated sensitization, and exposure to sunlight and socioeconomic conditions as risk or protective factors of food sensitization.
The almost universal penetration of Internet as a method of communication and easy access to most scientific publications creates an appropriate environment for the development of multicentre research. In fact, these media allow the creation of electronic platforms which we can use to provide patient education and support groups for the management of food allergies. In Latin America, Argentina had a website that provides information and recipes to families with food allergic patients (www.alergialimentaria.org).
In conclusion, this review show a need for further studies on food allergy in Latin America as their regional characteristics provide a different behaviour and different food sensitization pattern to that observed in Europe and the United States. Furthermore, these results must be translated into educational measures for health providers and patients.
Conflicts of interestWe declare no conflict of interest.
Ethical disclosuresConfidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
We would like to thank allergy and immunology societies in Mexico, Brazil and Argentina, who through their websites provide free access to articles from various Latin American journals facilitating the dissemination of scientific publications.