Background and rationale for the study. The Model for End Stage Liver Disease (MELD) score has not been derived and validated for the emergent transjugular intrahepatic portosystemic shunt (TIPS) population. We sought to identify predictive factors for survival among emergent TIPS patients, and to substantiate MELD for outcomes prognostication in this population.
Results. 101 patients with acute life threatening variceal hemorrhage underwent emergent TIPS (defined by failed endoscopic therapy for active bleeding, acute hemoglobin drop, ≥ 2-unit transfusion requirement, and/or vasopressor need) at between 1998-2013. Demographic, clinical, laboratory, and procedure parameters were analyzed for correlation with mortality using Cox proportional hazards regression to derive the prognostic value of MELD constituents. Area under receiver operator characteristic (AUROC) curves was used to assess the capability of MELD prediction of mortality. TIPS were created 119 ± 167 h after initial bleeding events. Hemodynamic success was achieved in 90%. Median final portosystemic pressure gradient was 8 mmHg. Variceal rebleeding incidence was 21%. The four original MELD components showed significant correlation with mortality on multivariate Cox regression: baseline bilirubin (regression coefficient 0.366), creatinine (0.621), international normalized ratio (1.111), and liver disease etiology (0.808), validating the MELD system for emergent cases. No other significant predictive parameters were identified. MELD was an excellent predictor of 90-day mortality in the emergent TIPS population (AUROC = 0.842, 95% CI 0.755-0.928).
Conclusions. Based on independent derivation of prognostic constituents and confirmation of predictive accuracy, MELD is a valid and reliable metric for risk stratification and survival projection after emergent TIPS.
The Model for End Stage Liver Disease (MELD) score was developed in 2000 to predict mortality in patients undergoing transjugular intrahepatic portosystemic shunt (TIPS) creation.1 This measure was conceived from data accrued in patients undergoing elective TIPS, and has since proven to be an accurate and robust prognostic metric for pre-procedure patient risk stratification and outcomes estimation after planned TIPS procedures.2–6 Although emergent cases constitute a significant proportion of TIPS procedures performed in contemporary medical practice, the MELD score has not been independently derived and validated for this patient population, and the degree to which this metric is directly translatable for prediction of early clinical outcomes in the emergent TIPS population is uncertain. Given the relative paucity of data evaluating the performance of the MELD score in this setting,7 differences in contributing prognostic factors, extent of parameter influence, and quantitative risk thresholds may exist between emergent and elective cases. To this end, external unbiased derivation and substantiation of the MELD system in the emergent setting is necessary to confirm applicability of this metric to emergent TIPS. With this in mind, we undertook the current investigation with the aim of identifying prognostic factors for early survival among patients undergoing emergent TIPS, confirming the predictive capacity of MELD components in this scenario, and validating the MELD system for use in emergent circumstances, with particular attention to risk assessment.
Material and MethodsThis study was performed with approval from our institutional review board. Patients provided consent for TIPS procedures.
Patients and variceal bleedingTwo hundred ninety five patients who underwent technically successful TIPS procedures between November 1998 and December 2013 at a single tertiary care, university affiliated hospital were identified through review of our Division of Interventional Radiology (IR) TIPS registry for potential retrospective study. Cases of emergent TIPS were selected from the registry, with such cases characterized by active variceal hemorrhage resulting in immediate threat to life and necessitating prompt medical intervention to maintain well-being. These patients were typically initially managed according to clinical practice guidelines of the American Association for the Study of Liver Diseases.8 Treatment encompassed intravascular volume support, blood transfusion, antibiotic prophylaxis, pharmacological therapy with somatostatin or its analogues, and esophagogastroduodenoscopy (EGD) to diagnose varices and treat with endoscopic ligation or sclerotherapy. Non-selective beta-blocker medications were not generally administered in the acute variceal hemorrhage setting. Patients were referred for TIPS in cases where hemorrhage could not be controlled or bleeding recurred despite medical therapy. Emergent cases were defined by failure of endoscopic therapy, hemoglobin drop with a known variceal source of bleeding, required transfusion of ≥ 2 units of packed red blood cells (PRBCs), or need for vasopressor medications to support blood pressure within 24-48 hours prior to TIPS. Cases of elective TIPS (n = 194) were excluded. One hundred one patients who underwent emergent TIPS procedures were thus included in the final study group.
TIPS proceduresTIPS creation was performed according to previously described methods9 using general anesthesia in the IR suite. Right jugular venous access was gained with placement of a 10 French sheath and systemic venous pressure measurement. The right hepatic vein was selected and free and wedged hepatic venography was performed. Next, a RöschUchida transjugular liver access set (Cook Medical Co., Bloomington IN) was used to access the right portal vein. After catheterization and pressure measurement, tract dilation was performed, followed by direct portography. Then, 10 or 12 mm Wallstent bare metal Stents (Boston Scientific, Natick MA) (used from 1998-2003) or 10 mm Viatorr covered stent-grafts (W.L. Gore & Associates, Flagstaff AZ) (used from 2004-2013) were deployed followed by balloon dilation. A final portosystemic pressure gradient was measured, followed by shunt venography. Coil embolization of gastroesophageal varices was performed at the discretion of the primary operator. Following TIPS procedures, patients underwent inpatient monitoring with daily acquisition of liver enzymes. Upon hospital discharge, patients were followed in an outpatient Hepatology clinic. Following TIPS, patients were monitored for evidence of shunt dysfunction using Doppler ultrasound at 1-month, 3-months, and subsequent 6-month intervals post-procedure. Abnormalities identified at Doppler ultrasound10 were further evaluated by TIPS venography. Of note, repeat venography 24-48 h post-TIPS for measurement of the PSG is not routinely performed in the clinical practice of the authors, and no patients underwent scheduled repeat measurement at this time frame.
Measured outcomesThe primary objective of this study was determination of prognostic factors for early mortality after emergent TIPS creation and assessment of accuracy of the MELD system for prediction of early mortality after emergent TIPS. Secondary outcome measures included TIPS hemodynamic success, bleeding control, and procedure-related complications classified according to the Society of Interventional Radiology Standards of Practice Committee classification of complications.11 Hemodynamic success was defined as reduction in the portosystemic pressure gradient (PSG) to an absolute value ≤ 12 mm Hg.12,13 Bleeding control was assessed by post-TIPS rebleeding incidence, and recurrent hemorrhage was diagnosed by clinical signs such as hematemesis or coffee ground emesis accompanied by laboratory hemoglobin reduction requiring blood product transfusion, with endoscopic confirmation when possible.9 Post-TIPS hepatic encephalopathy (HE) was defined by development of new mental status changes (confusion) or alterations in level of consciousness. Presence of HE was determined clinically by the patient’s hepatologist and was graded according to the West Haven classification system.14
Statistical analysisThe statistical methods and approaches utilized herein paralleled those employed in the original MELD manuscript of Malinchoc, et al.1 The demographic features of the study population, laboratory data, and procedure outcomes were reported using descriptive statistics as number (percent) or median (interquartile range). Study patients were followed from the date of TIPS until date of death, liver transplantation, or last documented clinical follow-up. Clinical outcomes were evaluated until May 2014. Transplant free survival was calculated using Kaplan-Meier statistics. Univariate Cox proportional hazards regression analysis was used to assess the influence of individual demographic data, laboratory values, and procedure parameters on patient survival outcomes, akin to the factors analyzed by Malinchoc, et al.1 Variables exhibiting a significance level ≤ 0.05 on univariate analysis were entered into a multivariate Cox proportional hazards regression analysis. For Cox regression analysis, laboratory values were transformed to their natural logarithms in order to lessen the influence of extreme quantities. A risk score equation was generated from the multivariate prognostic parameters and their regression coefficients, and was used to ascertain a risk score associated with a 3month survival threshold. If comparison to the original MELD risk system showed similar prognostic parameters, further analysis would assess the accuracy of the original MELD score in the emergent TIPS population. Area under receiver operator characteristic (AUROC) curves or C-statistics was used to assess the capability of MELD score prediction of early mortality. Statistical analysis was performed utilizing a commercially available software package (SPSS version 21; SPSS Inc., Chicago IL). P-values ≤ 0.05 were considered statistically significant.
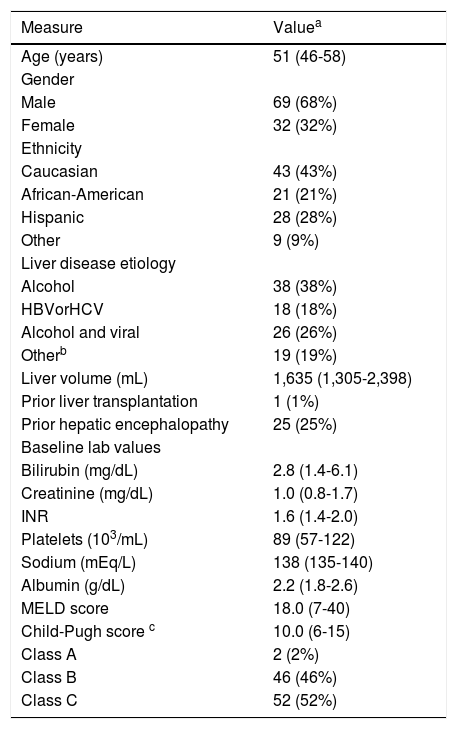
ResultsBaseline patient characteristicsPatient demographic data and liver disease characteristics of the study cohort are summarized in table 1. Within 48 h prior to TIPS procedures, 99/101 (98%) patients had a drop in hemoglobin greater than 1 g/dL, 64/101 (63%) received transfusion of ≥ 2 units of PRBCs, 30/101 (30%) required the use of vasopressors, and 53/101 (53%) required mechanical ventilation. Median number of PRBC units transfused per patient prior to TIPS was 4 (interquartile range 6). Thirty-five patients (35%) had failed endoscopic therapy within 24 h. Mean number of endoscopies per patient prior to TIPS was 1.9 ± 1.6 (median 1, range 1-8). Bleeding origin was found to be esophageal varices in 41/101 (41%) patients, gastric varices in 30/101 (30%) patients, both in 7/101 (7%), and rectal varices in 1/101 (1%), while the remaining had unknown origin.
Patient demographic and liver disease characteristics.
| Measure | Valuea |
|---|---|
| Age (years) | 51 (46-58) |
| Gender | |
| Male | 69 (68%) |
| Female | 32 (32%) |
| Ethnicity | |
| Caucasian | 43 (43%) |
| African-American | 21 (21%) |
| Hispanic | 28 (28%) |
| Other | 9 (9%) |
| Liver disease etiology | |
| Alcohol | 38 (38%) |
| HBVorHCV | 18 (18%) |
| Alcohol and viral | 26 (26%) |
| Otherb | 19 (19%) |
| Liver volume (mL) | 1,635 (1,305-2,398) |
| Prior liver transplantation | 1 (1%) |
| Prior hepatic encephalopathy | 25 (25%) |
| Baseline lab values | |
| Bilirubin (mg/dL) | 2.8 (1.4-6.1) |
| Creatinine (mg/dL) | 1.0 (0.8-1.7) |
| INR | 1.6 (1.4-2.0) |
| Platelets (103/mL) | 89 (57-122) |
| Sodium (mEq/L) | 138 (135-140) |
| Albumin (g/dL) | 2.2 (1.8-2.6) |
| MELD score | 18.0 (7-40) |
| Child-Pugh score c | 10.0 (6-15) |
| Class A | 2 (2%) |
| Class B | 46 (46%) |
| Class C | 52 (52%) |
HBV: hepatitis B virus. HCV: hepatitis C virus. INR: international normalized ratio. MELD: Model for End Stage Liver Disease.
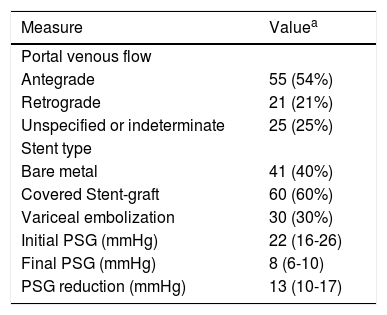
TIPS procedure results are summarized in table 2. TIPS were created 119 ± 167 (median 48, interquartile range 22-100) hours after the initial bleeding event. Of 84 patients with definitive data on time from initial bleeding to TIPS, 56 (67%) of TIPS procedure occurred within 72 h of hemorrhage, while 28 (33%) were performed more than 72 h later. Immediate post-TIPS hemodynamic success was achieved in 91/101 (90%) patients with median PSG reduction of 13 mmHg; PSG was not measured again at 24-48 h post-TIPS. Of 101 patients, 60 (60%) underwent covered Stent-graft TIPS, and 41 (40%) underwent bare metal Stent TIPS. Variceal embolization was performed in 30/101 (30%) patients. Procedure-related adverse events within 30days included HE in 33/101 (33%) patients and hepatic decompensation in 3/101 (3%). HE was predominantly minimal (grade 1, n = 10) or mild (grade 2, n = 14).
TIPS procedure findings and outcomes.
| Measure | Valuea |
|---|---|
| Portal venous flow | |
| Antegrade | 55 (54%) |
| Retrograde | 21 (21%) |
| Unspecified or indeterminate | 25 (25%) |
| Stent type | |
| Bare metal | 41 (40%) |
| Covered Stent-graft | 60 (60%) |
| Variceal embolization | 30 (30%) |
| Initial PSG (mmHg) | 22 (16-26) |
| Final PSG (mmHg) | 8 (6-10) |
| PSG reduction (mmHg) | 13 (10-17) |
TIPS: transjugular intrahepatic portosystemic shunt. PSG: portosystemic pressure gradient.
At the end of the data collection period, 21/101 (21%) patients experienced recurrent variceal hemorrhage. Eleven cases (52%) occurred within 2-days, and 16 cases (76%) within 2-weeks. The 30-day, 90day, 180-day, 1-year, and 2-year post-procedure rebleeding probabilities were 16%, 17%, 18%, 18%, and 18%, respectively. The median time to rebleeding event was 2-days (interquartile range 2-49) days. Of 21 patients with recurrent hemorrhage, 14 (67%) initially had esophageal variceal bleeding and 5 (24%) initially had gastric variceal bleeding.
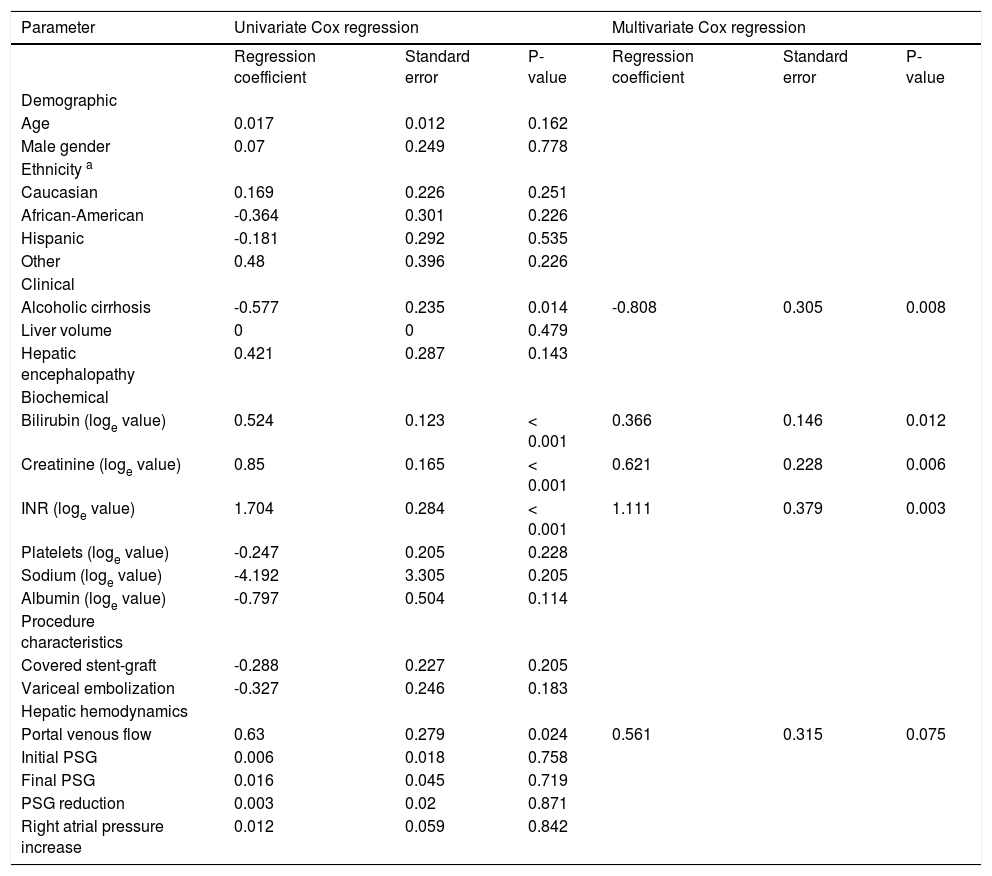
Patient survival and prognostic factors for mortalityAt the end of the data collection period, 80/101 (79%) patients had expired. The 30-day, 90-day, 180day, 1-year, and 2-year post-procedure survival probabilities were 69%, 60%, 55%, 44%, and 34%, respectively. The median survival time was 270 (95% CI 112-428) days. Table 3 shows the predictive capacity of various factors for overall mortality after TIPS creation. On univariate analysis, non-alcoholic liver disease etiology, baseline bilirubin, creatinine, international normalized ratio (INR), and retrograde portal venous flow direction -as determined angiographically immediately after shunt placement- were found to be significant predictors of overall mortality. On multivariate analysis, baseline bilirubin, creatinine, INR, and liver disease etiology were confirmed as independent predictors of overall mortality. The identification of these MELD components confirmed applicability of the MELD score in the emergent TIPS population. To that end, MELD was also found to be a significant independent predictor of overall mortality on Cox proportional hazards regression (P < 0.001).
Predictors of mortality among emergent TIPS patients.
| Parameter | Univariate Cox regression | Multivariate Cox regression | ||||
|---|---|---|---|---|---|---|
| Regression coefficient | Standard error | P-value | Regression coefficient | Standard error | P-value | |
| Demographic | ||||||
| Age | 0.017 | 0.012 | 0.162 | |||
| Male gender | 0.07 | 0.249 | 0.778 | |||
| Ethnicity a | ||||||
| Caucasian | 0.169 | 0.226 | 0.251 | |||
| African-American | -0.364 | 0.301 | 0.226 | |||
| Hispanic | -0.181 | 0.292 | 0.535 | |||
| Other | 0.48 | 0.396 | 0.226 | |||
| Clinical | ||||||
| Alcoholic cirrhosis | -0.577 | 0.235 | 0.014 | -0.808 | 0.305 | 0.008 |
| Liver volume | 0 | 0 | 0.479 | |||
| Hepatic encephalopathy | 0.421 | 0.287 | 0.143 | |||
| Biochemical | ||||||
| Bilirubin (loge value) | 0.524 | 0.123 | < 0.001 | 0.366 | 0.146 | 0.012 |
| Creatinine (loge value) | 0.85 | 0.165 | < 0.001 | 0.621 | 0.228 | 0.006 |
| INR (loge value) | 1.704 | 0.284 | < 0.001 | 1.111 | 0.379 | 0.003 |
| Platelets (loge value) | -0.247 | 0.205 | 0.228 | |||
| Sodium (loge value) | -4.192 | 3.305 | 0.205 | |||
| Albumin (loge value) | -0.797 | 0.504 | 0.114 | |||
| Procedure characteristics | ||||||
| Covered stent-graft | -0.288 | 0.227 | 0.205 | |||
| Variceal embolization | -0.327 | 0.246 | 0.183 | |||
| Hepatic hemodynamics | ||||||
| Portal venous flow | 0.63 | 0.279 | 0.024 | 0.561 | 0.315 | 0.075 |
| Initial PSG | 0.006 | 0.018 | 0.758 | |||
| Final PSG | 0.016 | 0.045 | 0.719 | |||
| PSG reduction | 0.003 | 0.02 | 0.871 | |||
| Right atrial pressure increase | 0.012 | 0.059 | 0.842 | |||
INR: international normalized ratio. PSG: portosystemic pressure gradient.
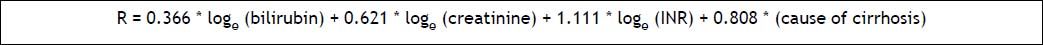
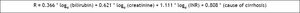
Based on regression coefficients, INR had the highest correlation with mortality (1.111), followed by cirrhosis etiology (0.808), creatinine (0.621), and bilirubin (0.366), comparable to findings of Malinchoc, et al.,1 who similarly demonstrated highest correlation with INR and lowest association with bilirubin. A TIPS risk score equation for our emergent TIPS population was thus defined by the formula (Figure 1).
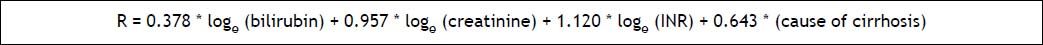
The generated risk equation bears significant similarity to the original MELD risk formula generated by Malinchoc, et al.,1 with particularly comparable regression coefficients for bilirubin (0.378 in original MELD manuscript) and INR (1.120 in original MELD manuscript). Based on both the emergent TIPS risk equation produced herein as well as the original MELD risk equation developed by Malinchoc, et al.,1 the average risk score for an emergent TIPS patient in the current study was 1.70, higher than the average risk score (1.13) identified by Malinchoc, et al.1 for elective TIPS patients.
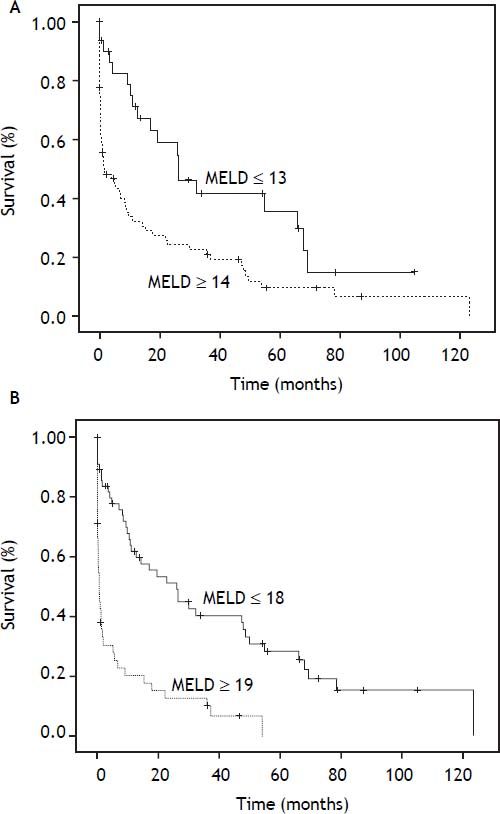
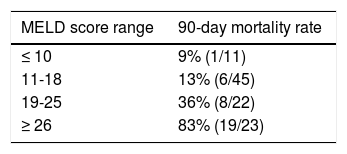
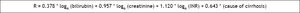
MELD score predictive capacity and survival thresholdsBased on identification of identical prognostic parameters for survival after emergent TIPS, the accuracy of the original MELD score in the emergent TIPS population was assessed in comparison to the risk equation generated herein. Baseline MELD score was highly predictive of 90-day mortality within the emergent TIPS study cohort, with an AUROC value of 0.842 (95% CI 0.755-0.928). The risk equation generated herein had statistically similar predictive accuracy (0.845, 95% CI 0.762-0.928). Using AUROC analysis, a MELD cut-off at 18 had a sensitivity and specificity of 80.9% and 69.4%, respectively, for predicting 90-day post-TIPS mortality; however, the optimal MELD threshold in the emergent population was a score of 20, with sensitivity and specificity of 77.9 and 79.9%, respectively. Using the original MELD risk equation, AUROC analysis showed that a MELD score threshold of 14 corresponded to median survival less than 3-months (Figure 2), while a MELD score threshold of 18 corresponded to median survival less than 1-month (Figure 2). The 90-day post-TIPS mortality rates for different MELD score ranges are shown in table 4.
Kaplan-Meier transplant free survival curve (a) of patients stratified by baseline MELD score above or below 13, which represents threshold for 3-month median survival. Median survival of patients with baseline MELD score ≤ 13 significantly greater than those with baseline MELD scores ≥ 14 (26.5 vs. 1.6 months, P = 0.002). Kaplan-Meier transplant free survival curve (b) of patients stratified by baseline MELD score above or below 18. Median survival of patients with baseline MELD score ≤ 18 significantly greater than those with baseline MELD scores ≥ 19 (26.1 vs. 0.57 months, P < 0.001).
Although the MELD score is the foremost risk stratification system for prediction of TIPS mortality outcomes,3–5,15,16 its applicability to the emergent TIPS population is poorly established given its derivation from elective procedures, and its usefulness in this scenario has been questioned.17 While Tseng, et al. demonstrated a high accuracy (AUROCs exceeding 0.7) of the MELD score for prediction of 30-, 60-, and 360-day mortality in a cohort of 107 patients who underwent emergent TIPS,7 their investigation did not specifically derive a relationship between MELD parameters and survival outcomes. Mukund, et al. likewise found independent prognostic capability of MELD in emergent TIPS, but similarly did not derive predictive ability of MELD constituents.18 Moreover, other studies exploring prognostic factors for survival after emergent TIPS procedures have identified a heterogeneous set of impactful parameters, including presence of ascites, use of mechanical ventilation, white blood cell count, platelet count, partial thromboplastin time (PTT), creatinine, bilirubin, sepsis occurrence, use of catecholamines for hemodynamic support, need for balloon tamponade, and procedure urgency itself.19–23 These elements have led to the development and use of scoring systems such as the prognostic index (PI),19 acute physiology and chronic health evaluation (APACHE) 2 score,24 Bonn TIPS early mortality (BOTEM) score,25 and Emory score22 for risk stratification in the emergent TIPS setting.26 While all of these scoring systems have shown prognostic value,6 use of the simple, objective, and consistent MELD score may be more desirable in order to enhance uniformity in risk assessment across both elective and emergent TIPS procedures.
In the current investigation, we independently derived the MELD system from a retrospective cohort of 101 patients undergoing emergent TIPS procedures. We found that serum bilirubin, creatinine, INR, and non-alcoholic liver disease etiology were significant independent predictors of overall mortality, as identified for elective TIPS procedures more than a decade ago. When comparing the current results to the original MELD score proposal by Malinchoc, et al.1 not only were the significant predictive risk factors the same, but the regression coefficients were also particularly similar as well, despite origination from a cohort of emergent TIPS patients. Most notably, regression coefficients for INR and bilirubin identified herein were similar to those in the MELD equation (Figure 3) to within approximately 1 and 3%, respectively. Further analysis of MELD score accuracy using AUROC analysis revealed excellent predictive capacity for 3-month mortality in the emergent population. In all, based on independent derivation of prognostic factors and confirmation of predictive accuracy, we believe that the MELD score is a valid and reliable metric for risk stratification and survival projection after emergent TIPS. This is particularly relevant given emerging data substantiating use of early TIPS in the treatment algorithm for acute variceal hemorrhage;27,28 the current study supports use of MELD score for patient risk stratification in this setting.
A notable difference in MELD risk threshold was identified between the emergent TIPS population in this study and elective cases in the published literature. We found that the average risk score for an emergent TIPS patient herein was higher than the average risk score identified by Malinchoc, et al.1 for elective TIPS patients (1.70 vs. 1.13). Furthermore, a MELD score threshold of 14 corresponded to median survival less than 3-months in the emergent setting, in contrast to the risk cutoff found by Malinchoc, et al.,1 in which less than 3-month survival occurred at a threshold MELD score of 18 (a MELD score threshold of 18 corresponded to median survival less than 1-month in our emergent population). These findings indicate that emergent TIPS confers generally higher risk than elective TIPS, and reflect a risk disparity between emergent and elective TIPS patient populations. As opposed to elective TIPS, in which MELD score greater than 18 are associated with poorer outcomes, patients with MELD scores ≥ 14 undergoing emergent TIPS should be considered higher risk. We speculate that this increased risk reflects the hazard of variceal bleeding rather than incrementally greater risk attributable to the TIPS procedure in the emergent scenario. Notably, the optimal MELD threshold for early mortality detection in the emergent population identified herein was a score of 20, similar to that determined by Tseng, et al.7
Patients undergoing emergent TIPS are often critically ill and thus at high risk of poor outcome and early mortality.17 Previous reports on emergent TIPS populations have shown a wide range in clinical outcomes, with 30-day mortality incidence ranging from 17-60% and rates of variceal rebleeding between 11-50%.17 The results of the current study are consistent with these findings, showing 30-day mortality and rebleeding rates of 31% and 16%, respectively, following emergent TIPS. Notably, comparison of such clinical outcomes to historical controls must be in the context of baseline liver disease magnitude, patient comorbid conditions, TIPS timing, and type of medical management. To this end, a recent landmark randomized controlled trial of 32 patients who underwent emergent TIPS reported excellent clinical outcomes, with 1-year postTIPS mortality in only 14%, recurrent hemorrhage in only 3%, and an HE rate of 28%,27 compared with 56%, 18%, and 33% in the current study. However, mean MELD score was markedly lower in the former investigation as compared to the latter (15.5 vs. 19.8), and the incidence of shock was lower than in the current study (22% vs. 30%). Furthermore, TIPS were created earlier during the acute bleeding period in the study of Garcia-Pagan, et al.27 (all within 72 h vs. only two-thirds within 72 h herein). Another notable difference relates to the long inclusion period in the present study, which may have prevented application of optimal contemporary medical therapy with vasoactive drugs and antibiotic prophylaxis in all patients, further negatively impacting survival. In all, these outcome disparities corroborate the notion that application of early TIPS combined with up-to-date pharmacological management in properly selected patients may optimize clinical outcomes in the emergent TIPS setting.
There are limitations to this investigation. First, this study was retrospective and non-randomized nature, represents the experience of a single institution, and includes a limited sample size. A prospective validation study performed at multiple centers would be necessary to further substantiate the findings herein. Second, the definition of emergent TIPS used here was somewhat subjective. However, there is no formally recognized definition of emergent TIPS, and selected cases were characterized by an immediate threat to life with clinical and/or laboratory signs of persistent or refractory variceal bleeding, similar to cases deemed emergent in the original MELD manuscript of Malinchoc, et al.1 and excluded from their analysis. Third, because patients in this study were accrued over an approximately decade-long period, technical differences in TIPS creation and disparities in medical care during the study period may have contributed to differences in clinical outcomes over time. Fourth, mortality was considered collectively herein rather than specific assessment for liver failure induced death. However, all-cause mortality was also used in the original MELD study of Malinchoc, et al.1 Fifth, the current study did not attempt to compare the relative accuracy of MELD for emergent versus non-emergent variceal bleeding indications.
ConclusionIn conclusion, use of TIPS under emergency conditions for bleeding varices is supported by emerging data showing survival benefit,27,28 and simple and reliable methods to predict prognosis are necessary. Recently, Reverter, et al. tested and validated a MELD-based prognostic model to predict survival of patients after acute variceal bleeding due to portal hypertension.29 With a similar endorsement required for the predictive capability of MELD in the setting of portal decompressive therapy of variceal bleeding, the current study presented independent derivation of the MELD system in a population of patients undergoing emergent TIPS, with subsequent validation of the traditional MELD score for accurate prediction of 3-month mortality. These results support use of the MELD system for outcomes prognostication in the emergent TIPS population, although an expectedly lower quantitative threshold is associated with mortality risk similar to elective procedures.
Abbreviations- •
APACHE: acute physiology and chronic health evaluation.
- •
AUROC: area under receiver operator characteristic.
- •
BOTEM: Bonn TIPS early mortality
- •
HE: hepatic encephalopathy.
- •
INR: international normalized ratio.
- •
IR: interventional radiology.
- •
MELD: Model for End Stage Liver Disease.
- •
PI: prognostic index.
- •
PRBCs: packed red blood cells.
- •
PSG: portosystemic pressure gradient.
- •
TIPS: transjugular intrahepatic portosystemic shunt.
None.