Endoscopic retrograde cholangiopancreatography may be difficult in patients that have undergone Roux-en-Y gastric bypass. Due to the fact that prevalence of morbid obesity is increasing, and laparoscopic procedures for its treatment have increased, the incidence of biliary tract problems in patients of altered anatomy is also growing. We describe a laparoscopic technique to access the biliary tree by endoscope, through the excluded stomach.
En los pacientes a los que se les ha realizado una cirugía gástrica en Y-de-Roux, la realización de una colangiopancreatografía retrógrada endoscópica (CPRE) es muy dificultosa. Debido al aumento de la prevalencia de la obesidad mórbida y a la realización de cirugías laparoscópicas para su tratamiento, la incidencia de problemas biliares en pacientes con anatomía modificada también es creciente. Presentamos una técnica quirúrgica laparoscópica para acceder a la vía biliar por endoscopio, a través del estómago excluido.
Surgery for the treatment of obesity has progressively increased in the last 3 decades.1 The prevalence of this disease has grown drastically and in epidemic proportions throughout the world. Currently, this is a national healthcare problem in the United States as well as in many other countries.2
The first laparoscopic Roux-en-Y gastric bypass surgery for the treatment of obesity was performed by Wittgrove et al.3 in 1994. Since then, the number of laparoscopic procedures has increased year after year over the last decade,1 and it is now considered the gold standard treatment in the United States.4
There is a well-known association between weight loss and the formation of calculi.5 The treatment of choledocholithiasis can be a dilemma due to the anatomic alterations caused by the surgery, which makes endoscopic access difficult.
We present a surgical technique for transgastric gastroduodenoscopy and endoscopic retrograde cholangiopancreatography (ERCP) for patients who have undergone Roux-en-Y gastric bypass surgery for the treatment of obesity.
Case ReportThe patient is a 53-year-old woman with a personal history of COPD, Arnold–Chiari malformation and morbid obesity. She underwent biliopancreatic diversion due to her obesity, with no complications. Four years later, she was admitted for obstructive jaundice, which resolved spontaneously, and again one month later for symptoms of mild acute pancreatitis. Magnetic resonance cholangiopancreatography detected a slight dilatation of the intra- and extrahepatic bile duct, a 9-mm common bile duct and 5-mm lithiasis in the distal common bile duct 10mm from the papilla (Fig. 1). The case was discussed during a clinical session with the gastroenterology department, and the treatment agreed upon included laparoscopic cholecystectomy and transgastric ERCP.
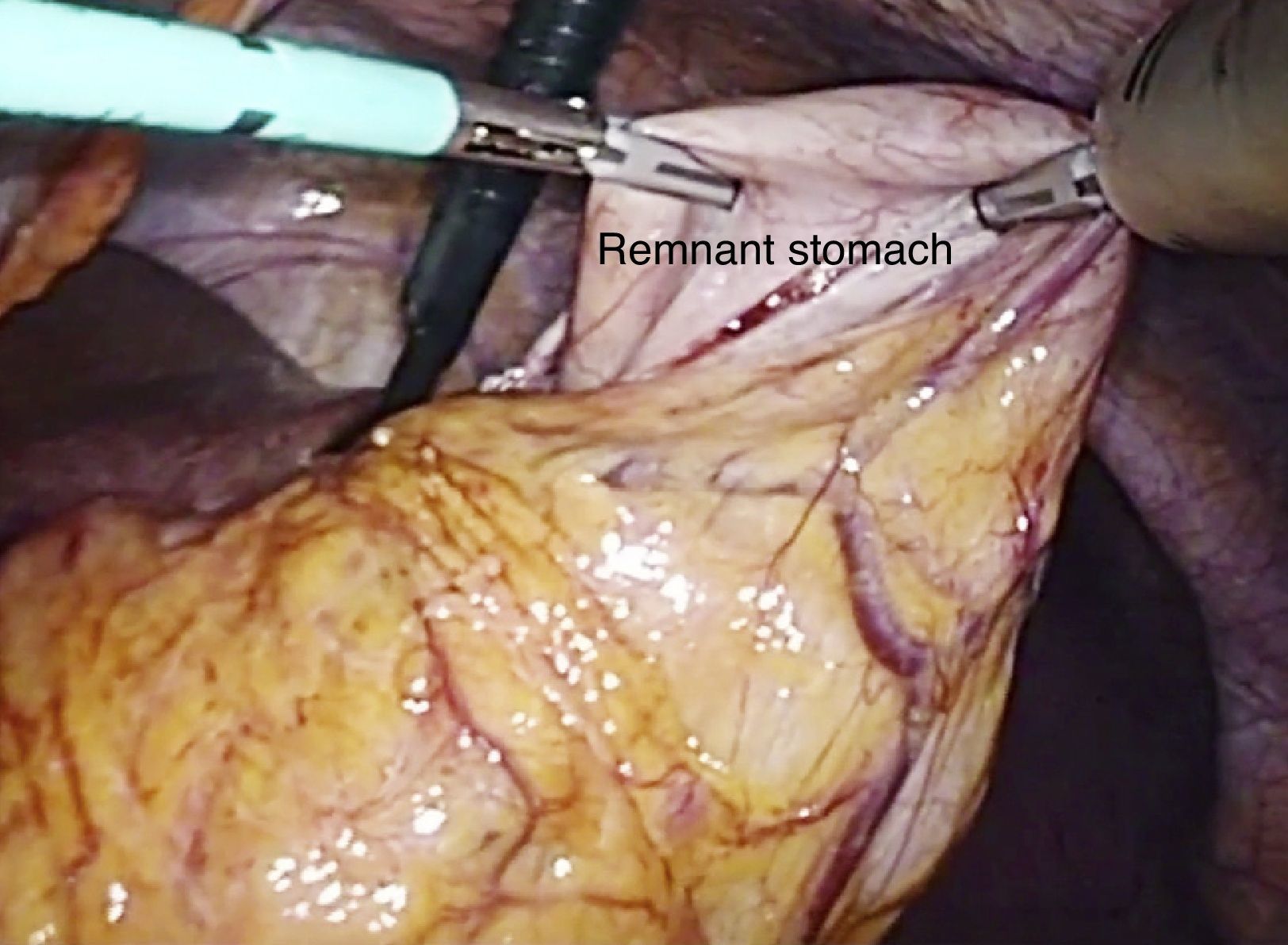
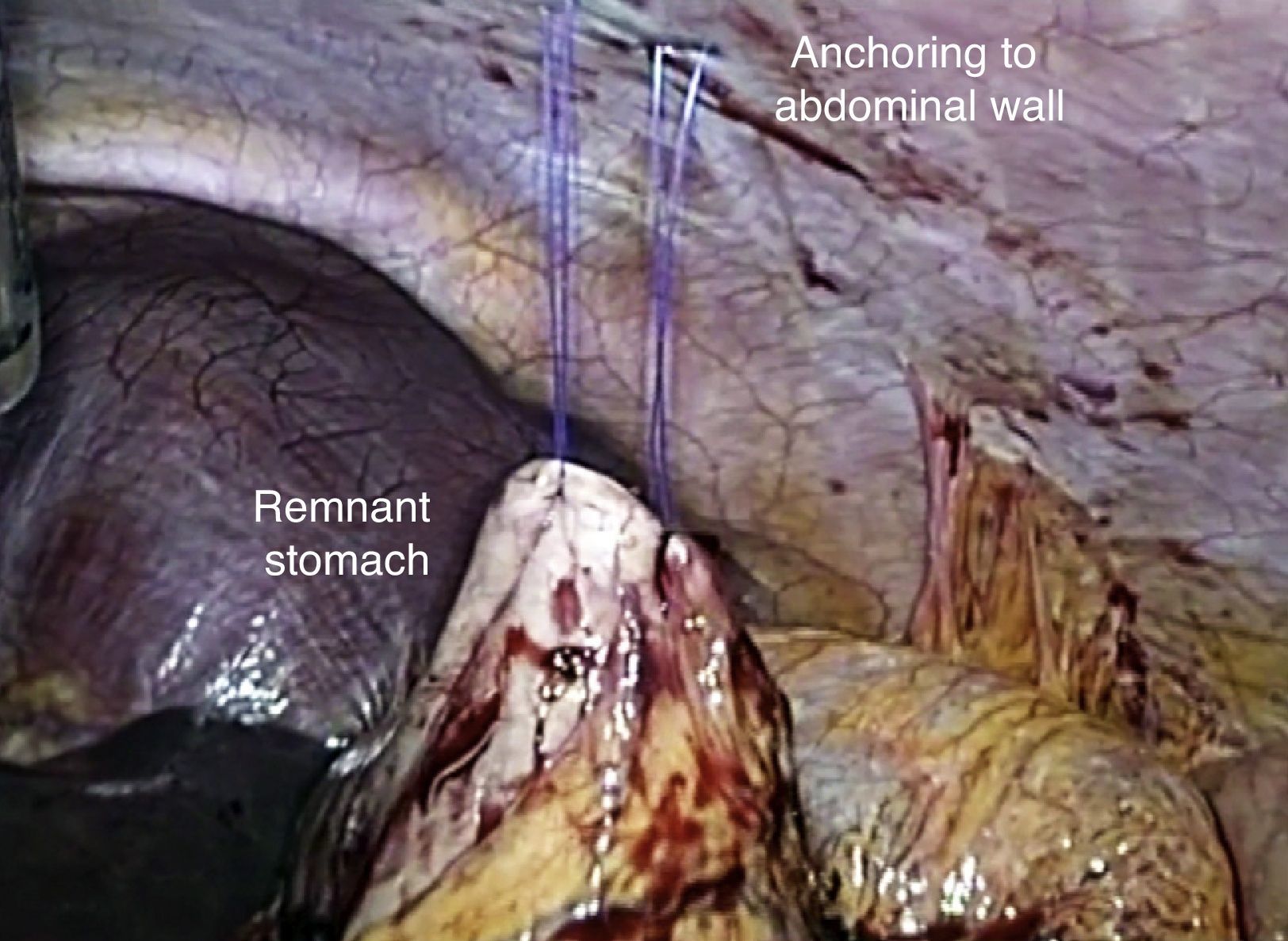
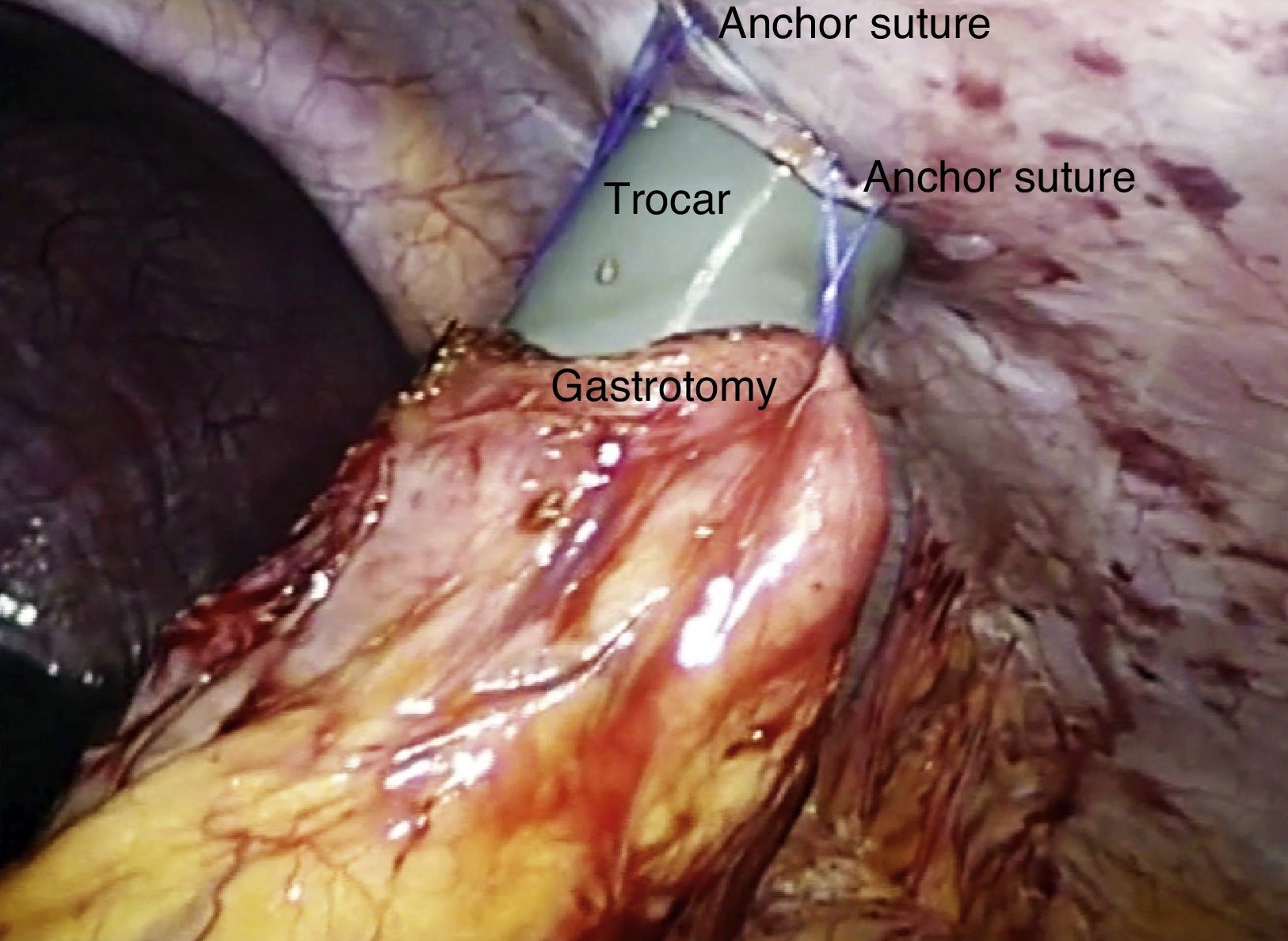
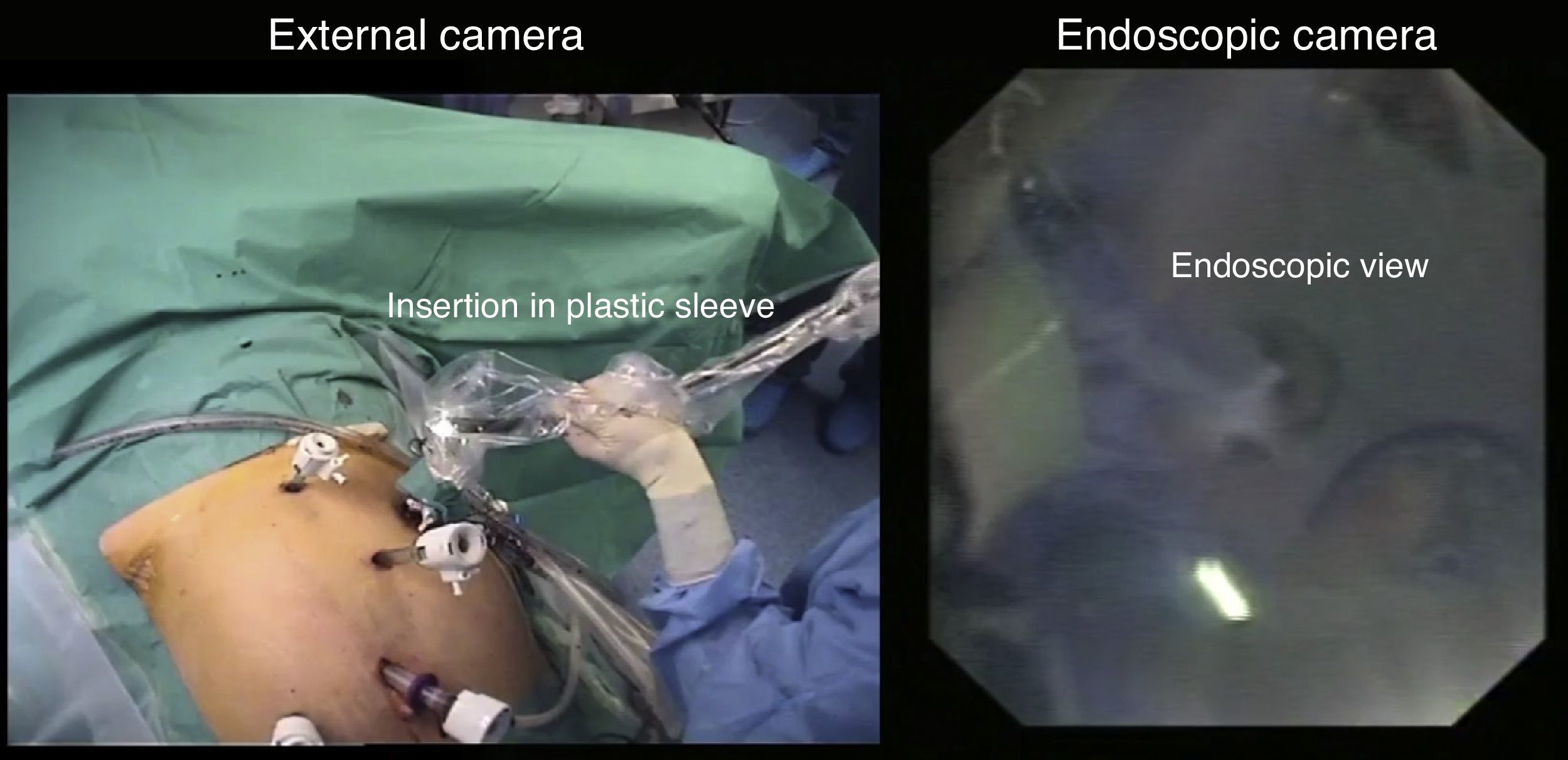
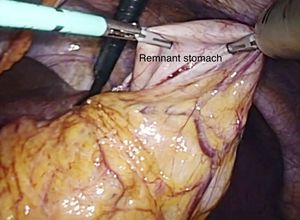
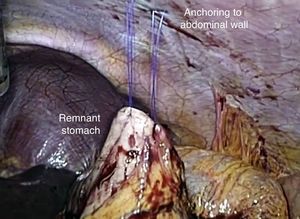
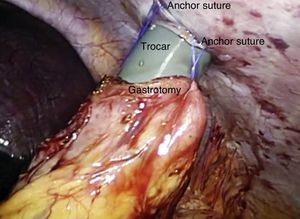
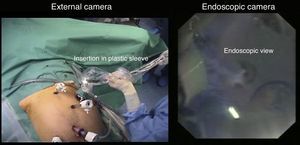
Surgical TechniqueUnder general anaesthesia and in supine decubitus (French position for laparoscopic cholecystectomy), pneumoperitoneum was initiated with an umbilical Hasson port. Three additional trocars were placed in the epigastrium and on the right and left clavicular midlines, under direct vision. After adhesiolysis and locating the alimentary loop, the stomach remnant was mobilised to select the location of the 15-mm trocar placement for the insertion of the endoscope (Fig. 2). Two calibre 2/0 monofilament sutures were introduced through the thickness of the abdominal wall to anchor the stomach (Fig. 3). The 15-mm trocar was placed between the 2 sutures. A gastric aperture was created and the 15-mm trocar was inserted in the stomach, then the sutures were tightened to achieve a seal (Fig. 4). The sterility of the surgical field was maintained with the placement of a bag in the trocar, prior to the insertion of the endoscope (Fig. 5). The surgeon directed the endoscope towards the pylorus, crossed it, and then reached the second portion of the duodenum to locate the papilla. To avoid distension of the bowel loops caused by the insufflation of air, an intestinal clamp was placed on the first jejunal loop after the Treitz angle.
At this point, the gastrointestinal endoscopist was able to proceed with ERCP as usual. The procedure was concluded and the gallstones were extracted without complications. Cholangiography confirmed that there were no residual calculi and the endoscope was withdrawn. Finally, cholecystectomy was done and the gastrotomy was closed with an endostapler, including the staples used for the gastropexy.
The patient was discharged 5 days later. Six months later, a follow-up magnetic resonance cholangiopancreatography demonstrated the bile duct with no residual lithiasis.
DiscussionFor patients who have previously undergone gastric surgery with Roux-en-Y reconstruction, therapeutic ERCP is a difficult procedure, especially when there is a long alimentary loop. The widespread acceptance of gastric bypass surgery for the treatment of obesity has resulted in an increase in the number of gastrointestinal endoscopies with altered digestive anatomy. These patients have a high prevalence of cholelithiasis during the first 6 months after bypass surgery of even more than 36%.6,7 Treatment with ursodiol has been used to prevent the formation of bile calculi, and it is recommended in these patients.8 However, complications can arise related with gallstones.
Traditional oral ERCP requires following the alimentary loop, crossing the bottom of the loop and ascending the biliopancreatic loop. The success rate ranges between 33% and 67% in expert hands.5,9 To increase this rate, a series of specialised techniques has been developed. Double-balloon oral ERCP is a feasible technique to study the biliopancreatic tree and gastric remnant. Nonetheless, this procedure presents a series of limitations: (1) the cannulation of the papilla is difficult; (2) movement along the intestinal loops can be problematic due to possible adherences; (3) there are few long-length accessories available on the market today for these procedures; and (4) a learning curve is involved.10 In spite of these limitations, there are published patient series with success rates for cannulation of up to 90%, including therapeutic interventions.11–13 However, retroperitoneal perforation occurred in 3.3%–7.7%.12,13 Although this technique can be effective, it requires equipment that is not universally available at all hospitals.
With these disadvantages, other endoscopic access pathways for the papilla have been proposed. The transgastric approach was originally described in 2002.14 Previously, there had been reports of upper gastrointestinal endoscopies through a gastrostomy in patients with benign oesophageal stenosis.15,16 This percutaneous approach is the least invasive and requires a gastrotomy that should be dilated by inserting a tube that should be substituted by a larger one every 2–3 weeks until the endoscope fits. One advantage of this procedure is that the ERCP can be done in the endoscopy room and with the patient in the anatomical position. Some of the disadvantages are that it cannot be used in emergency cases and that the patient needs to make several office visits to substitute the gastrostomy tubes. In the series by Martínez et al.17 all the patients were successfully treated with no complications derived from the gastrostomy.
The use of gastrotomy, in open as well as laparoscopic surgery, allows for the use of the endoscope early on and without the need to mature the stoma. In addition, another advantage to laparoscopy is the possibility to evaluate other causes of chronic abdominal pain, such as internal hernias. The disadvantages observed of the combination in 112 patients from the series published with this technique10,18–29 are associated with the access (3.6%) and include wound infection (n=1), haematoma of the abdominal wall (n=1) and problems caused by the closure of the gastrostomy (n=2). Additional complications (2.7%) related with the endoscopic procedure are post-ERCP pancreatitis (n=2) and retroperitoneal perforation (n=1).
There are some variations in the technique used. The number of ports can vary from 2 to 4, as in our case, depending on whether the patient had a prior cholecystectomy. Trocar placement also depends on the anatomy and previous interventions. Nonetheless, it is necessary to place a long 12 or 15mm trocar in the left upper quadrant to allow for the mobilisation of the gastric remnant and the creation of the gastrotomy. Selection of the site in the abdominal wall is outlined by the placement of 2 or 4 sutures that provide adequate retraction and exposure. The closure of this gastrotomy can be done by simple suture, double suture or endostapler. In patients with problems of oesophageal stenoses, a gastrostomy tube can be left in for feeding.
The transgastric ERCP technique is feasible and presents a low rate of complications related with the technique. The access to the stomach pouch is safe and can provide high rates of cannulation. Furthermore, the laparoscopic approach provides exploration of the abdominal cavity and the resolution of possible internal hernias.
Conflicts of InterestThe authors have no conflict of interests to declare.
We the authors would like to extend our thanks to the scientific committee of the 30th National Congress of Surgery for selecting this video for the “Best in Conference” section. We would also like to especially thank our families.
Please cite this article as: Molina Romero FX, Morón Canis JM, Llompart Rigo A, Rodríguez Pino JC, Morales Soriano R, González Argente FX. Colangiopancreatografía retrógrada endoscópica transgástrica por laparoscopia tras derivación biliopancreática. Cir Esp. 2015;93:594–598.