Introduction. Hepatocellular carcinoma is the most common primary tumor of the liver and is diagnosed in more than a half million people worldwide each year. This study aims to assess factors associated with the recurrence and survival of patients with hepatocellular carcinoma and liver transplantation in a cohort of patients from Medellín, Colombia.
Material and methods. This was a descriptive retrospective study of a consecutive series of liver transplant patients from the Pablo Tobon Uribe Hospital of Medellín from January 2004 to May 2013. Demographic, clinical, imaging, and pathology variables were analyzed.
Results. Three hundred thirty liver transplants were performed during the study period, 54 cases (16.4%) had one or more hepatocellular carcinomas in the explant, and 79.6% of these patients were men. Cirrhotic patients had different etiologies, but most of them were due to alcohol abuse (22.2%), followed by hepatitis B virus infection (20.4 %), and hepatitis C virus infection (18.5%). In the pathology specimen, 51.9% had only one focus of hepatocellular carcinoma, 22.2% had two foci and 12.9% had three tumors. Recurrence of hepatocellular carcinoma occurred in 7.4% patients with an average time of 81 months. During follow-up, 25.9% of the patients died in an average time of 67.9 months (CI95 59.1-80.1 months).
Conclusion. Recurrence and survival of patients with liver transplantation for hepatocellular carcinoma in this study had a similar behavior as that reported in the world literature. The factors associated with these outcomes were vascular invasion, poor tumor differentiation and satellitosis.
Hepatocellular carcinoma (HCC) is current public health problem, as it is the most common primary tumor of the liver, and it most often occurs in patients with liver cirrhosis.1 HCC is diagnosed in more than a half million people worldwide each year, is the fifth most common tumor in men and is the seventh most common tumor in women.2 Its frequency varies widely according to geographic location and distribution, and there is often a different prevalence between ethnic groups and even between regions within the same country. For Colombia in particular, an incidence of 2 cases per 100,000 is estimated.3,4
This tumor is presented in 80 to 90% of the cases in patients with liver cirrhosis, mainly associated with hepatitis C virus, hepatitis B virus, and alcohol abuse; less frequently, HCC is found when cirrhosis is due to hereditary hemochromatosis, Wilson’s disease or autoimmune disease.1
HCC was an indication for liver transplantation almost indiscriminately in the 1970s and early 1980s, but then it was virtually contraindicated in the mid-1980s due to poor survival and high recurrence rate. However, the seminal publication of Mazzaferro in 1996 showed similar survival rates between patients transplanted with HCC and those in patients who were transplanted without HCC (75% at 4 years); his HCC group had several strict criteria: one tumor of 5 cm or less or three tumors, each of them less than 3 cm. Since then, these criteria for liver transplants in cases of HCC have been known as the Milan criteria.5–7
The most important factors associated with recurrence and survival after liver transplantation are the levels of alpha-fetoprotein (AFP) prior to transplantation, tumor size, tumor differentiation, vascular invasion, and macroscopic and microscopic presence of satellitosis.8–12
To the best of our knowledge, few Latin American studies have addressed this specific issue of liver transplantation and HCC, perhaps due to the poor development in this field in different countries. Only Brazil, Argentina, Colombia, and Mexico have solid transplant groups with a significant number o f transplants per year. In Colombia, for example, no strong data are available with reports and statistics about liver cancer, considering that there are few groups with few annual procedures (less than 50 liver transplants per year on average for each group).13–16 In this study, the survival of liver transplant patients with HCC was analyzed to try to define what prognostic factors may determine survival and recurrence in a group of patients in Medellín, Colombia.
Material and MethodsAn observational, descriptive study with survival analysis was performed, using secondary sources of information (medical records and data base), in which the recurrence and survival of patients with HCC transplanted in the Hospital Pablo Tobon Uribe, Medellín, were analyzed from April 1, 2004 until May 31, 2013.
The study population consisted of all records of liver transplant patients in the Pablo Tobón Uribe Hospital in whom a HCC was found in the explant. The diagnostic criteria for HCC were based on the American Association for the Study of Liver Diseases and European Association for the Study of the Liver guidelines. The patients were followed every month for the first six months, then every two months for the next six months, and then every three months.
The exclusion criteria were patients under 18 years old, and the lack of information in the clinical register for get all the data that were needed.
Between April 1, 2004 and May 31, 2013, 330 liver transplants in adult patients (18 years or more) were performed in the Pablo Tobon Uribe Hospital. All of the livers were from cadaveric donors. The presence of HCC was confirmed in 54 cases (16.4%), and in 9 patients (2.7%) HCC was an incidental finding.
Statistical analysisFor the analysis, the following variables were recorded: demographics (age, sex), clinical (etiology of cirrhosis, previous complications), biochemical (alpha-fetoprotein levels), imaging (CT scan and MRI findings), and histopathology (number and size of tumors, vascular invasion, and cell differentiation). All of these were the independent variables; the dependent variables were recurrence and death.
For the univariate statistical analysis, frequency measures of central tendency are described. In addition, the survival analysis with Kaplan Meier was calculated, and recurrence and survival were also estimated. In the bivariate analysis, the Log Rank test was used, and the value of statistical significance was considered at p < 0.05.
For the multivariate analysis, to determine the factors that best explain tumor recurrence and patient survival, the Hosmer-Lemeshow criteria with p ≤ 0.25 in the bivariate analysis were used. Then, a Cox regression analysis was performed; first, the crude hazard ratio was calculated and then adjusted to determine the change in the measure of association. The value of significance accepted was p < 0.05. The statistical analysis was performed using SPSS version 21(Statistical Package for the Social Sciences Inc.; Chicago, Illinois, USA).
ResultsOf the 54 cases with liver transplant and HCC, 79.6% were men. The median age of all the HCC patients was 58 years (IR 51-62 years). The most frequent etiology of cirrhosis was alcohol abuse (22.2%), followed by hepatitis B infection (20.4%), hepatitis C infection (18.5%), and others (33.3%). The AFP (ks = 0.393, P = 0.000) had a median of 11 ng/mL (IR 4.9 to 81.5 ng/mL). The waiting time for transplantation (ks = 0.203, P = 0.000) had a median of 28 days (IR 15-44).
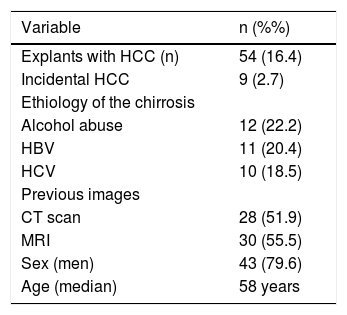
The imaging techniques that were used before the liver transplant were CT scan in 28 patients and MRI in 30 patients. Vascular invasion in the explant was found in 27.9% of cases (15 patients), all with tumors of 3 cm or more, and satellitosis was found in 14.8% (8 patients); and all of the tumors measured 2.5 cm or more. In 38 cases (70.4%), the tumor was well differentiated and of variable size, 12 patients (22.2%) had moderately differentiated tumors also of different sizes, and in 2 cases (3.7%), poorly differentiated tumors and complete necrosis of the tumor were found (Table 1).
Characteristics of the patients with liver transplantation for hepatocellular carcinoma. HPTU, 2004-2012.
| Variable | n (%%) |
|---|---|
| Explants with HCC (n) | 54 (16.4) |
| Incidental HCC | 9 (2.7) |
| Ethiology of the chirrosis | |
| Alcohol abuse | 12 (22.2) |
| HBV | 11 (20.4) |
| HCV | 10 (18.5) |
| Previous images | |
| CT scan | 28 (51.9) |
| MRI | 30 (55.5) |
| Sex (men) | 43 (79.6) |
| Age (median) | 58 years |
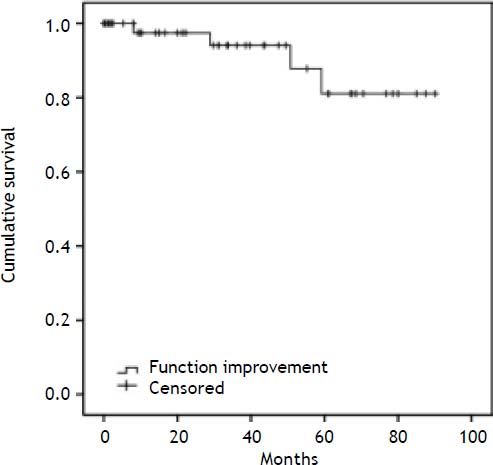
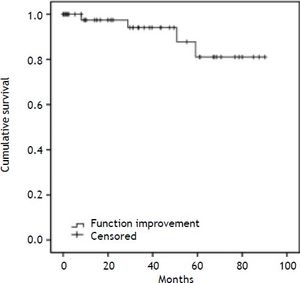
Recurrence of HCC occurred during the follow-up study in four patients (7.4%) in an average time of 81 months, ranging between 73.5 and 89.2 months; the possibility of being free of recurrence at eight months was 97.4%, at two years was 94.1% and at 5 years was 81.1% (Figure 1).
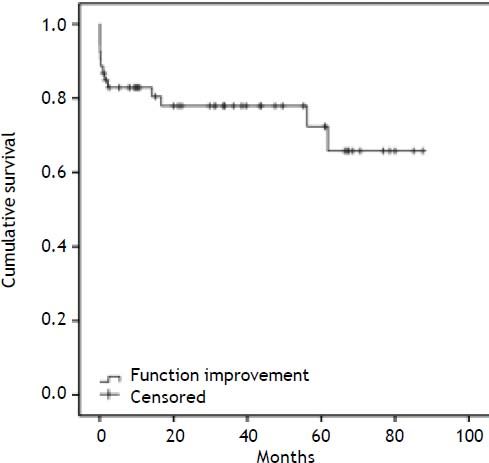
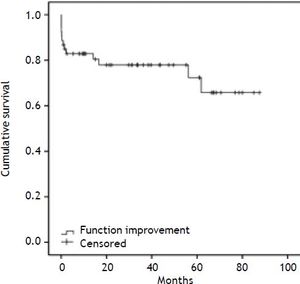
Fourteen patients died during follow-up (25.9%) in an average time of 67.9 months. The likelihood of survival in the first year was 83.2%, in the third year was 78.4%, and in the fifth year was 73.2% (Figure 2).
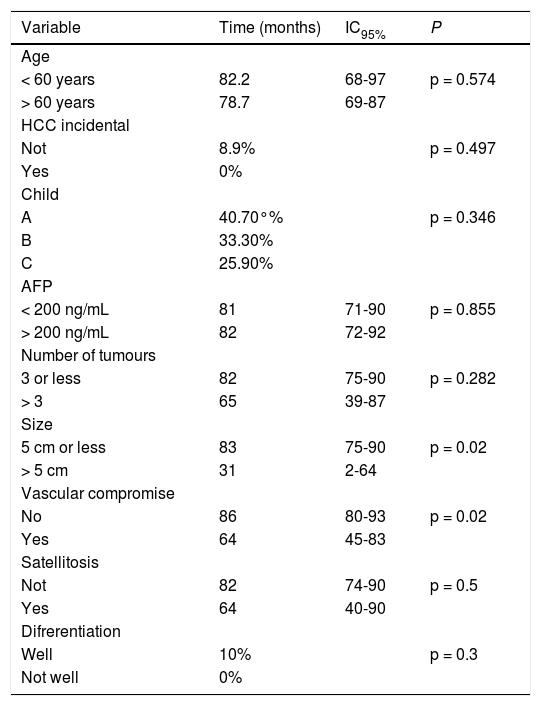
It was found that the variables associated with tumor recurrence were: tumor size (5 cm or more, p = 0.029, and vascular compromise (p = 0.02); there were no variables associated with death in these patients (Tables 2 and 3).
Relationship of demographic, clinical, imaging and pathology of patients with liver transplantation for hepatocellular carcinoma with recurrence. HPTU, 2004-2012.
| Variable | Time (months) | IC95% | P |
|---|---|---|---|
| Age | |||
| < 60 years | 82.2 | 68-97 | p = 0.574 |
| > 60 years | 78.7 | 69-87 | |
| HCC incidental | |||
| Not | 8.9% | p = 0.497 | |
| Yes | 0% | ||
| Child | |||
| A | 40.70°% | p = 0.346 | |
| B | 33.30% | ||
| C | 25.90% | ||
| AFP | |||
| < 200 ng/mL | 81 | 71-90 | p = 0.855 |
| > 200 ng/mL | 82 | 72-92 | |
| Number of tumours | |||
| 3 or less | 82 | 75-90 | p = 0.282 |
| > 3 | 65 | 39-87 | |
| Size | |||
| 5 cm or less | 83 | 75-90 | p = 0.02 |
| > 5 cm | 31 | 2-64 | |
| Vascular compromise | |||
| No | 86 | 80-93 | p = 0.02 |
| Yes | 64 | 45-83 | |
| Satellitosis | |||
| Not | 82 | 74-90 | p = 0.5 |
| Yes | 64 | 40-90 | |
| Difrerentiation | |||
| Well | 10% | p = 0.3 | |
| Not well | 0% |
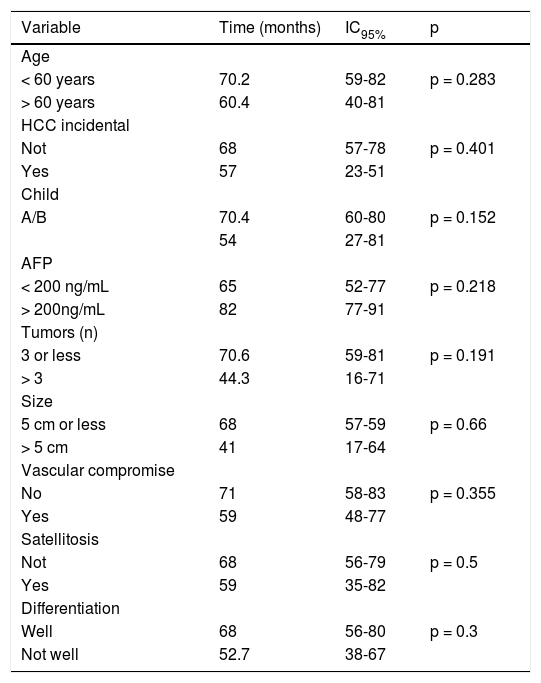
Relationship of demographic, clinical, imaging and pathology death of patients with liver transplantation for hepatocellular carcinoma with death. HPTU, 2004-2012.
| Variable | Time (months) | IC95% | p |
|---|---|---|---|
| Age | |||
| < 60 years | 70.2 | 59-82 | p = 0.283 |
| > 60 years | 60.4 | 40-81 | |
| HCC incidental | |||
| Not | 68 | 57-78 | p = 0.401 |
| Yes | 57 | 23-51 | |
| Child | |||
| A/B | 70.4 | 60-80 | p = 0.152 |
| 54 | 27-81 | ||
| AFP | |||
| < 200 ng/mL | 65 | 52-77 | p = 0.218 |
| > 200ng/mL | 82 | 77-91 | |
| Tumors (n) | |||
| 3 or less | 70.6 | 59-81 | p = 0.191 |
| > 3 | 44.3 | 16-71 | |
| Size | |||
| 5 cm or less | 68 | 57-59 | p = 0.66 |
| > 5 cm | 41 | 17-64 | |
| Vascular compromise | |||
| No | 71 | 58-83 | p = 0.355 |
| Yes | 59 | 48-77 | |
| Satellitosis | |||
| Not | 68 | 56-79 | p = 0.5 |
| Yes | 59 | 35-82 | |
| Differentiation | |||
| Well | 68 | 56-80 | p = 0.3 |
| Not well | 52.7 | 38-67 |
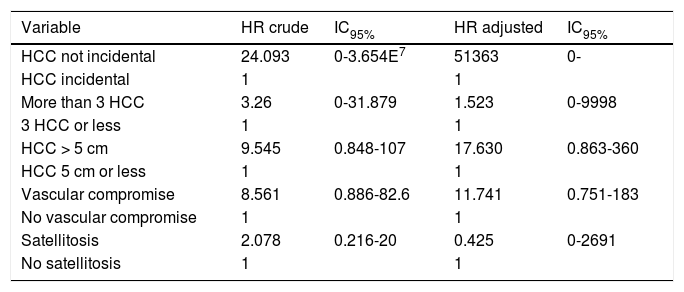
For the multivariate analysis in recurrence, the following variables were included: number of tumors (3 or fewer tumors as cutoff), tumor size (5 cm or less as a cutoff), vascular compromise, and satellitosis in the pathology. The crude hazard ratio for tumor recurrence showed no statistically significant association in any of the variables, but it is noteworthy that recurrence was faster when the pathology showed more than three tumors, when the tumor size was more than 5 cm in diameter, and when there was microscopic vascular involvement. This analysis when adjusted, showed that the variables outlined above are all factors that increase the speed of relapse except satellitosis, but again, none of these variables was statistically significant (Table 4).
Factors related to tumor recurrence in patients with liver transplantation for hepatocellular carcinoma. HPTU, 2004-2012.
| Variable | HR crude | IC95% | HR adjusted | IC95% |
|---|---|---|---|---|
| HCC not incidental | 24.093 | 0-3.654E7 | 51363 | 0- |
| HCC incidental | 1 | 1 | ||
| More than 3 HCC | 3.26 | 0-31.879 | 1.523 | 0-9998 |
| 3 HCC or less | 1 | 1 | ||
| HCC > 5 cm | 9.545 | 0.848-107 | 17.630 | 0.863-360 |
| HCC 5 cm or less | 1 | 1 | ||
| Vascular compromise | 8.561 | 0.886-82.6 | 11.741 | 0.751-183 |
| No vascular compromise | 1 | 1 | ||
| Satellitosis | 2.078 | 0.216-20 | 0.425 | 0-2691 |
| No satellitosis | 1 | 1 |
For the multivariate analysis in survival, the following variables were included: age (cutoff value of 60 years), child score, number of tumors (3 or less), tumor size (5 cm as a cutoff), vascular compromise, satellitosis, and cell differentiation in the final pathology. The crude hazard ratio for survival showed no statistically significant association in any of the variables, but survival was reduced when the age was more than 60 years, the patient was Child C, there were more than three tumors in the explant, the tumor was more than 5 cm in diameter, there was vascular involvement, and with the presence of satellitosis.
This analysis when adjusted, showed that the variables outlined above are all factors that decrease the survival, but again, none of these variables was statistically significant (Table 5).
DiscussionThe most important aspect of this study is that it present epidemiological and demographic data from liver transplant patients in Colombia with HCC as well as insight into HCC progression in terms of recurrence and survival. In a paper published in 2005 on the distribution of HCC by sex in Colombia, the authors found an equal HCC prevalence between men and women;16 however, in the present study, a similar distribution was not observed. Most previous studies show that the HCC incidence is much higher in men than in women with a ratio of up to 4:1. The etiology of the cirrhosis was mainly due to alcohol, or hepatitis B and C virus.
Additionally, another important finding is that AFP had no diagnostic value in the present study, as 50% of patients had levels below 20 ng/mL and only 18.5% cases had values above 200 ng/mL, which is a value used by many international organizations as the cutoff for diagnosis of HCC.
It is important to note the short time on the waiting list, as 50% of the patients waited less than a month on the waiting list; this finding reflects both the opportunity to obtain a liver transplant and also the opportunity to prevent tumor progression. These findings are reported in up to 20% of patients on the transplant list in the world.
The recurrence observed in this study was 7.4% after an average of 81 months; after two years, the probability of being free of recurrence was 94.1% and was 81.1% after five years. The survival of patients was 67.9%; the probability of survival at one year was 83.2%, and at five years it was 73.2%. These findings show more optimistic results than many of the world’s largest series of reference groups, where recurrences are estimated to be between 15 to 20% and five-year survival is estimated to be between 65 to 70%.
The bivariate analysis supports the findings of the World Series, where the most important features in terms of tumor recurrence were the presence of vascular invasion in the pathology and tumor size of more than 5 cm (p < 0.05). Some reports show an increase of up to 15 times the risk of recurrence when vascular invasion is present.17,18 In this study, the increase was 7.5 times, but in the explanatory analysis, this rate increased to 12.3 times compared with those patients who did not have vascular invasion.
The main limitations of this study are the small number of patients studied despite the extended study period, which was due to the high complexity and resultant difficulties in accessing medical services in Colombia. Some of the biases that may been present were monitored in the moment, as was the fact that the liver explants were assessed by two expert pathologists in HCC, and the data collection was only performed by researchers.
ConclusionIn conclusion, in this serie, demographic characteristics and the etiology of HCC was similar to the world literature reports, AFP was also useless in the diagnosis of HCC. The most important factors in recurrence and survival after liver transplant were tumor size more than 5 cm, more than 3 tumors, and vascular compromise. The 5 year survival was similar to that reported in different world series.
Abbreviations- •
AASLD: American Association for the Study of Liver Disease.
- •
AFP: alpha- fetoprotein.
- •
EASL: European Association for the Study of Liver.
- •
HBV: hepatitis B infection.
- •
HCC: hepatocellular carcinoma.
- •
HCV: hepatitis C infection.
Sustainability Project Vicerrectoría Research, Universidad de Antioquía.