Lipomas are benign subepithelial tumors occurring throughout the gastrointestinal tract, most commonly in the colon and rarely in the duodenum.1–4 The majority are asymptomatic and found incidentally.3,4 Nevertheless, lipomas may cause symptoms as abdominal pain, change in bowel habits or bleeding.2–4 This case series, of which 2 cases were previously published as single case reports,5,6 aims to describe endoscopic resection of large gastrointestinal lipomas (Table 1). In all cases, endoloop (MAJ-254, Olympus) ligation was performed and, in all but one, complemented with unroofing of the lesion to allow a sample for histological analysis. Slightly different technical aspects detailed in each case were adopted to adjust to the characteristics of the lesion.
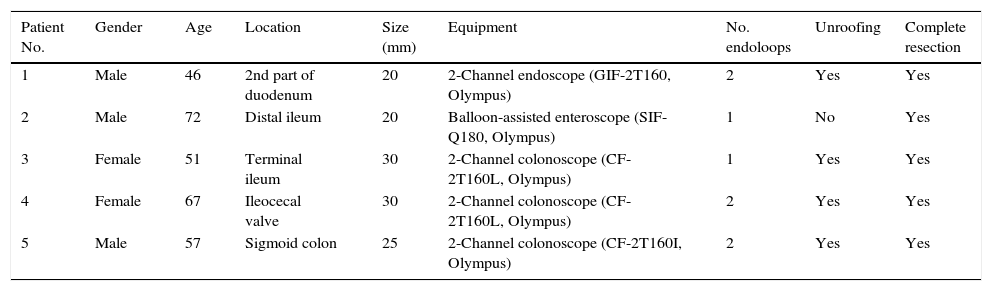
Summary of the characteristics of the patients, lesions and techniques performed.
| Patient No. | Gender | Age | Location | Size (mm) | Equipment | No. endoloops | Unroofing | Complete resection |
|---|---|---|---|---|---|---|---|---|
| 1 | Male | 46 | 2nd part of duodenum | 20 | 2-Channel endoscope (GIF-2T160, Olympus) | 2 | Yes | Yes |
| 2 | Male | 72 | Distal ileum | 20 | Balloon-assisted enteroscope (SIF-Q180, Olympus) | 1 | No | Yes |
| 3 | Female | 51 | Terminal ileum | 30 | 2-Channel colonoscope (CF-2T160L, Olympus) | 1 | Yes | Yes |
| 4 | Female | 67 | Ileocecal valve | 30 | 2-Channel colonoscope (CF-2T160L, Olympus) | 2 | Yes | Yes |
| 5 | Male | 57 | Sigmoid colon | 25 | 2-Channel colonoscope (CF-2T160I, Olympus) | 2 | Yes | Yes |
A 46-year-old man was referred for endoscopic resection of a large lipoma diagnosed incidentally in a computed tomography (CT). Although asymptomatic, the patient asked for resection regarding the dimension of the lesion. Upper endoscopy revealed a pseudopedunculated lesion measuring 20mm, in the duodenum. With a double-channel endoscope, an endoloop was previously placed externally to a foreign body forceps which grasp and retract the lesion, while the endoloop was subsequently tightened around the base of the lesion. A second endoloop was positioned using the “loop-over-loop” technique, in which the first endoloop was mobilized with a foreign body forceps guiding the placement of the second endoloop in the base of the lesion, immediately beneath the first endoloop. After endoscopic ligation, a snare was used to unroof the top of the lesion. A follow-up endoscopy performed one month later revealed a regular scar with no residual lesion.
A 72-year-old man was referred to our department with a chronic history of episodic abdominal pain and vomiting. A CT enterography was performed and revealed a large pedunculated lesion resembling a lipoma in the distal ileum. The patient underwent retrograde single-balloon enteroscopy6 that revealed a yellowish pedunculated subepithelial lesion covered with normal mucosa in the distal ileum, which was ligated with an endoloop around the false pedicle of the lesion. The patient underwent a follow-up enteroscopy one month later, which revealed complete resection of the lesion. After a year of follow-up the patient remained asymptomatic.
A 51-year-old woman presented with a 6-month history of episodic abdominal pain and chronic diarrhea, which was presumed to be caused by the ball-valve effect of a large lipoma in the terminal ileum. As the manipulation of the lipoma resulted in consecutive retractions to the terminal ileum, a grasp-to-retract technique was employed using a 2-channel therapeutic colonoscope.7 While a forceps pulled and stabilized the lipoma at the ascending colon, a detachable snare, previously positioned over the forceps, was placed around the base of the pseudopedunculated lesion. The endoloop ligation was complemented with unroofing of the lesion. Two months after resection, the patient was asymptomatic and a regular scar was confirmed.
A 67-year-old woman underwent an endoscopic resection of a large asymptomatic lipoma of 30mm at the ileocecal valve (Video 1), due to the dimensions of the lesion and patient's informed request. With a 2-channel therapeutic colonoscope, the lesion was stabilized with a foreign body forceps while an endoloop was applied and tightened around its base. Subsequently, a second endoloop was positioned using the “loop-over-loop” technique. Finally, unroofing through resection of the top of the lesion with a snare was performed. A follow-up endoscopy performed one month later revealed a regular scar with no residual lesion.
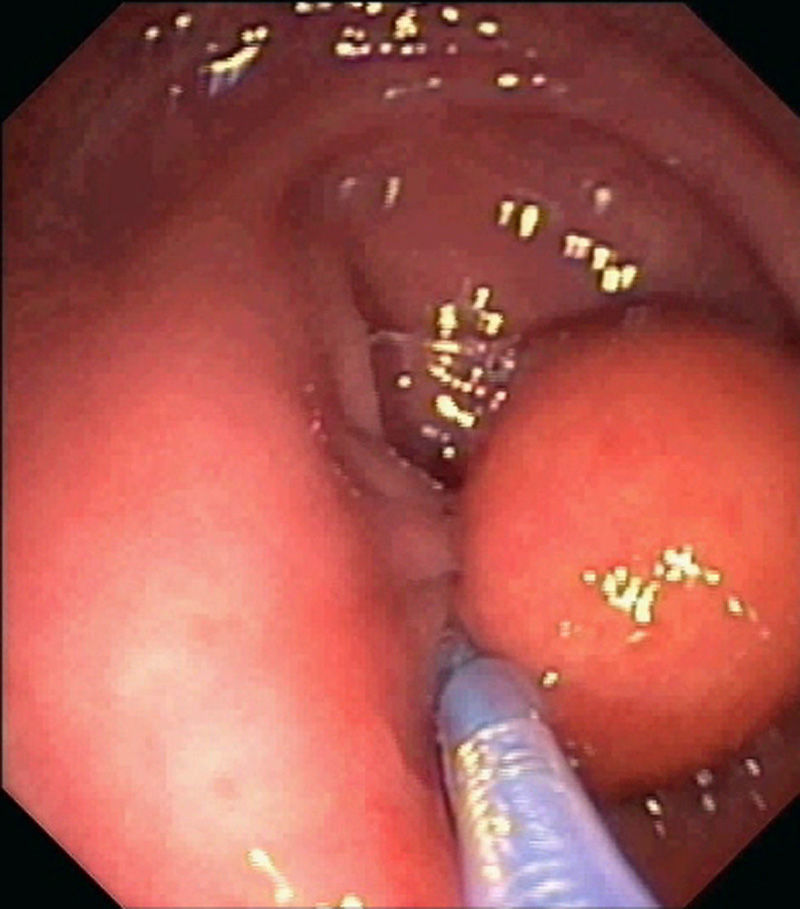
A 57-year-old man underwent endoscopic resection of a pseudopedunculated subepithelial lesion of 25mm at the sigmoid colon, regarding the dimensions of the lesion and preference of the patient to remove the lesion. With a double-channel colonoscope, a detachable snare was a tightly applied around the base of the lesion (Fig. 1) and another endoloop was further placed around the base of lesion using the “loop-over-loop” technique. Finally, unroofing was performed. Endoscopic follow-up assessment performed a month after the resection, revealed a regular scar with no residual lesion.
The main reasons described in previous case series for resection of gastrointestinal lipomas include symptomatic lesions or asymptomatic lesions larger than 20mm which may develop symptoms or complications, namely intestinal obstruction, invagination, perforation or bleeding.4,7 Nevertheless, larger asymptomatic lesions may be removed after discussion of the risks and benefits with the patient.
Endoscopic resection of lipomas using cautery snare polypectomy is associated with a high risk of bleeding and perforation, as fat tissue conducts electrosurgical current less efficiently and higher amounts of energy are necessary to resect lesions.2,4,7 Conversely, endoloop ligation has a neglectable risk of perforation by promoting slow mechanical transection of large pseudopedunculated lipomas.2,4–6,8,9 Moreover, careful selection of the lesions is crucial to ensure a safe resection, as endoscopic ligation should not be performed on broad based or sessile lipomas.7 In our series, all the lipomas were pseudopedunculated and no complications were recorded.
The main drawbacks of endoloop ligation are the difficulty in catching the lipoma with the detachable snare, the potential need of further procedures to remove the lesion and lack of a specimen for histological diagnosis. These difficulties may be obviated using a grasping forceps to place the lipoma deep inside the endoloop, using two endoloops to reinforce the ligation and performing the unroofing technique, respectively.2–4,8,10 All patients were successfully treated with only one endoscopic session. Moreover, despite the impossibility of confirm complete resection of the lesion, unroofing allowed partial histological evaluation of the specimen corroborating the endoscopic diagnosis.
Conflict of interestsAuthors declare no conflict of Interests for this article.