Objective. To evaluate the incidence, demographic, clinical and laboratory characteristics of patients with acute viral hepatitis E in Montenegro.
Material and methods.A total of 400 patients with acute viral hepatitis from January 1st, 2000 to December 31st, 2007 were enrolled in the study. Serological tests for hepatitis A, B, C, D, and E viruses, Epstein-Barr virus, cytomegalovirus, and herpes simplex viruses were performed. Standard laboratory tests for liver function were analyzed. The results are presented as absolute numbers, mean ± SD, range of values, and percent. A P value < 0.05 was considered significant.
Results.Twenty-four (6%) patients had clinically and/or serologically confirmed acute hepatitis E. The mean age of the patients was 25 ± 6 years; 62.5% were males. The majority of the patients (66%) belonged to the 20 to 40 yrs age group (P < 0.05). Seven patients were asymptomatic. Foremost symptoms were loss of appetite (100%), fatigue (94%) and vomiting (75%). The most frequent clinical sign was mild to moderate liver enlargement (94%). Jaundice had 12/17 symptomatic patients. Elevation of alanine aminotransferase was found in 19 patients including two patients without symptoms. The enzyme, gamma glutamyltranspeptidase was increased in all patients.
Conclusion.Acute hepatitis E in Montenegro emerges as an autochthonous infection with a low incidence. Sub-clinical and anicteric infections may occur. Elevation of gamma glutamyltranspeptidase is an important parameter of the biochemical profile of the disease.
Hepatitis E virus (HEV) is an enterically transmitted virus characterized as a self-limited disease.1,2 It has many clinical and epidemiological similarities with hepatitis A causing clinical and sub-clinical liver inflammation in humans worldwide, particularly in resource-poor nations.3,4 The reservoir of HEV is unknown, although it is accepted that the virus may be transmitted by animals.5-7 The overall case fatality rate is 4%, while in pregnant women it is from 15-25% during the second and third trimesters.8-10
ObjectiveThe aim of this retrospective study were to evaluate the incidence and demographic, clinical and laboratory characteristics of patients with acute viral hepatitis E in Montenegro.
Material and MethodsFrom January 1st, 2000 to December 31st, 2007, a total of 400 patients with acute viral hepatitis were included in the study. The majority of patients were consecutively hospitalized in the Clinic for Infectious Diseases, Clinical Centre of Montenegro, Podgorica with clinical, biochemical and serological confirmation of the disease. The others were out-patients in close contact (household, sexual, etc.) with hospitalized patients with or without symptoms but elevated aminotransferases at the time of diagnosis of acute hepatitis in the index case. In the later group of patients, serological diagnosis was performed for acute hepatitis B and C while hepatitis A was mostly diagnosed using biochemical and epidemiological data. Acute viral hepatitis A, B and C was defined according to CDC definition.11,12 Additional analysis was done on patients negative for acute hepatitis A, B and C serological markers that further were tested for acute hepatitis D (in a risk group patients) and E. Extra blood samples were collected and tested for immune globulin class M anti-hepatitis E virus (IgM anti-HEV) from all family contacts of hospitalized HEV infected patients (17 families, 72 persons) for over a period of 30 ± 15 days after the diagnosis of the index case. Other acute hepatitis A, B, C, D and E negative persons were tested for Epstein-Barr virus, cytomegalovirus, and herpes simplex virus acute infection.
In patients, a complete medical history was taken, the upper abdomen was examined by ultrasound and standard hematological and biochemical liver function tests were performed. Viral serological analyses were made with commercial immunoassay kits for hepatitis A, B, C and D viruses, EpsteinBarr virus, cytomegalovirus, and herpes simplex viruses 1 an 2 (BioRad ELISA; Ortho EIA). IgM anti-HEV was detected by enzyme linked immunosorbent assay (ELISA) with Mexican and Burma virus strains (EIAgen HEV IgM, Adaltis Inc., Montreal, Canada; HEV IgM, DIA. PRO, Milano, Italy). Both tests have high specificity and sensitivity (98%).
For statistical analysis of parametric and non-parametric variables, the electronic data base organized in the Statistical Package for Social Science (SPSS) for Windows (version 11.0) was used. A P value < 0.05 was considered significant. The results are presented as absolute numbers, mean ± SD, range of values, and percent.
ResultsThe mean age of the patients was 25 ± 6 yrs; ranging from 6 to 48 yrs. The majority of the patients (66%) belonged to the 20 to 40 yrs age group (P < 0.05). Males vs. females were 62.5% and 37.5%, respectively (P > 0.05).
Among the 400 patients, acute hepatitis E was clinically and/or serologically confirmed with positive IgM anti-HEV in total of 24 (6%) individuals. Hepatitis B virus surface antigen (HBsAg was) positive but immune globulin class M anti-hepatitis B core antigen (IgM anti-HBc) was negative in two of them and these patients were diagnosed as acute HEV superinfection in HBV carriers.
There were 7/24 (29.1%) out-patients with sub-clinical (without symptoms and/or jaundice) infection confirmed with positive IgM anti-HEV. These patients had close (familiar) contact with acute hepatitis E index case. The overall incidence of acute hepatitis E with history of family contact was found in 9.7% (7/72) of patients. Among them, four patients belonged to the same family, while the other three patients were members of three different families.
Analysis of social-epidemiological data showed a significantly low frequency of patients having risks for acquiring infection in the context of their behavior (intravenous drug user, one patient; prostitute, one patient; men having sex with men, two patients), or history of traveling abroad (Albania, one patient; Germany, one patient; U.S., two patients; Bosnia and Herzegovina, two patients). The majority of patients had a central type of water supply and sewage drainage. One patient owned pigs, but he others had no contact with domestic or wild animals.
Concerning clinical symptoms and signs, all hospitalized patients had loss of appetite. The majority of the patients (94%) showed fatigue and 74% of patients vomited. Abdominal pain was not notably reported. The majority of patients had mild to moderate liver enlargement (94%). Spleen enlargement and hemorrhagic syndrome was present in minority of patients (35% and 6%, respectively). In general, clinical course of the disease was mild to moderate. Prolonged prothrombin time (18 seconds) in one patient was not followed with other sings of liver insufficiency (hepatic encephalopathy or coagulopathy) and returned to normal value after administration of K vitamin. Two patients diagnosed as HEV superinfection in hepatitis B virus carriers did not show a difference in clinical presentation or biochemical parameters in comparison with other patients. Recovery of all patients was complete up to 65 days of the illness.
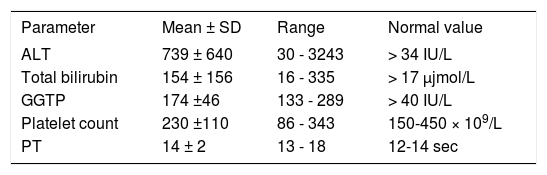
Values of laboratory parameters in patients with acute hepatitis E are presented in table 1.
Values of laboratory parameters in the patients with acute hepatitis E (n = 24).
| Parameter | Mean ± SD | Range | Normal value |
|---|---|---|---|
| ALT | 739 ± 640 | 30 - 3243 | > 34 IU/L |
| Total bilirubin | 154 ± 156 | 16 - 335 | > 17 μjmol/L |
| GGTP | 174 ±46 | 133 - 289 | > 40 IU/L |
| Platelet count | 230 ±110 | 86 - 343 | 150-450 × 109/L |
| PT | 14 ± 2 | 13 - 18 | 12-14 sec |
ALT: Alanine aminotransferase. GGTP: Gamma glutamyltranspeptidase. PT: Prothrombin time.
An increase of serum alanine aminotransferase (ALT) activity was evident in the majority of patients (79.2%). Among them, two patients had sub-clinical infection, others were all hospitalized patients. Total serum bilirubin was elevated in 12 symptomatic patients (70.6%). Gamma glutamyl-transpeptidase (GGTP) was increased in more than three-fold the normal value in all patients, while this enzyme was four times than normal value in 7/ 17 symptomatic patients and in 2/7 asymptomatic patients. Regression analysis did not show the absolute value or four-fold elevation of GGTP as significant predictor factors for symptomatic or asymptomatic patients (P = 0.531 and P = 0.409, respectively).
DiscussionThis is our first investigation about the incidence of hepatitis E in Montenegro. Data of 400 hospitalized and out-patients patients with acute viral hepatitis showed that 24 (6%) of them had acute hepatitis E. This result illustrates the emergence of hepatitis E in Montenegro, although with a low incidence.
Concerning social-demographic data of these patients, we found that males were more numerous (62.5%) than females (37.5%) although without of statistical difference. Similar investigations regarding to the HEV infection from neighboring Serbia also revealed that this infection rate among the male population was significantly higher than in females.13
The age of the patients varied extremely. The youngest was a 6 year-old child, while the oldest was 48 years old. Analysis of ages showed the highest frequency of patients in the group aged from 20-40 yrs (66%). Other authors also reported the highest frequency of patients with hepatitis E in this age group.1,4 This finding can be explained by the possibility of persistence of abundant mature receptors on hepatocytes for the virus in adults.
Epidemiologic data showed that the majority of patients had never traveled out of the country. Only seven (29.2%) patients had returned from other than high-endemic countries at least six months before the illness. These data indicate non-travel related HEV as the autochthonous virus in Montenegro. Furthermore, autochthonous infections of HEV were previously reported in our neighborhood (Serbia and Greece).13,14 Additionally, the emergence of accidental non-travel related hepatitis E was also reported from other European countries.15-18
In our cohort, the absence of contact with domestic or wild animals, with exception in one patient, can exclude zoonotic spread of HEV infection as a possible mode of transmission. Serological evidence of asymptomatic patients with acute hepatitis E in families with patients with clinical symptoms may indicate simultaneously infection or possible person-to-person transmission, although later is not common in sporadic hepatitis E.19 In addition to epidemiological data, there was little evidence that some bizarre behavior (e.g. intravenous drug abuse or multiple sexual partners) or blood transfusion was associated with HEV transmission as was reported by some authors.20,21
Clinical features of hepatitis E in our patients did not differ from viral hepatitis of other etiologies in general. The persistence of established chronic liver disease (although in only two patients with chronic hepatitis B virus infection) did not influence the clinical course. After more than two months of follow-up, the infection was self-limited with no clinical or laboratory evidence of chronic hepatitis. It is intriguing that recent studies reported the persistence of chronic HEV infection related to marked immunosuppression.22,23
An asymptomatic form of the disease was serologically confirmed in 7/24 patients indicating that hepatitis E can resolve as an unrecognized infection almost in one third of cases. The mild form or short course of sub-clinical disease can explain normalization of ALT activity in 5/7 patients without symptoms before disappearance of IgM anti-HEV lasting a few months more.1,24 Elevation of GGTP in all patients without differences related to clinical features (sub-clinical vs. clinical cases) points to this enzyme as an important biochemical parameter for acute hepatitis E. The reason for elevation of GGTP in hepatitis E could be infection of the pancreas or bile duct cells with this virus but this is still controversial.
In conclusion, our investigation shows that acute hepatitis E in Montenegro emerges as an autochthonous infection with a low incidence. Clinical features of HEV infection are similar to those of other acute viral hepatitis. Sub-clinical of the disease may occur. Elevation of GGTP is important biochemical parameter of the disease and is independent of the clinical course. However, the mode of transmission remains to be resolved.
Abbreviations- •
HEV: Hepatitis E virus.
- •
IgM anti-HEV. Immune globulin class M antihepatitis E virus.
- •
ELISA. Enzyme linked immunosorbent assay.
- •
HBsAg. Hepatitis B virus surface antigen.
- •
IgM anti-HBc. Immune globulin class M antihepatitis B core antigen.
- •
ALT. Alanine aminotransferase.
- •
GGTP. Gamma glutamyltranspeptidase.