We present the case of a 70-year-old male patient with a history of diabetes mellitus, diverticulitis, with an abdominal aortic endoprosthesis fitted and chronic kidney disease, who attended the Accident and Emergency department due to sharp abdominal pain in the right hypochondrium after a haemodialysis session. There was no fever, vomiting or other clinical symptoms by system.
On examination he presented a soft, depressible abdomen with abdominal guarding in the right hypochondrium and a positive Murphy’s sign. The examination was supplemented with general blood tests, which showed leucocytosis with neutrophilia, elevated C-reactive protein and slightly elevated transaminases.
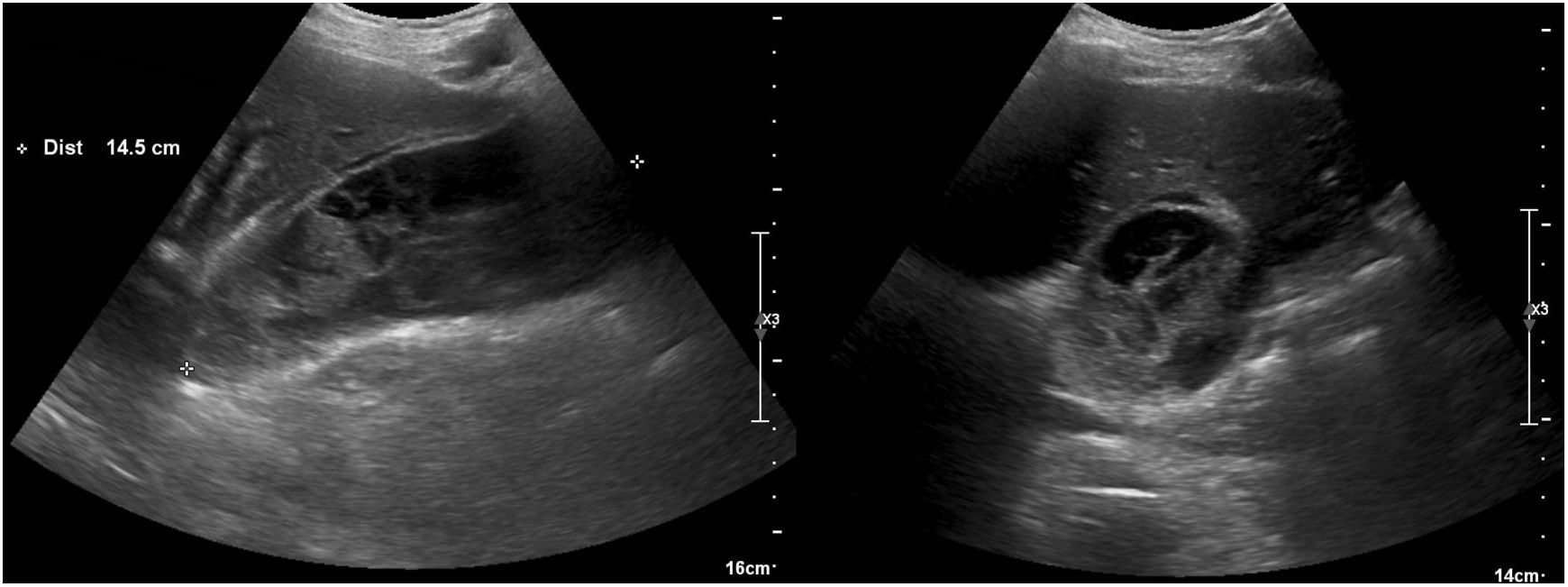
The ultrasound revealed a distended gallbladder of some 15 × 6 cm, with abundant heterogeneous intravesicular content without dilation of the bile duct (Fig. 1).
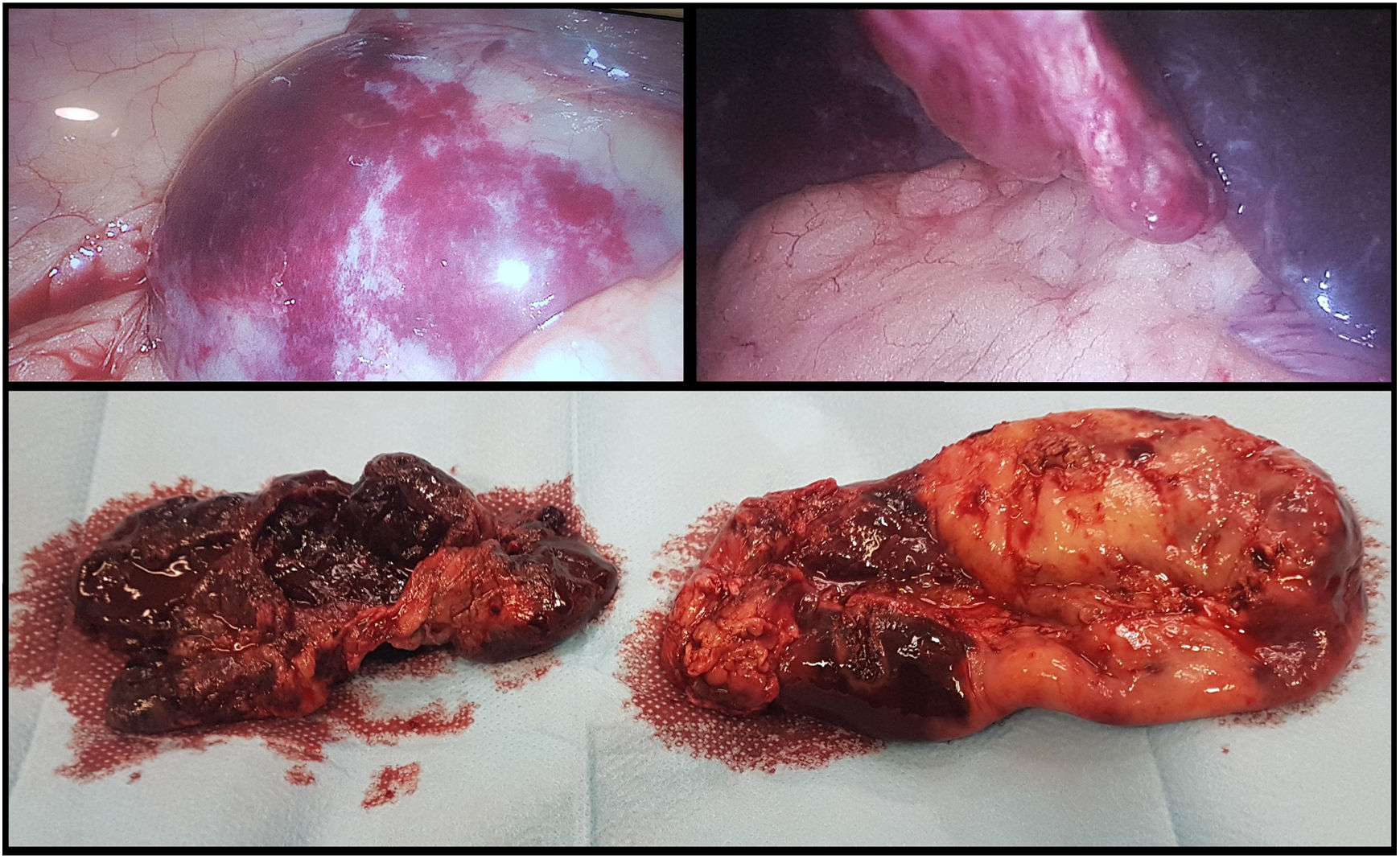
Given the persistence of pain in spite of analgesia and the suspicion of acute cholecystitis, the decision was made to perform a laparoscopic cholecystectomy, in which a necrohaemorrhagic gallbladder with intravesical clots was found (Fig. 2).
Patients on haemodialysis have a higher risk of bleeding due to a deficiency in platelet aggregation secondary to uraemia and the use of anticoagulants and low-molecular-weight heparins in haemodialysis treatments.1,2 When they present with abdominal pain, we must consider various less common haemorrhagic processes in the differential diagnosis, such as haemobilia or necrohaemorrhagic cholecystitis,3 as occurred in our case.
Please cite this article as: Gomez Sanchez J, Garde Lecumberri C, Gonzalez Puga C, Miron Pozo B. Colecistitis necrohemorrágica tras terapia renal sustitutiva. Gastroenterol Hepatol. 2019;42:500–501.