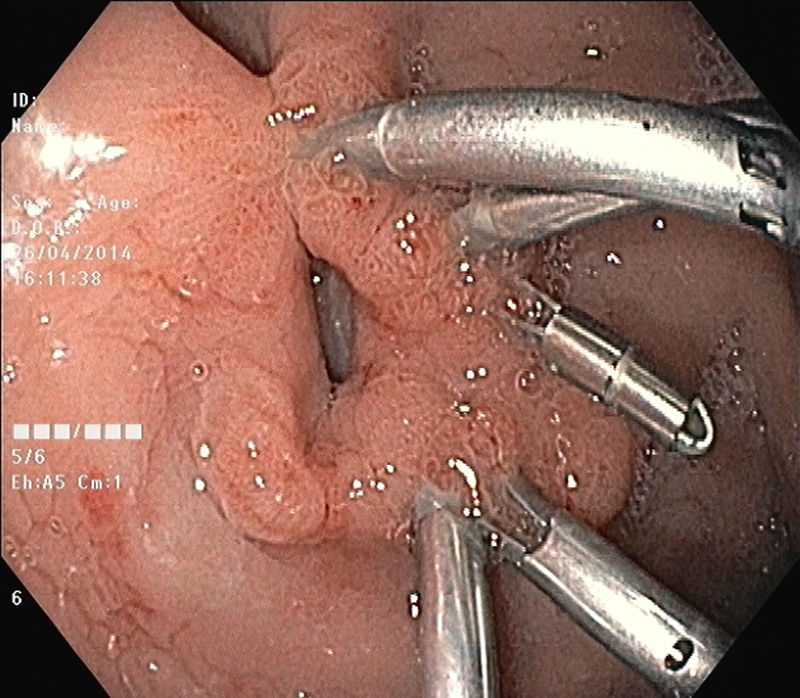
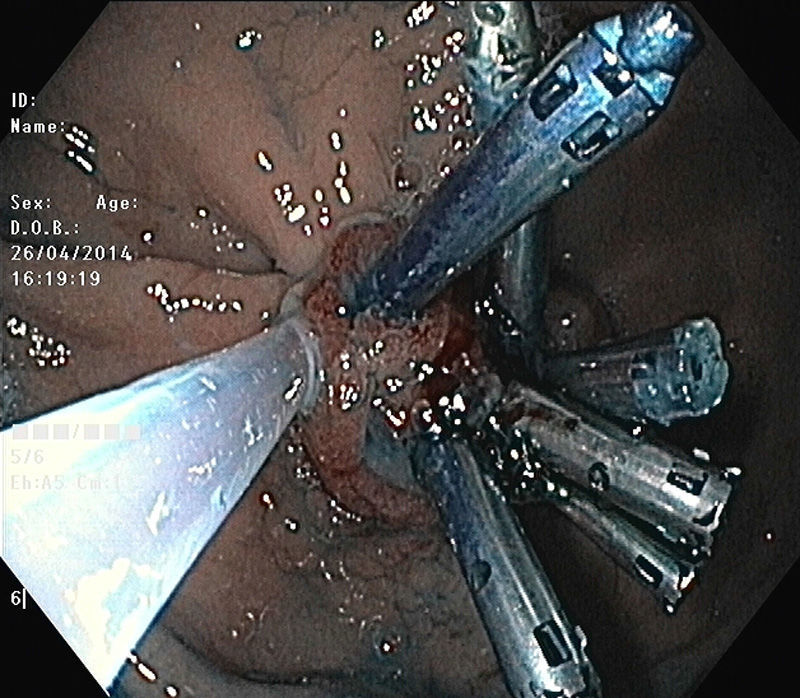
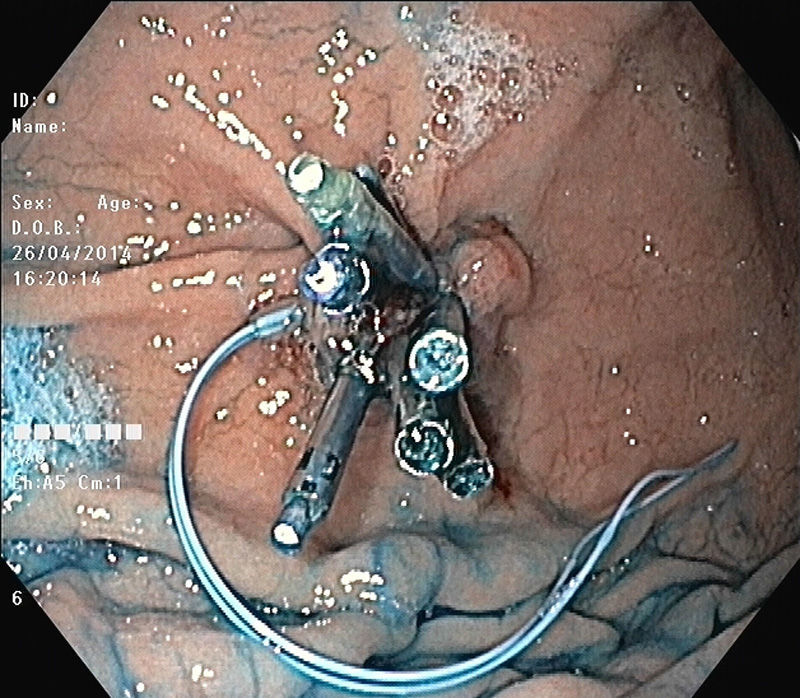
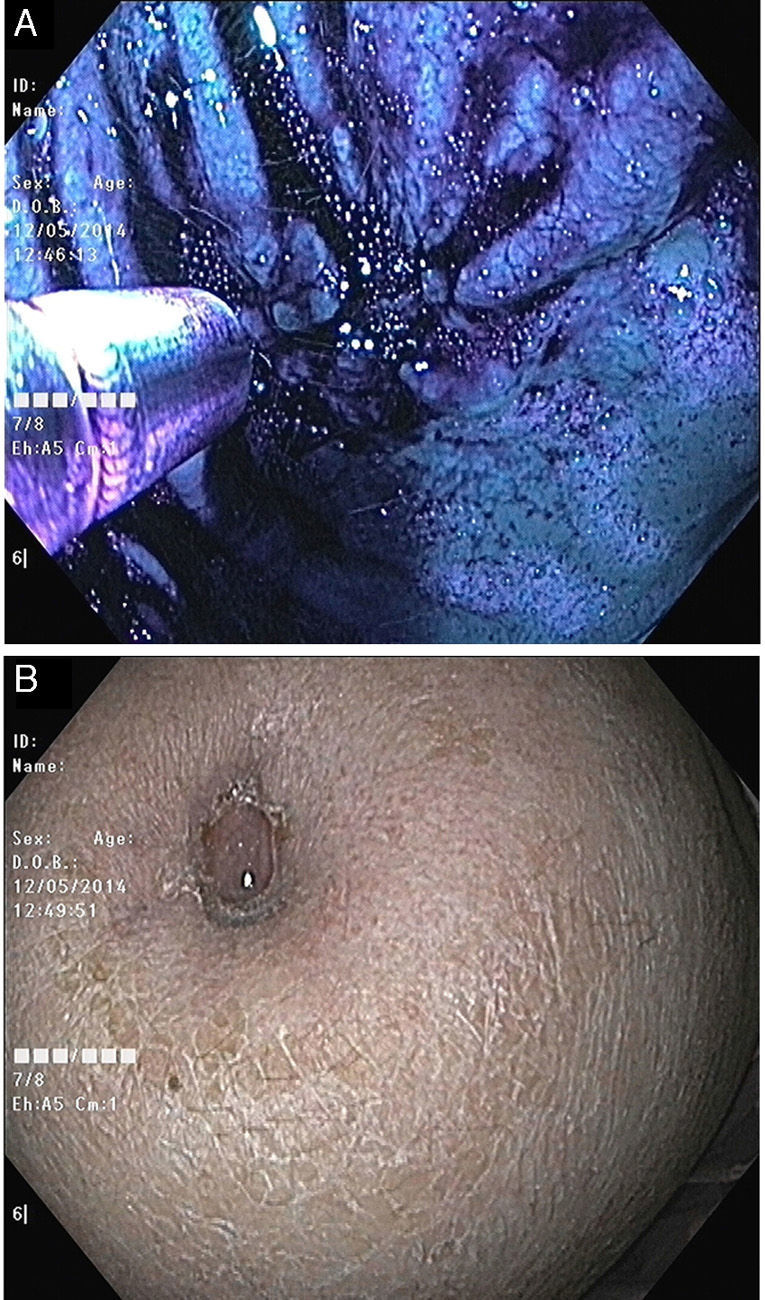
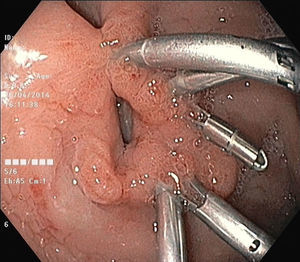
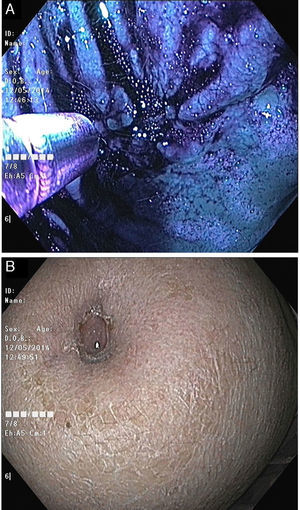
The authors present a case of a 68-year-old woman with end-stage metastatic breast cancer and biphosphonate-related osteonecrosis of the jaw with a chronic gastrocutaneous fistula which persisted a month after removal of a 24 Fr percutaneous endoscopic gastrostomy (PEG) tube. Conservative management with intravenous antibiotics, regular wound cleaning, high-dose proton pump inhibitor and a nasojejunal tube for enteral feeding was instituted. After two unsuccessful attempts to close the gastric defect with endoclips, a third endoscopy was performed revealing extravasion of methylene blue through the gastric orifice with the previously placed endoclips (Fig. 1). After closure of the gastric orifice with additional endoclips, a tulip-bundle technique was performed. In this technique an endoloop snare (MAJ-254; Olympus, Japan) was placed over the endoclips resulting in closure of fistulous tract (Video). External digital pressure of the stoma enabled proper positioning of the endoloop deeper below the endoclips, which was then tightened around the endoclips (Fig. 2) closing the gastric orifice (Fig. 3). A follow-up endoscopy performed half a month later revealed complete closure of the gastric defect with no extravasion of methylene blue (Fig. 4A) to the skin (Fig. 4B).
Although PEG is a safe and efficient procedure for enteral nutrition, some complications may occur, including peristomal infection, leakage and chronic gastrocutaneous fistula.1–3
The tulip-bundle technique has a range of applications including hemostasis and closure of perforations and fistulae.3–6 The tulip-bundle technique may represent a good alternative for closure of chronic gastrocutaneous fistula,3 which is particularly useful in patients with multiple comorbidities as our patient.