El síndrome de apneas-hipoapneas del sueño (SAHS) es frecuente en pacientes hipertensos e influye en una mayor incidencia de morbimortalidad cardiovascular. El objetivo es conocer cuál es el perfil clínico de hipertensos con SAHS en comparación con hipertensos sin SAHS para conocer qué variables han de permitir orientar su cribado desde Atención Primaria.
MetodologíaEstudio observacional retrospectivo descriptivo de casos (hipertensos con SAHS) y controles (hipertensos sin SAHS), realizado en un centro de salud urbano. A partir del registro informatizado del centro se seleccionó a los pacientes diagnosticados de SAHS e hipertensión mayores de 30 años. Por cada caso se obtuvo, aleatoriamente y apareando por edad y sexo, hipertensos sin SAHS.
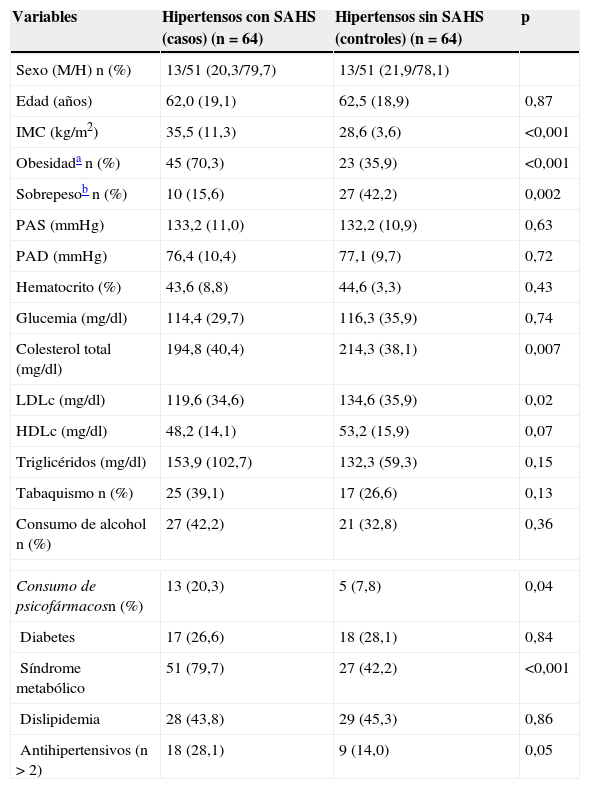
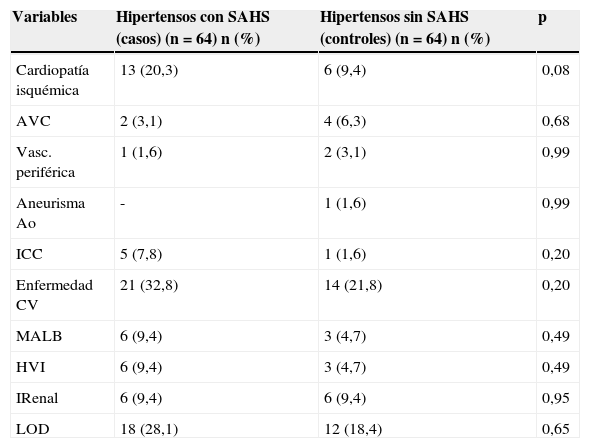
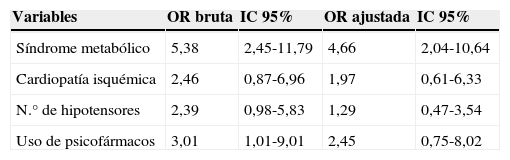
ResultadosSe seleccionaron 64 casos y 64 controles. En el análisis bivariante destacaba un mayor IMC (34,3±12,8 vs. 28,6±3,6), predominio de obesidad (70,3 vs. 35,9%), síndrome metabólico (77,3 vs. 42,2%), consumo de psicofármacos (19,7 vs. 7,8%) y antihipertensivos (26,5 vs. 14,0%), cardiopatía isquémica (20,3 vs. 9,4%) en el grupo de casos respecto al grupo controles (p<0,05 para todas las variables). El análisis multivariante mostró que únicamente presentar síndrome metabólico se relacionaba con la presencia de SAHS en hipertensos (OR 4,65; IC 95%: 2,03-10,64; p<0,001).
ConclusionesEn hipertensos atendidos en Atención Primaria se debería realizar el cribado de SAHS si presentan criterios de síndrome metabólico.
Sleep apnea hypopnea syndrome (SAHS) is frequent in hypertensive patients and plays a role in a greater incidence of cardiovascular morbidity-mortality. This study aims to know the clinical profile of hypertensive patients with SAHS compared to hypertensive patients without SAHS to know which variables should be used to orient their screening from primary care.
MethodologyAn observational, descriptive, retrospective study of cases (hypertensive patients with SAHS) and controls (hypertensive patients without) was performed in an urban health care center. Based on a computerized registry of the site, patients diagnosed of SAHS and hypertension over 30 years of age were selected. For each case, one control case of hypertensive patients without SAHS paired by age and gender was randomly obtained.
ResultsA total of 64 cases and 64 controls were selected. Standing out in the bivariate analysis were greater BMI (34.3±12.8 vs. 28.6±3.6), predominance of obesity (70.3 vs. 35.9%), metabolic syndrome (77.3 vs. 42.2%), consumption of psychopharmaceuticals (19.7 vs. 7.8%) and anithypertensive drugs (26.5 vs. 14.0%), ischemic heart disease (20.3 vs. 9.4%) in the case group versus control group (P<.05 for all the variables). The multivariate analysis showed that only the presence of metabolic syndrome was related with the presence of SAHS in hypertensive patients (OR 4.65; 95% CI: 2.03-10.64; P<.001).
ConclusionsScreening for SAHS should be performed in hypertensive patients seen in primary care if they have metabolic syndrome criteria.
Artículo
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora