Anaphylaxis is the most severe of all allergic reactions and can even prove fatal. There is limited evidence of a difference in prescribing patterns for self-injectable epinephrine (SIE) between general paediatricians and paediatricians with greater knowledge of allergology.
ObjectivesAssess knowledge about prescribing SIE of a sample of primary care/hospital paediatricians and paediatricians with specialised knowledge of allergology through a questionnaire asking them about clinical cases of anaphylaxis in their daily paediatric practice.
Materials and methodsParticipants were primary care and hospital paediatricians practicing in different regions of the province of Barcelona and paediatricians with specialised knowledge in the field of allergology from Spain.
ResultsA total of 183 paediatricians responded. Of that 59.6% were paediatricians with specialised knowledge of allergology. General paediatricians in most cases correctly prescribed SIE device (more than 70% answered correctly in five of the eight clinical cases). In the case of drug anaphylaxis, which is an avoidable allergen for which SIE is not indicated, 67.5% of general paediatricians would prescribe it. In the case of exercise-induced anaphylaxis there were also differences in the prescription of epinephrine by general paediatricians, with only 40% prescribing it.
ConclusionsIn this study the percentage of SIE prescriptions would be higher than expected by general paediatricians, with no differences in the cases proposed between them and the paediatricians with better knowledge of allergology.
Despite these results, it is important to insist on conducting education programmes and disseminating them to facilitate physicians’ recognition and treatment of anaphylactic reactions.
Anaphylaxis is a severe systemic allergic reaction of rapid onset that is potentially fatal. Heterogeneity in the clinical signs and symptoms is one reason that the actual frequency of anaphylactic reactions is unknown and probably underestimated because many cases go undiagnosed and/or unreported.1 Overall prevalence is estimated from 0.05 to 2%, with incidence thought to be increasing, particularly in children and adolescents. According to the Spanish Alergológica 2005 study (a study analysing epidemiological, clinical and socioeconomic factors of allergic diseases in patients consulting for the first time in an allergology department in 2005), 14.5% of the population under 14 years were allergic to foods (the most common cause of anaphylaxis in children). A total of 66% of these children had been referred to the specialist through the paediatrician, 20.3% by the primary care physician, and only 6.8% by other specialists. Of these patients, 48.5% had required assistance in emergency care due to allergic symptoms. It should be noted that 10.5% of food-allergic children had had an anaphylactic reaction.2 An Australian study in children found a prevalence of 1 per 1000 A&E visits to be due to anaphylactic reaction, with associated triggers recognised in only 68.4% of them.3
Although anaphylaxis is a relatively common condition, little is known about the knowledge among the healthcare professionals involved in the care of patients at risk of anaphylaxis. A review of the literature published in Allergy in April 2010, which included studies addressing outcome in knowledge, education, management and quality of life regarding anaphylaxis revealed deficiencies in the management of anaphylaxis at the medical level, as well as among patients and the community.4
Materials and methodsThe study population consisted of 183 paediatricians, 109 of them (59.6%) with specialised knowledge in the field of allergology and 74 general paediatricians in the public health system as well as hospital care and private health facilities in various regions of the province of Barcelona.
A clinical case-based questionnaire was designed by a paediatrician specialising in allergology and an allergist to assess knowledge about prescribing self-injectable epinephrine (SIE) in the treatment of anaphylaxis. The survey instrument was presented to participants in a clinical session in each of the facilities during the months of May and June of 2013.
Assessment of the responses was based on the opinion of the experts who conducted the survey, relying on the published literature.
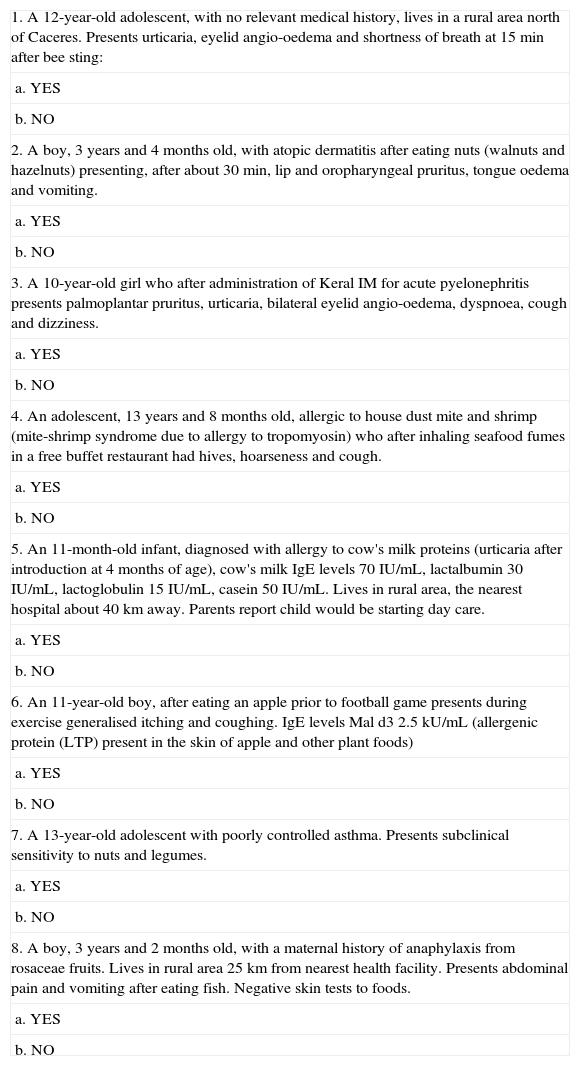
The questionnaire posed eight clinical cases, each of which reflected a situation in which prescribing SIE would be indicated or not for the patient, once assessed by the physician. It presented different clinical cases: an infant, four children and three cases of adolescents. Regarding triggers, there was a case of allergy to hymenoptera venom, a case of adverse reaction to drugs, five cases of adverse reaction to food and a case of exercise-induced food-dependent anaphylaxis. In all cases there were only two possible answers (yes or no) (Table 1).
Questionnaire.
| 1. A 12-year-old adolescent, with no relevant medical history, lives in a rural area north of Caceres. Presents urticaria, eyelid angio-oedema and shortness of breath at 15min after bee sting: |
| a. YES |
| b. NO |
| 2. A boy, 3 years and 4 months old, with atopic dermatitis after eating nuts (walnuts and hazelnuts) presenting, after about 30min, lip and oropharyngeal pruritus, tongue oedema and vomiting. |
| a. YES |
| b. NO |
| 3. A 10-year-old girl who after administration of Keral IM for acute pyelonephritis presents palmoplantar pruritus, urticaria, bilateral eyelid angio-oedema, dyspnoea, cough and dizziness. |
| a. YES |
| b. NO |
| 4. An adolescent, 13 years and 8 months old, allergic to house dust mite and shrimp (mite-shrimp syndrome due to allergy to tropomyosin) who after inhaling seafood fumes in a free buffet restaurant had hives, hoarseness and cough. |
| a. YES |
| b. NO |
| 5. An 11-month-old infant, diagnosed with allergy to cow's milk proteins (urticaria after introduction at 4 months of age), cow's milk IgE levels 70IU/mL, lactalbumin 30IU/mL, lactoglobulin 15IU/mL, casein 50IU/mL. Lives in rural area, the nearest hospital about 40km away. Parents report child would be starting day care. |
| a. YES |
| b. NO |
| 6. An 11-year-old boy, after eating an apple prior to football game presents during exercise generalised itching and coughing. IgE levels Mal d3 2.5kU/mL (allergenic protein (LTP) present in the skin of apple and other plant foods) |
| a. YES |
| b. NO |
| 7. A 13-year-old adolescent with poorly controlled asthma. Presents subclinical sensitivity to nuts and legumes. |
| a. YES |
| b. NO |
| 8. A boy, 3 years and 2 months old, with a maternal history of anaphylaxis from rosaceae fruits. Lives in rural area 25km from nearest health facility. Presents abdominal pain and vomiting after eating fish. Negative skin tests to foods. |
| a. YES |
| b. NO |
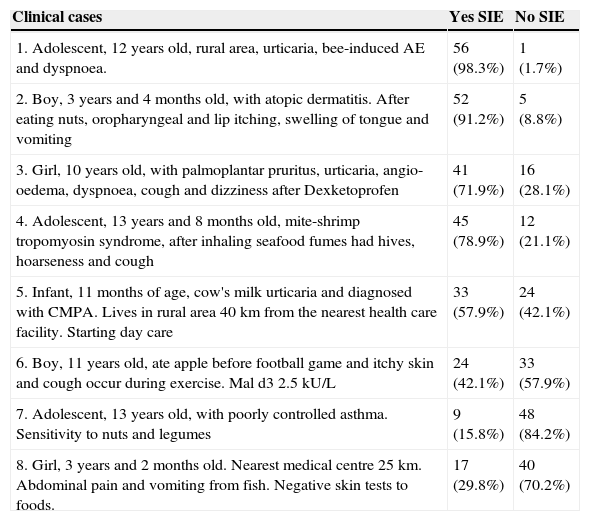
A total of 183 paediatricians responded to the survey, 59.6% of whom are paediatricians with specialised knowledge in allergology. Of the 74 general paediatricians who participated (40.4%), 57 (77%) also worked emergency services shifts (Tables 2 and 3).
Responses of the 57 general paediatricians working emergency services shifts.
| Clinical cases | Yes SIE | No SIE |
|---|---|---|
| 1. Adolescent, 12 years old, rural area, urticaria, bee-induced AE and dyspnoea. | 56 (98.3%) | 1 (1.7%) |
| 2. Boy, 3 years and 4 months old, with atopic dermatitis. After eating nuts, oropharyngeal and lip itching, swelling of tongue and vomiting | 52 (91.2%) | 5 (8.8%) |
| 3. Girl, 10 years old, with palmoplantar pruritus, urticaria, angio-oedema, dyspnoea, cough and dizziness after Dexketoprofen | 41 (71.9%) | 16 (28.1%) |
| 4. Adolescent, 13 years and 8 months old, mite-shrimp tropomyosin syndrome, after inhaling seafood fumes had hives, hoarseness and cough | 45 (78.9%) | 12 (21.1%) |
| 5. Infant, 11 months of age, cow's milk urticaria and diagnosed with CMPA. Lives in rural area 40km from the nearest health care facility. Starting day care | 33 (57.9%) | 24 (42.1%) |
| 6. Boy, 11 years old, ate apple before football game and itchy skin and cough occur during exercise. Mal d3 2.5kU/L | 24 (42.1%) | 33 (57.9%) |
| 7. Adolescent, 13 years old, with poorly controlled asthma. Sensitivity to nuts and legumes | 9 (15.8%) | 48 (84.2%) |
| 8. Girl, 3 years and 2 months old. Nearest medical centre 25km. Abdominal pain and vomiting from fish. Negative skin tests to foods. | 17 (29.8%) | 40 (70.2%) |
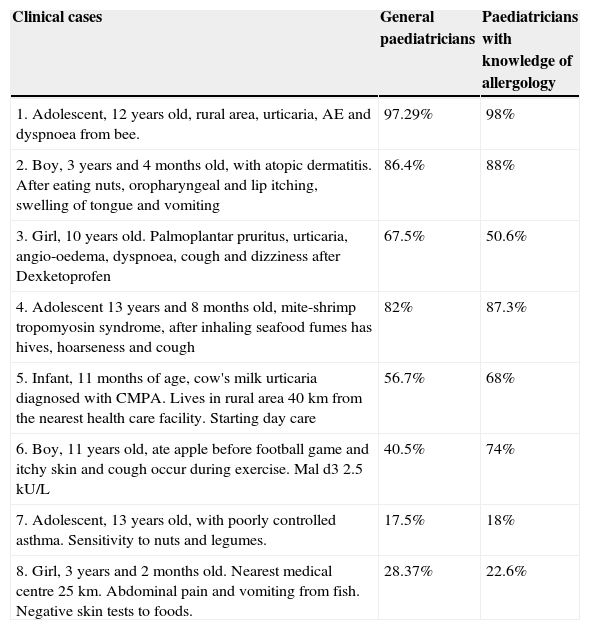
Percentage of primary care/hospital care physicians and specialised doctors who would prescribe self-injectable epinephrine in the different cases.
| Clinical cases | General paediatricians | Paediatricians with knowledge of allergology |
|---|---|---|
| 1. Adolescent, 12 years old, rural area, urticaria, AE and dyspnoea from bee. | 97.29% | 98% |
| 2. Boy, 3 years and 4 months old, with atopic dermatitis. After eating nuts, oropharyngeal and lip itching, swelling of tongue and vomiting | 86.4% | 88% |
| 3. Girl, 10 years old. Palmoplantar pruritus, urticaria, angio-oedema, dyspnoea, cough and dizziness after Dexketoprofen | 67.5% | 50.6% |
| 4. Adolescent 13 years and 8 months old, mite-shrimp tropomyosin syndrome, after inhaling seafood fumes has hives, hoarseness and cough | 82% | 87.3% |
| 5. Infant, 11 months of age, cow's milk urticaria diagnosed with CMPA. Lives in rural area 40km from the nearest health care facility. Starting day care | 56.7% | 68% |
| 6. Boy, 11 years old, ate apple before football game and itchy skin and cough occur during exercise. Mal d3 2.5kU/L | 40.5% | 74% |
| 7. Adolescent, 13 years old, with poorly controlled asthma. Sensitivity to nuts and legumes. | 17.5% | 18% |
| 8. Girl, 3 years and 2 months old. Nearest medical centre 25km. Abdominal pain and vomiting from fish. Negative skin tests to foods. | 28.37% | 22.6% |
Following the recommendations of the EAACI, after an episode of anaphylaxis from hymenoptera insect sting there would be an absolute indication for prescription of SIE.6 In all, 97% of paediatricians and 98% of specialists in allergology would correctly prescribe the device. In the case of poison anaphylaxis, food anaphylaxis (nuts, shellfish, etc.) there is also absolute indication for SIE. A total of 84% of paediatricians and 88% specialists said they would prescribe SIE in such cases. In the case of food allergy, particularly exercise-induced anaphylaxis, SIE should be prescribed. In this case only 40.5% of paediatricians chose it as opposed to 74% of specialists. In cases of subclinical sensitivity to foods with no history of reaction, in non-IgE mediated food hypersensitivity reactions and/or anaphylaxis, SIE prescription drugs are not indicated. A high percentage of paediatricians, both general and specialists, would prescribe SIE (67.5% and 50.6%, respectively) after a drug anaphylaxis (question 3). In the case of IgE-mediated non-anaphylactic hypersensitivity reactions and medical facilities far from the residence SIE should be prescribed depending on the risk-benefit assessment of delay in its administration. In these cases, as shown in question 5 (nearest hospital is 40km away and infant with urticaria due to cow's milk protein allergy), only 56.7% of paediatricians and 68% of specialists would recommend having SIE in the family home.
DiscussionThere is no universally accepted definition of anaphylaxis nor clear criteria for its diagnosis, which often leads to confusion in treatment.5 This is because there are numerous clinical signs and symptoms present in an anaphylactic reaction that may vary between different patients and even between episodes in the same patient. The EAACI defines anaphylaxis as a severe generalised or systemic hypersensitivity reaction, potentially fatal, characterised by the rapid development of potentially fatal problems of the airways and/or circulation, usually accompanied by changes in the skin and/or mucous membranes.6 Furthermore, these symptoms and signs that appear in anaphylaxis may be present in other conditions which must be taken into account when considering a differential diagnosis (acute urticaria, vasovagal syncope, foreign body aspiration, septic shock, etc.).7
The emergency management of anaphylaxis is based on early diagnosis, which is primarily clinical. Intramuscular epinephrine is the first-line treatment in cases of anaphylaxis.8 By definition, at least two systems of the organism must be simultaneously involved in this syndrome. Mucocutaneous involvement is the most common sign, although it may be absent in 20% of patients. Next are the respiratory tract, the gastrointestinal tract and the cardiovascular system.4 In children, respiratory and digestive symptoms are predominant at a similar rate and are also most commonly associated with each other.5
Foods and drugs are the most common causes of anaphylaxis in children and adults, respectively. We should note that the paediatric population has risk factors for severe anaphylaxis. These include adolescence and the coexistence of asthma and food allergy.9,10
Although most paediatricians acknowledge reading guidelines for the diagnosis and treatment of anaphylaxis, there are no clear criteria indicating SIE (see modified algorithm) which is associated with a deficit of prescriptions in cases in which it would be indicated.8 In addition, there is a low level of knowledge among parents of children at risk of anaphylaxis as well as among paediatricians themselves as to how to use the SIE device, so mistakes are made when using it.11,12
Primary care physicians, family doctors, paediatricians and emergency physicians must be aware of the need for all patients who have had anaphylactic reactions to be assessed and, in most cases, monitored by an allergy specialist. It is important that they be familiar with the SIE, that they know when to prescribe it and how it works and that they understand that it is essential for these patients.
Anaphylaxis often occurs in the absence of community healthcare professionals. Prompt administration of self-injectable epinephrine is the initial treatment of choice in the context of a personalised emergency action plan that is key to survival. There are large differences in the rate of use of self-injectable epinephrine in different EU countries. These differences are greater when compared with the United States and Canada. It is possible that this difference is explained by the different criteria for prescribing it that are followed in each country.13,14 In Spain, indication of SIE, according to the summary of product characteristics for marketed devices, is limited to patients who suffer or have presented anaphylaxis, while in other countries, patients at risk of an anaphylactic reaction are also included.
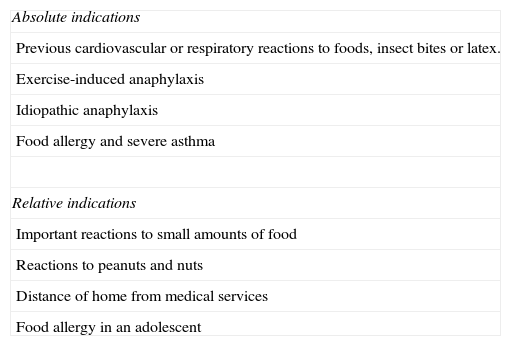
In 2007, the EAACI published a position paper in the Allergy journal which included absolute and relative criteria for the prescription of SIE.6
There are four absolute indications for a self-injectable epinephrine device (Table 4): one previous cardiovascular or respiratory reaction to a food, insect bite or allergy to latex; exercise-induced anaphylaxis; idiopathic anaphylaxis and coexistent persistent asthma in children with food allergies. This latter indication is extrapolated from data arising from retrospective studies. Prospective studies are needed to better define the severity and control of asthma associated with an increased risk of anaphylaxis in food allergic children. The indications are a history of even a mild reaction to peanuts or nuts; any reaction to small amounts of food including food allergen inhalation and/or dermal contact; those patients who live far from a medical facility and allergic reactions to foods in adolescents. Isolated atopic dermatitis and oral allergy syndrome induced by food do not justify the prescription of auto-injectable epinephrine device.
Indications for self-injectable epinephrine.6
| Absolute indications |
| Previous cardiovascular or respiratory reactions to foods, insect bites or latex. |
| Exercise-induced anaphylaxis |
| Idiopathic anaphylaxis |
| Food allergy and severe asthma |
| Relative indications |
| Important reactions to small amounts of food |
| Reactions to peanuts and nuts |
| Distance of home from medical services |
| Food allergy in an adolescent |
Although self-injectable epinephrine can be life-saving, excessive prescribing could be potentially harmful. It is easy to speculate that if all children with food allergy were prescribed, children with increased risk of anaphylaxis may receive less attention. Furthermore, the availability of a self-injectable epinephrine device could encourage children to take less strict avoidance measures.
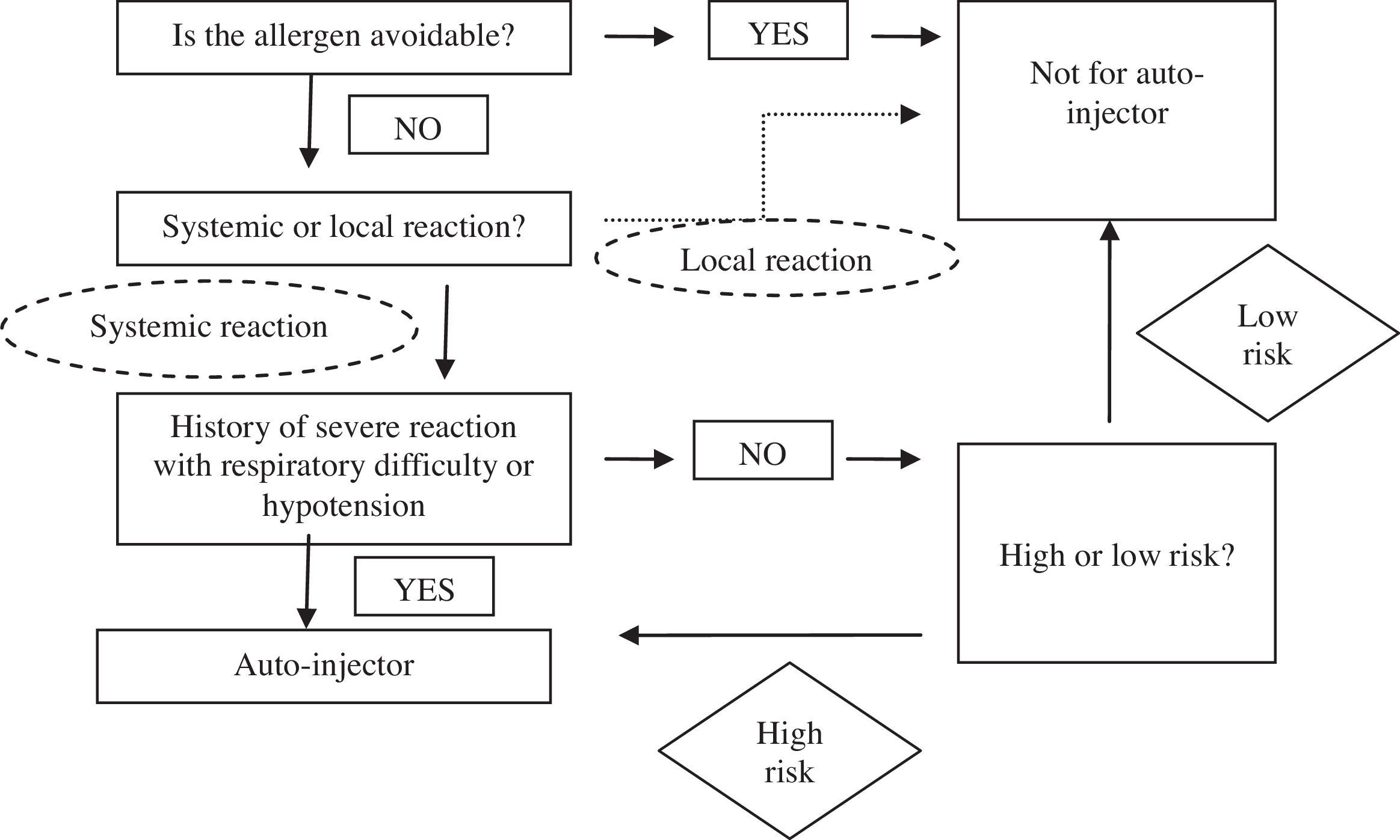
Tools such as the following algorithm could be useful to define which children should be provided with a SIE. This algorithm, based on the MacLean-Tooke algorithm, was modified and presented in the sessions after completion of the survey, as an approach to be followed prior to prescribing SIE.
Adapted McLean-Tooke algorithm8There is a need for greater consensus in the assessment of risk (low/high) of anaphylaxis, key to making a wise decision. Published data suggest that patients considered at-risk should be those with poorly-controlled asthma, with reactions to very small amounts of allergen, those who are allergic to foods such as nuts or shellfish, those who have difficult access to health facilities, those who present systemic mastocytosis, having high total IgE levels, atopic dermatitis and/or children under five years and adolescents.
ConclusionsAlthough published studies indicate that there is a deficit of prescriptions for SIE in cases where it would be indicated, in this study there were no differences in the cases proposed between general paediatricians and paediatricians with more knowledge of allergology in terms of prescribing SIE. Regarding prescribing, it was noted that in certain cases such as drugs anaphylaxis, which is not an indication for SIE, it would be prescribed by more than 50% of both general physicians and those with knowledge of allergology.
General paediatricians, in most cases, properly prescribe the SIE. Although the results are positive, it is only a sample population so we must continue to ensure that healthcare professionals, doctors and nurses disseminate guides and training activities to increase awareness of anaphylaxis as a medical emergency. Knowledge about anaphylaxis among paediatricians and general practitioners should be disseminated because epinephrine is the first line of treatment and the delay in its administration is associated with poor prognosis. We propose the modified algorithm presented as a useful tool in daily practice when prescribing SIE. The way SIE works must be explained to patients who have experienced anaphylaxis and they should always be referred to a consulting allergy specialist to assess each case.
Ethical disclosuresConfidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article
Protection of human subjects and animals in researchThe authors declare that no experiments were performed on humans or animals for this investigation.
Conflict of interestThe authors have no conflict of interest to declare.