To identify clinical characteristics, treatment modalities, and course of spontaneous rectus sheath hematoma (SRSH). In the literature, there is no prospective clinical trial that is intended for treatment in clinical research.
MethodsSeventeen SRSH patients diagnosed and treated between March 2012 and March 2014 at the general Surgery Department of Erzincan University Training and Research Hospital were included. Age, sex, weight, height, predisposing factors, comorbid diseases, Charlson index, current medical treatment, physical examination signs, imaging methods, lowest hemoglobin value, blood type, SRSH type, INR/Factor V Leiden mutation/Factor VII/Factor VIII/Factor X/Protein S/Protein C values, treatment method, transfusions hospitalization duration, and outcome were studied.
ResultsThirteen patients were female. The mean age was 63.3±18.7 years (range, 22–87 years), and the mean BMI was 27.8±3.5 (range, 20.9–33.7). Six patients had Grade I SRSH, 5 had Grade II SRSH, and 6 had Grade III SRSH. Thirteen were hospitalized for a mean duration of 9.3±8.1 days (range, 1–30 days). The death rate attributable to SRSH was 5.8%.
ConclusionEarly diagnosis of SRSH by ultrasonography and/or computerized tomography is important for a low mortality rate. Even though medical treatments are important, arterial embolization by interventional radiology, or more radical interventions such as surgery, may be required.
Identificar las características clínicas, las modalidades de tratamiento y la evolución del hematoma espontáneo de la vaina del recto (HEVR). En la literatura, no hay ningún estudio clínico prospectivo sobre el tratamiento en un ámbito de investigación clínica.
MétodosSe incluyeron en el estudio 17 pacientes con HEVR que fueron diagnosticados y tratados entre marzo de 2012 y marzo de 2014 en el Departamento de Cirugía General del Hospital Docente e Investigador de la Universidad de Erzincan. Se evaluaron los datos de edad, sexo, peso, altura, factores predisponentes, comorbilidades, índice de Charlson, tratamiento médico actual, signos a la exploración física, exploraciones de diagnóstico por la imagen, valor mínimo de la hemoglobina, tipo sanguíneo, tipo de HEVR, valores de INR/mutación de factor v Leiden/factor vii/factor viii/factor x/proteína S/proteína C, método de tratamiento, transfusiones, duración de la hospitalización y evolución clínica.
ResultadosTrece pacientes fueron mujeres. La media de edad fue de 63,3±18,7 años (rango, 22–87 años), y la media del IMC fue de 27,8±3,5 (rango, 20,9–33,7). Seis pacientes presentaban un HEVR de grado i, 5 un HEVR de grado ii y 6 un HEVR de grado iii. Trece fueron ingresados durante un periodo medio de hospitalización de 9,3±8,1 días (rango, 1–30 días). La tasa de mortalidad atribuible al HEVR fue del 5,8%.
ConclusionesUn diagnóstico precoz del HEVR mediante ecografía y/o tomografía computarizada es importante para obtener una tasa de mortalidad baja. A pesar de que los tratamientos médicos son importantes, pueden ser necesarias una embolización arterial mediante radiología intervencionista o intervenciones más radicales como la cirugía.
Rectus sheath hematoma is the direct rupture or damage of inferior or superior epigastric arteries. As a result, blood accumulates in the rectus sheath.1,2 Because there is no previous surgery in most cases, the process is referred to as spontaneous rectus sheath hematoma (SRSH).3 In the past, this disease was rarely seen. The initial clinical diagnosis of the disease may be difficult because it can be confused with other conditions. For example, it may be diagnosed as an intra-abdominal inflammatory process, thus causing a delay in diagnosis and unnecessary laparotomy. The sudden onset of abdominal pain with palpable abdominal masses in elderly women is a general clinical presentation. In the etiology, female sex, advanced age, anticoagulant therapy, and exaggerated abdominal wall tension are associated with the disease.4 An obscure etiology of SRSH is deficiency of coagulation factors, which is rarely defined. In particular, deficiencies in factors VII and X are observed.5
Among radiologically evaulated patients with acute abdominal pain, the annual estimated rate of SRSH is 1.2%–1.5%. As a result, the average physician rarely encounters this clinical situtation. While bed rest and analgesia are the standard treatment protocols, more radical interventions may be needed.6 Although SRSH may regress with conservative treatment, the mortality rate may be as high as 4%, and this rate increases up to 25% in the presence of anticoagulant usage.3 The identification of SRSH etiological factors facilitates diagnosis at the time of presentation, ensuring fast and effective treatment. The purpose of this prospective study is to identify clinical characteristics, treatment modalities, and the course of the disease. In the literature, there is no other prospective series on this clinical condition.
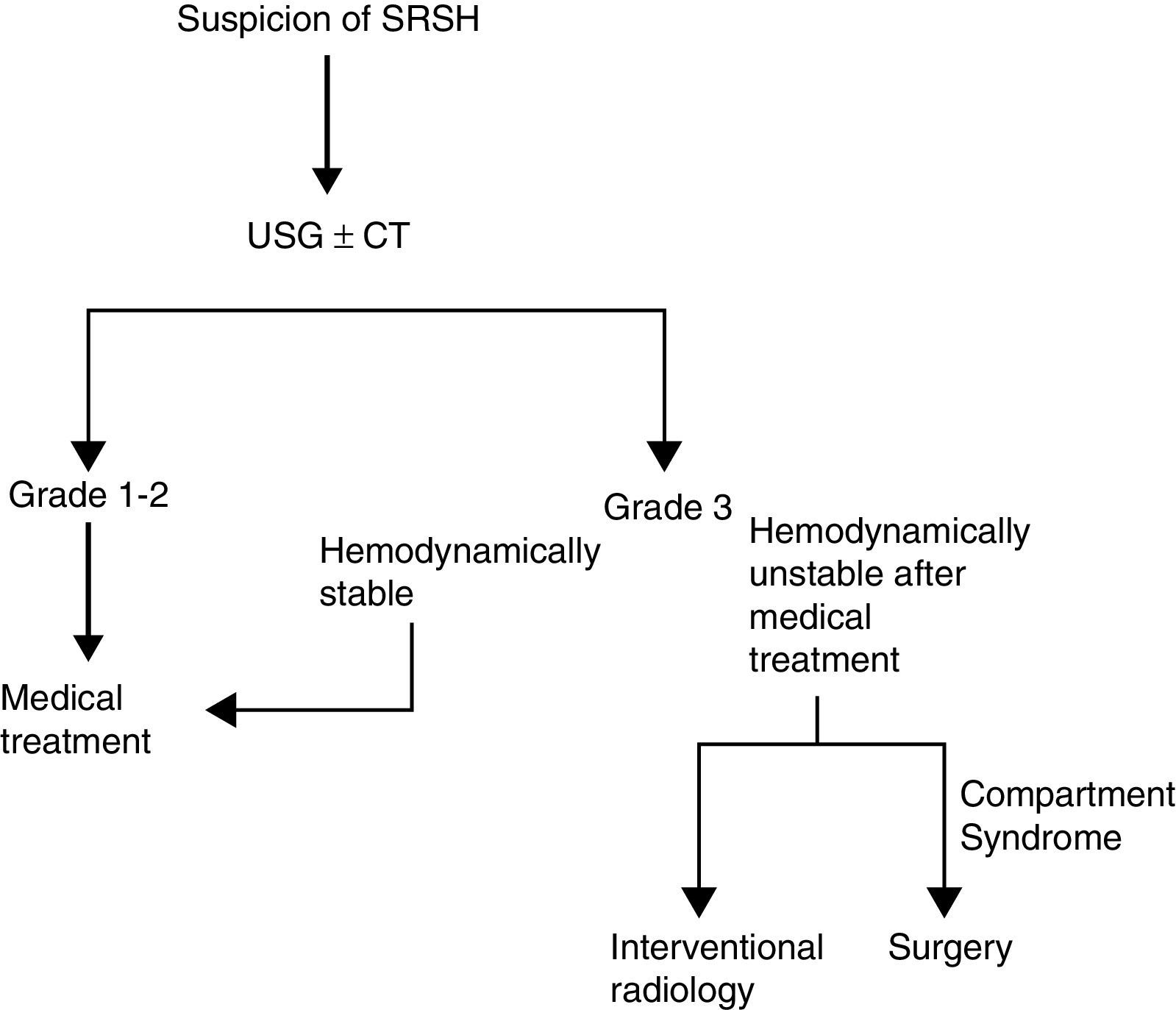
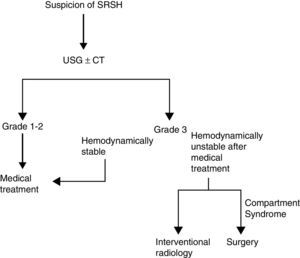
MethodsWe included SRSH patients diagnosed and treated between March 2012 and March 2014 at the general surgery clinic of Erzincan University Training and Research Hospital. Erzincan University Training and Research Hospital is a tertiary referral hospital. Microsoft Excel 2007 was used after each treatment to record different factors such as age, sex, weight, height, predisposing factors (cough, exercise, etc.), and comorbid diseases. Also recorded were Charlson index, current medical treatment (anticoagulant, antiplatelet, antiaggregant, etc.), physical examination signs (Carnett/Fothergill's sign), and imaging methods such as ultrasonography (US) and computerized tomography (CT). Finally, lowest hemoglobin value, blood type, SRSH type, INR/Factor V Leiden Mutation/Factor VII/Factor VIII/Factor X/Protein S/Protein C values, treatment methods (medical, arterial embolization by interventional radiology, surgery), transfusion, hospital stay and outcome (cure, death, cause of death) were recorded as well. The Factor VII/Factor VIII/Factor X/Protein S/Protein C values of patients using anticoagulants, antiplatelets, antiaggregants, etc. were also recorded one week after the last medication dose. We used physical examination and imaging methods to diagnose SRSH, and patients were divided into three groups based on imaging method. The Grade I group had intramuscular, unilateral hematoma that did not dissect along the fascia. The Grade II group had intramuscular hematoma that could be bilateral and dissect along the fascia, leading to a possible drop in hemoglobin. The Grade III group had a hematoma that dissected along the fascia with extraperitoneal extension or intraperitoneal extension and prevesical blood that lead to a drop in hemoglobin.7 The diagnosis and treatment protocol applied is shown in Fig. 1. Grade I patients with comorbid diseases and all Grade II and Grade III patients were hospitalized. When regression of hematoma was confirmed using US, the patient was discharged. All patients were referred to AI and followed up by AI. This study was conducted according to the Declaration of Helsinki and local ethical approval was obtained from the Erzincan University Ethical Committee. Informed consent was obtained from all patients.
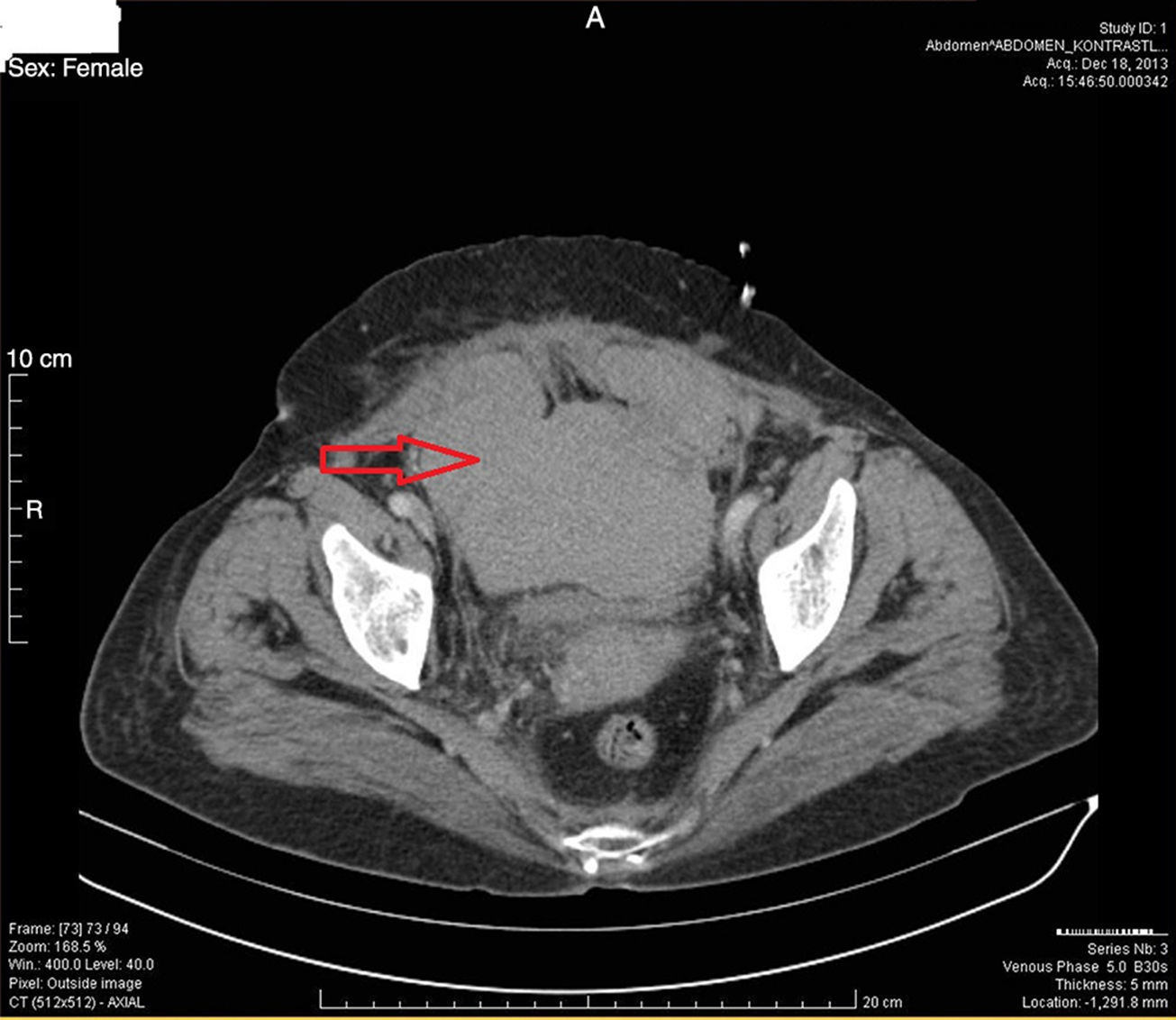
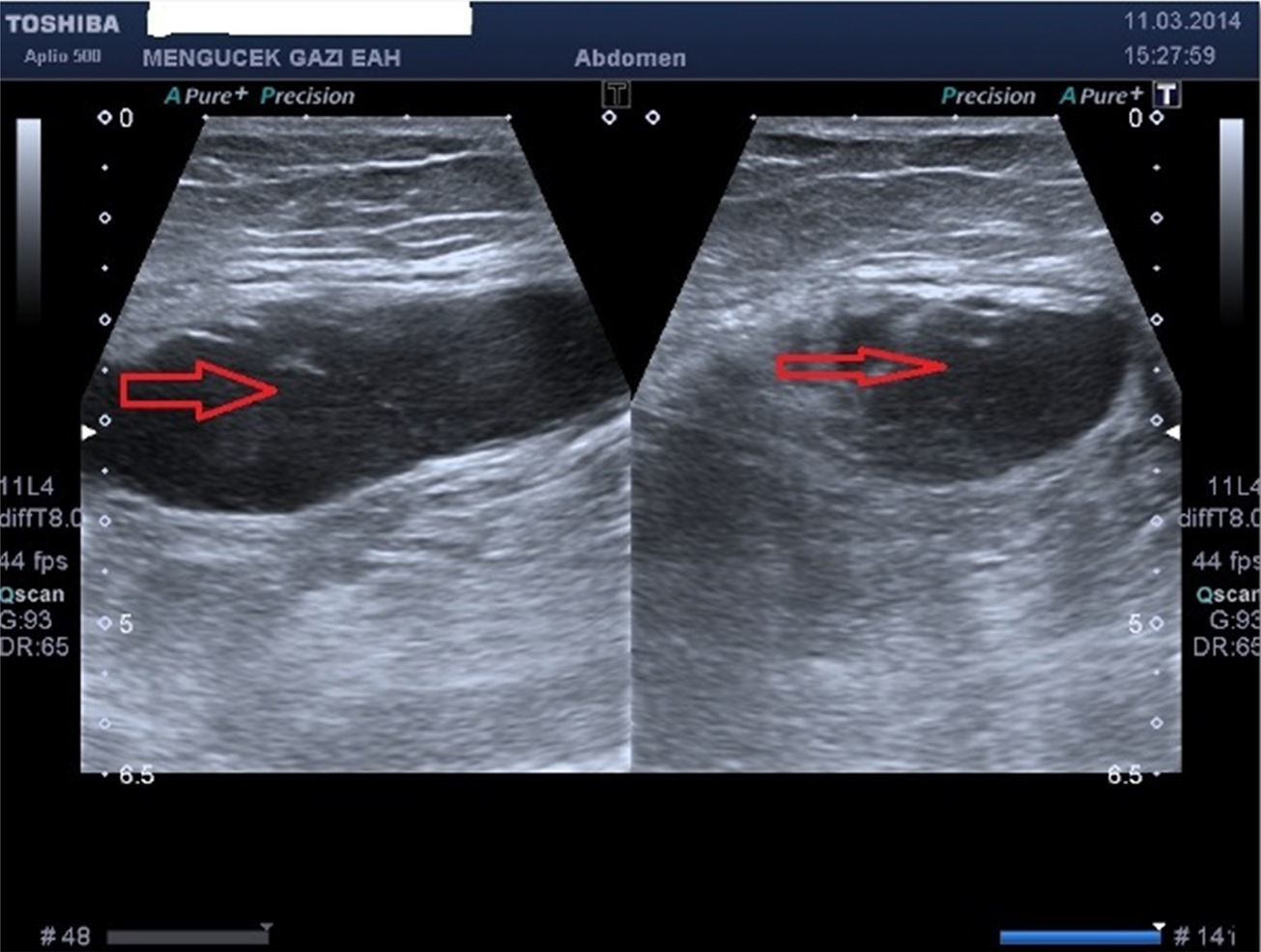
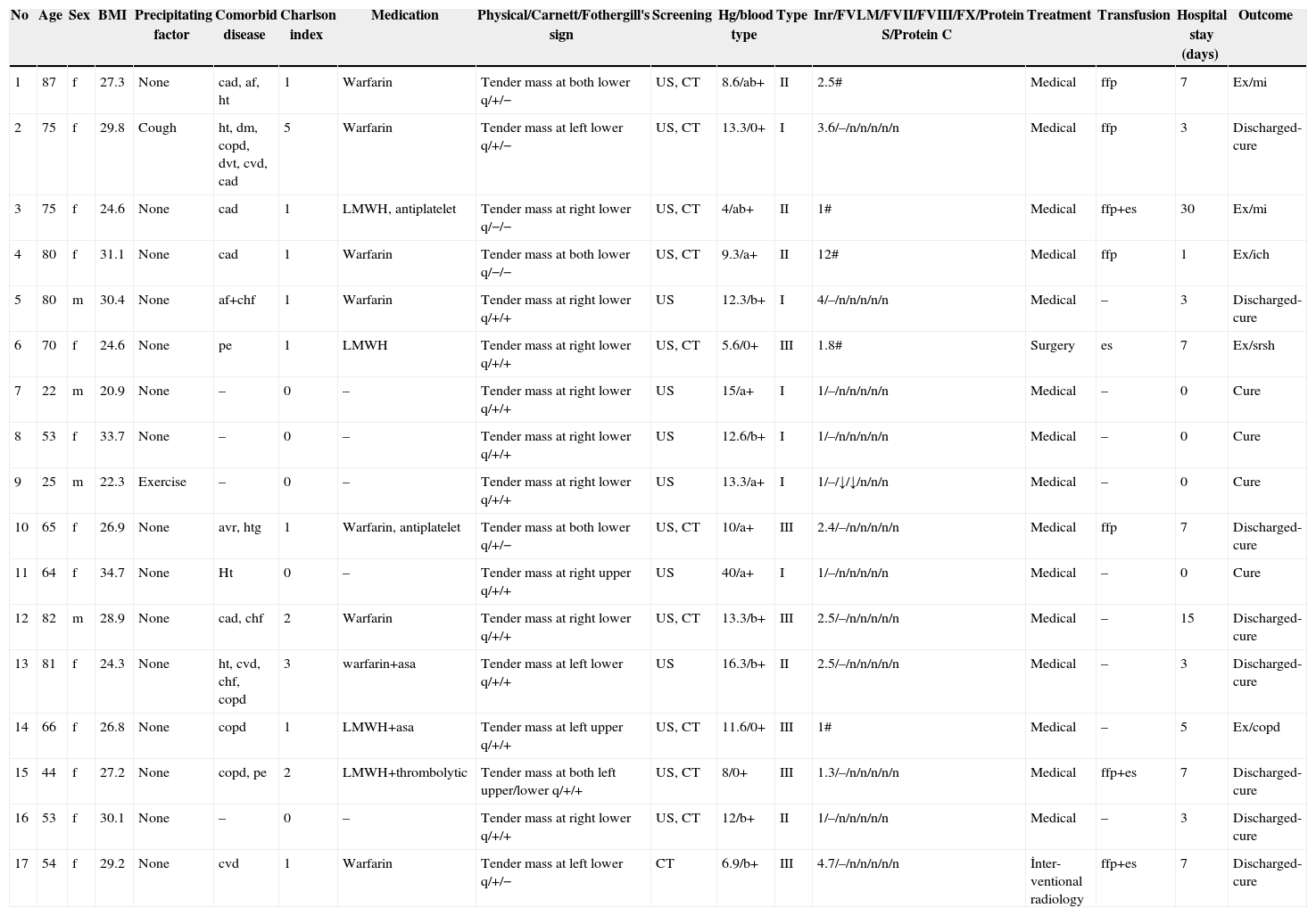
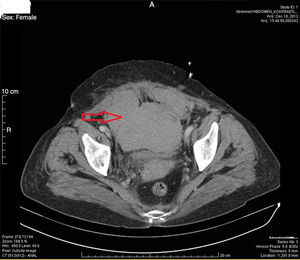
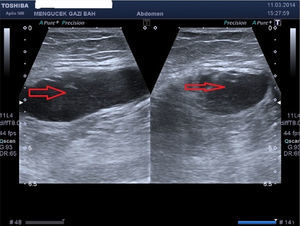
ResultsThirteen patients (76.5%) were female. The mean age was 63.3±18.7 years (range, 22–87 years). Mean BMI was 27.8±3.5 (range, 20.9–33.7). Thirteen patients (76.5%) were admitted to the emergency department and all others were admitted to an outpatient clinic. Thirteen patients (76.5%) were hospitalized. The mean hospital stay was 9.3±8.1 days (range, 1–30). On 4 (23.5%) patients who were not hospitalized, an outpatient follow-up protocol was used as 1st week and 1st–6th months control. They had less pain than the hospitalized patients, and non steroidal anti inflammatory drugs were given. Six patients (35.3%) were in the Grade I group, 5 patients (29.4%) were in the Grade II group, and 6 patients (35.3%) were in the Grade III group. Five patients (29.4%) were not on anticoagulant, antiplatelet (clopidogrel), antiaggregant, etc. treatment. The majority of patients (8 individuals, 47%) had a tender mass in the right lower quadrant. Fifteen patients (88.2%) had Carnett's sign, and 11 patients (64.7%) had Fothergill's sign. A CT scan (Fig. 2) subsequent to US (Fig. 3) was used for diagnosis in 10 patients (58.8%). Six patients (35.3%) were diagnosed using only US. Of 12 patients in whom factor levels could be measured, only one had factor VII–VIII deficiencies. Erythrocyte suspension was used to increase hemoglobin levels and/or fresh frozen plasma was used to neutralize the effect of coumadin in 8 patients (47%). Medical treatment was used in 15 patients (88.2%). Arterial embolization by interventional radiology was used in 1 patient. One patient who had abdominal compartment syndrome was operated on and died on the 6th postoperative day. However, SRSH is neither the only cause of long hospitalizations, nor the only cause of death. Long hospitalizations are generally caused by comorbid diseases. The other causes of death are comorbidities such as myocardial infarction, chronic obstructive pulmonary disease, and intracerebral hemorrhage. The death rate from SRSH was 5.8%; all data are shown in Table 1.
Patients Charts.
| No | Age | Sex | BMI | Precipitating factor | Comorbid disease | Charlson index | Medication | Physical/Carnett/Fothergill's sign | Screening | Hg/blood type | Type | Inr/FVLM/FVII/FVIII/FX/Protein S/Protein C | Treatment | Transfusion | Hospital stay (days) | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 87 | f | 27.3 | None | cad, af, ht | 1 | Warfarin | Tender mass at both lower q/+/− | US, CT | 8.6/ab+ | II | 2.5# | Medical | ffp | 7 | Ex/mi |
| 2 | 75 | f | 29.8 | Cough | ht, dm, copd, dvt, cvd, cad | 5 | Warfarin | Tender mass at left lower q/+/− | US, CT | 13.3/0+ | I | 3.6/–/n/n/n/n/n | Medical | ffp | 3 | Discharged-cure |
| 3 | 75 | f | 24.6 | None | cad | 1 | LMWH, antiplatelet | Tender mass at right lower q/−/− | US, CT | 4/ab+ | II | 1# | Medical | ffp+es | 30 | Ex/mi |
| 4 | 80 | f | 31.1 | None | cad | 1 | Warfarin | Tender mass at both lower q/−/− | US, CT | 9.3/a+ | II | 12# | Medical | ffp | 1 | Ex/ich |
| 5 | 80 | m | 30.4 | None | af+chf | 1 | Warfarin | Tender mass at right lower q/+/+ | US | 12.3/b+ | I | 4/–/n/n/n/n/n | Medical | – | 3 | Discharged-cure |
| 6 | 70 | f | 24.6 | None | pe | 1 | LMWH | Tender mass at right lower q/+/+ | US, CT | 5.6/0+ | III | 1.8# | Surgery | es | 7 | Ex/srsh |
| 7 | 22 | m | 20.9 | None | – | 0 | – | Tender mass at right lower q/+/+ | US | 15/a+ | I | 1/–/n/n/n/n/n | Medical | – | 0 | Cure |
| 8 | 53 | f | 33.7 | None | – | 0 | – | Tender mass at right lower q/+/+ | US | 12.6/b+ | I | 1/–/n/n/n/n/n | Medical | – | 0 | Cure |
| 9 | 25 | m | 22.3 | Exercise | – | 0 | – | Tender mass at right lower q/+/+ | US | 13.3/a+ | I | 1/–/↓/↓/n/n/n | Medical | – | 0 | Cure |
| 10 | 65 | f | 26.9 | None | avr, htg | 1 | Warfarin, antiplatelet | Tender mass at both lower q/+/− | US, CT | 10/a+ | III | 2.4/–/n/n/n/n/n | Medical | ffp | 7 | Discharged-cure |
| 11 | 64 | f | 34.7 | None | Ht | 0 | – | Tender mass at right upper q/+/+ | US | 40/a+ | I | 1/–/n/n/n/n/n | Medical | – | 0 | Cure |
| 12 | 82 | m | 28.9 | None | cad, chf | 2 | Warfarin | Tender mass at right lower q/+/+ | US, CT | 13.3/b+ | III | 2.5/–/n/n/n/n/n | Medical | – | 15 | Discharged-cure |
| 13 | 81 | f | 24.3 | None | ht, cvd, chf, copd | 3 | warfarin+asa | Tender mass at left lower q/+/+ | US | 16.3/b+ | II | 2.5/–/n/n/n/n/n | Medical | – | 3 | Discharged-cure |
| 14 | 66 | f | 26.8 | None | copd | 1 | LMWH+asa | Tender mass at left upper q/+/+ | US, CT | 11.6/0+ | III | 1# | Medical | – | 5 | Ex/copd |
| 15 | 44 | f | 27.2 | None | copd, pe | 2 | LMWH+thrombolytic | Tender mass at both left upper/lower q/+/+ | US, CT | 8/0+ | III | 1.3/–/n/n/n/n/n | Medical | ffp+es | 7 | Discharged-cure |
| 16 | 53 | f | 30.1 | None | – | 0 | – | Tender mass at right lower q/+/+ | US, CT | 12/b+ | II | 1/–/n/n/n/n/n | Medical | – | 3 | Discharged-cure |
| 17 | 54 | f | 29.2 | None | cvd | 1 | Warfarin | Tender mass at left lower q/+/− | CT | 6.9/b+ | III | 4.7/–/n/n/n/n/n | İnter-ventional radiology | ffp+es | 7 | Discharged-cure |
Hg: Hemoglobin, f: female, m: male, cad: coronary artery disease, af: atrial fibrillation, ht: hypertension, dm: diabetus mellitus, copd: chronic obstructive pulmonary disease, dvt: deep vein thrombosis, cvd: cerebrovascular disease, chf: congestive heart failure, pe: pulmunary emboli, avr: atrial valve replacement, htg: hypertriglyceridemia, LMWH: low molecular weight heparin, ffp: fresh frozen plasma, es: erythrocyte suspension, #: unavailable, q: quadrant, n: normal, ex: exitus, mi: myocardial infarction, ich: intracerebral hemorrhage, asa: acetylsalicylic acid.
Spontaneous rectus sheath hematoma has a high mortality rate and is commonly seen in elderly women, particularly those being treated with anticoagulants. Patients often complain of abdominal pain and have palpable abdominal masses. Several etiological factors such as asthma, hypertension, pregnancy, and warfarin usage were researched. Patients with acute abdominal pain may be misdiagnosed with appendicitis, diverticulitis, or perforation.8,9 Moreover, these patients may be inadvertantly operated on. Consequently, a precise diagnosis might be delayed. This disease is commonly found in females10; 76.5% of patients in our study were female. Spontaneous rectus sheath hematoma is mostly seen in the lower abdomen, as in the study of Anyfantakis et al.11 We typically found SRSH in the lower right quadrant (47%). Differential diagnosis must be conducted to exclude acute appendicitis, which is the most commonly reported cause for acute abdominal pain. Above the arcuate line, the posterior sheath of the rectus has a buffering effect; below the arcuate line, there is weak fascia transversalis and peritoneum, which may be why SRSH is mostly observed in the lower abdomen. Furthermore, changes in the length of muscle were seen mostly in the lower quadrants during movement, and thus may be likely causes of the ruptures of inferior epigastric vessels. Likewise, SRSH may be misdiagnosed due to peritoneal irritation signs because it is close to the peritoneum.12
Low molecular weight heparin (LMWH) usage rarely results in rectus hematoma compared with warfarin, but in this study, such a result was observed. Single LMWH usage might be a result of iatrogenic injury to the inferior epigastric vessels during subcutaneous injection in the abdomen. For these drugs, injections to the deltoid region may be safer than injections to the abdomen. The factors level will be within normal range 72–96h after ending warfarin. Considering this situtation, the factor levels of the patients using anticoagulants, antiaggregants, etc. were routinely checked on the 7th day after the last dose of these drugs. Only one patient had low factor levels. Because of a deficiency of factors, intra-abdominal, intramuscular, or intra-articular hemorrhage, as well as intramuscular hemorrhage, can be seen as rectus hematoma. In the literature, in these groups of patients, only one case report exists of detected blood factor levels and diagnosed low levels of factor VII and factor X, respectively.13
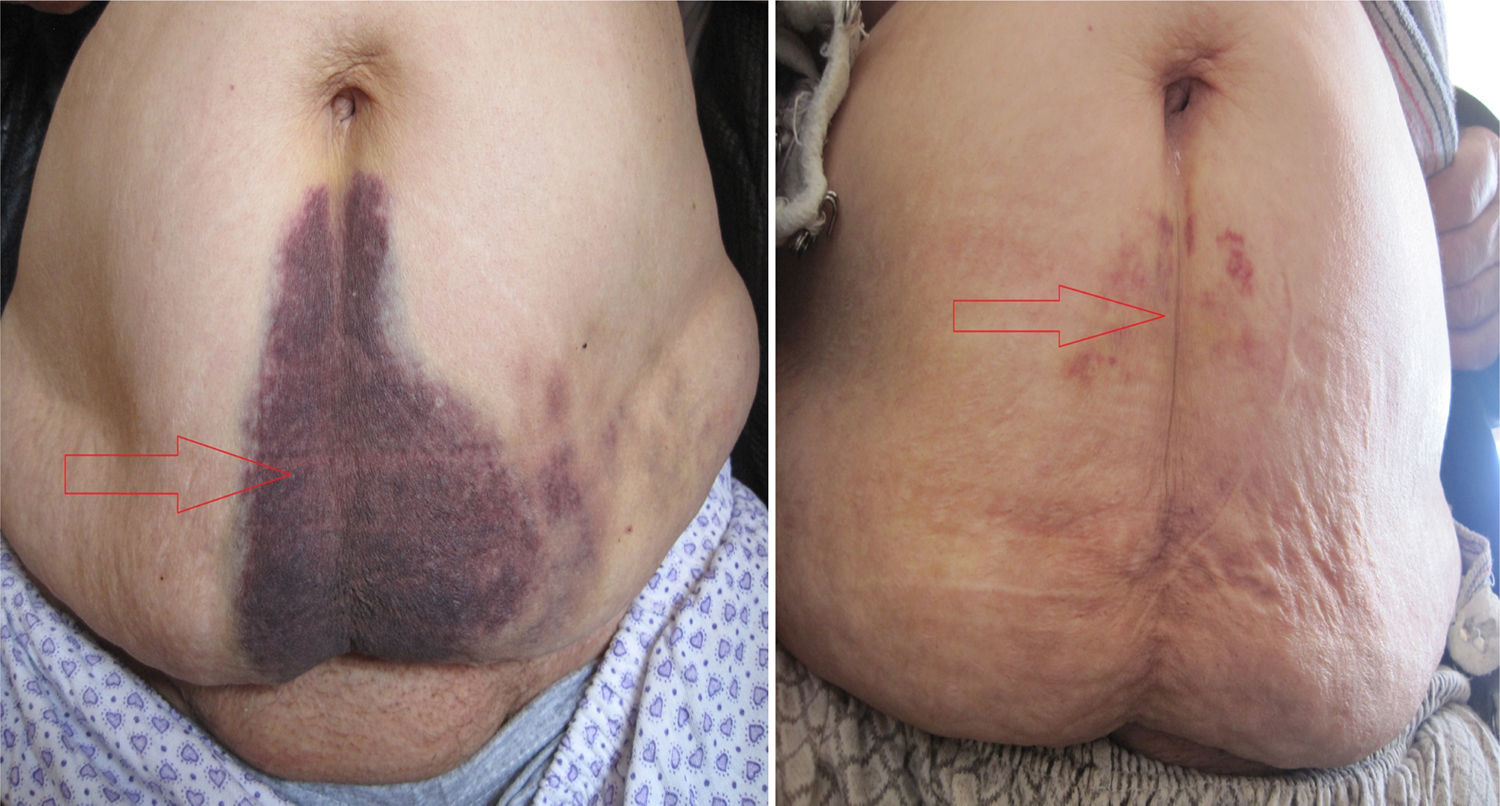
In the diagnosis of SRSH, US and/or CT may be used, as in our study. The US is beneficial for measuring the hematoma during the follow-up period. For a suspicious diagnosis, checking INR levels, and Carnett sign14 versus Fothergill's sign15 may be helpful. In Carnett sign, abdominal pain will diminish when the abdominal wall muscles tense. A positive sign shows abdominal wall pathologies, such as rectus hematoma; a negative sign is typical of intrabdominal pathologies such as acute appendicitis.16 In Fothergill's sign, palpable masses do not pass the midline and do not change position with rectus muscle flexion. A positive sign shows rectus hematoma. Anyfantakis et al.11 found that 85.7% of SRSH patients had Carnett sign and 57.1% had Fothergill sign; these rates are similar to what we found. All patients in our study were diagnosed 1–3h after admission, and treatment started immediately thereafter. The late signs of SRSH are periumblical ecchymosis (Fig. 4), which shows intraperitoneal rupture of vessels, and Gray Turner's sign (flank ecchymosis; Fig. 5), which shows extraperitoneal spreading of blood.17 Abdominal wall ecchymosis was found at a rate of 20% by Cherry et al. Ecchymosis, which can not be seen in the acute phase, may be prominent in the chronic phase.4 In our study, fast regression of ecchymosis was achieved with the help of local fibrinolytic agents such as chondroitin polysulphate (Fig. 4).
Except for Grade III injuries, surgical intervention is not advised. Instead of surgery, medical treatments such as bed rest, stopping anticoagulants, hydration, blood replacement when hemoglobin decreases, and fresh frozen plasma for warfarin overdose are suggested. Anyfantakis et al.11 achieved success with conservative treatment in 85.7%, which is similar to our rate. Surgery is advised only for hemodynamically unstable Grade III patients, with aggressive hydration and blood transfusion thereafter. However, in this patient group, the less invasive method of arteriography with selective embolization of the epigastric arteries must be performed prior to surgery because open surgical interventions remove the buffering effect of the hematoma, and therefore aggravate the hemorrhage.3 Open surgery can be applied when interventional radiology cannot control the hemorrhage, when the hematoma is infected, and when compartment syndrome is found.3 Arterial embolization is a safe and effective method. Rimola et al. used catherization for 12 patients and found no rebleeding during a 19±18 day follow-up period. While this study is the largest percutaneous embolization study to date, the number of patients was not large enough to compare embolization with surgery.18 McBeath et al. applied open surgery to SRSH patients for compartment syndrome and secondary renal failure. The hematoma was evacuated, the compartment syndrome ended, and renal failure was avoided.19 Meanwhile, measuring intra-abdominal pressure may help to distinguish patients who are candidates for surgery. In our study, one patient whose intra-abdominal pressure increased up to 20mm H2O was operated on. The hematoma, which spread to the intraperitoneum from the right rectus muscle, was evacuated, and intra-abdominal pressure decreased. No bleeding vessels were observed. The patient was taken to the ICU and was dead by the 6th postoperative day. She had a Grade III injury and hemodynamic instability. Grade I injuries resolve over a period of about one month, Grade II injuries resolve over 2–4 months, and Grade III injuries resolve after more than 3 months. Classification using CT may help to evaluate the prognosis. As expected, Grade III injuries has the poorest prognosis.
Reversing anticoagulation in patients who have an important reason for receiving it is a difficult dilemma of the present study. Considering the risks and benefits, after exact diagnosis, anticoagulant treatment was stopped immediately. The time at which anticoagulant treatment is restarted is critical. In our series, after obtaining a hemodynamically stable situtation, anticoagulant treatment was restarted. Clinical judgment is important in these cases. In the study by Cherry et al., rehematoma occured in 2 out of 41 patients after restarting anticoagulants.4 We found no new hematomas or increases in hematoma size. Clinicians must make decisions after evaluating the risks and the benefits of anticoagulant treatment.
This is the first and only study that is prospectively designed. Based on literature searches from Pubmed and Google Scholar, this study represents the third largest study in terms of number of patients (after Smithson et al.3 who included 24 patients and Dağ et al.20 who studied 22 patients).
ConclusionsSpontaneous rectus sheath hematoma is an emergent situation, and atypical presentation may delay diagnosis and treatment. An early diagnosis is important for a low mortality rate. Even though medical treatments are principally important, arterial embolization by interventional radiology, or more radical interventions such as surgery, may be required.
Conflict of InterestThe authors declare no conflict of interest
Please cite this article as: Isik A, Peker K, Soyturk M, Firat D, Yoruker U, Yilmaz I. Evaluación diagnóstica y tratamiento de pacientes con hematoma de la vaina de los rectos. Cir Esp. 2015;93:580–588.