Young adults with attention deficit hyperactivity disorder (ADHD) are at high risk of substance use (SU). The aims of the current study were: 1) to examine the use of alcohol, tobacco, marijuana and other illegal drugs by adults with and without ADHD; 2) to compare the oppositional, conduct, anxiety, depression, sleep and antisocial personality symptoms of ADHD adults with SU and ADHD adults without SU; 3) to examine the ability of ADHD symptoms and conduct problems to predict SU. A total of 93 young adults, 43 without ADHD and 50 with a childhood diagnosis of ADHD, who were part of the Spanish sample of the Multicenter ADHD Genetics (IMAGE) study, collaborated in a follow-up evaluation 10.1 years later. ADHD participants were divided into two groups based on the presence or absence of SU. Statistically significant differences were found between young adults with and without ADHD in their use of tobacco, marijuana and alcohol. A statistically significant association was also shown between externalization problems and a greater risk of SU. Conduct problems, to a greater degree than ADHD symptoms, affect SU in ADHD adults.
Los jóvenes con trastorno por déficit de atención con hiperactividad (TDAH) tienen un elevado riesgo de uso de sustancias (US). Los objetivos del presente trabajo fueron: 1) analizar el consumo de alcohol, tabaco, marihuana y otras drogas ilegales en adultos con y sin TDAH; 2) comparar a los adultos con TDAH con y sin US en oposicionismo, problemas de conducta, ansiedad, depresión, sueño y personalidad antisocial; 3) determinar la capacidad de la sintomatología de TDAH y de los problemas de conducta para predecir el US. Noventa y tres jóvenes adultos, 43 sin TDAH y 50 con diagnóstico de TDAH en la infancia que participaron en el estudio Multicenter ADHD Genetics (IMAGE) colaboraron en una evaluación de seguimiento 10.1 años después. Los participantes con TDAH se dividieron en dos subgrupos según presencia o ausencia de US. Los jóvenes con y sin TDAH se diferenciaron significativamente en consumo de tabaco, marihuana y alcohol. Se constató una relación significativa entre los trastornos de conducta y US en adultos TDAH. Los problemas de conducta más que los síntomas de TDAH influyen en el US de adultos con TDAH.
The accumulated research has shown that attention deficit hyperactivity disorder (ADHD) symptoms extend throughout life in up to 60% of the cases (Willcutt, 2012). Their persistence has been associated with functional impairment in psychosocial, educational, professional and family functioning (Biederman, Petty, Woodworth et al., 2012). In addition, compared to adults without ADHD, adults with ADHD experience higher levels of anxiety disorders, mood disorders, conduct disorders and antisocial personality disorder (Hesson & Fowler, 2015; Miranda, Berenguer, Colomer, & Roselló, 2014; Nogueira et al., 2014), as well as an increased risk of abuse/dependence on nicotine, alcohol, marijuana, cocaine, and other unspecified substances (Breyer, Lee, Winters, August, & Realmuto, 2014; van Emmerik-van Oortmerssen et al., 2012). Of the core ADHD symptoms, hyperactivity/impulsivity generally shows more robust and consistent relations with dependence on various illicit substances than inattention which has only been associated with alcohol use (Capusan, Bendtsen, Marteinsdottir, Kuja-Halkola, & Larsson, 2015; Roberts, Peters, Adams, Lynam, & Milich, 2014).
In addition, the strength of the association between substance use (SU) and ADHD varies. Thus, among adolescents with ADHD, about 19%-46% smoke cigarettes, whereas only 10–24% of non-ADHD individuals smoke (Burke, Loeber, White, Stouthamer-Loeber, & Pardini, 2007). Moreover, cigarette smoking is a risk factor for other substance misuse. In fact, adolescents with ADHD are 4 to 5 times more likely than controls to escalate to heavy cigarette and marijuana use after trying these substances once (Biederman, Petty, Hammerness, Batchelder, & Faraone, 2012).
Another interesting issue is the analysis of the influence of other psychopathologies, including comorbid externalizing and internalizing problems, in predicting substance abuse/dependence. Some findings indicate that conduct disorder (CD) and oppositional defiant disorder (ODD) are positively associated with SU in ADHD subjects. Thus, Symmes et al. (2015) compared nicotine use throughout young adulthood in three groups, based on childhood status: ADHD only, ADHD externalizers and control groups. Results indicated that at all three data collection points, individuals with childhood ADHD plus an externalizing disorder reported higher nicotine use compared to the ADHD group without an externalizing disorder and the comparison group of non-ADHD youth. The group differences were significant, even after controlling for possible confounding variables (age, gender, and current treatment with psychostimulant medication).
Along the same lines, Brinkman, Epstein, Auinger, Tamm and Froehlich (2015) found that adolescents with an ADHD+CD diagnosis had a 3- to 5-fold increase in the likelihood of using tobacco and alcohol, and initiated use at a younger age, compared to those with neither disorder. Having ADHD alone was associated with an increased likelihood of tobacco use, but not alcohol use. Hyperactivity-impulsivity symptom counts were not independently associated with any outcome, while every symptom increase in inattention increased the likelihood of tobacco and alcohol use by 8-10%.
A meta-analysis by Serra-Pinheiro et al. (2013) also concluded that the risk of SU in individuals with ADHD could be explained to a large degree by the frequent presence of ODD and CD. However, some studies have shown a direct link between ADHD and SU, even when CD is controlled (Arias et al., 2008), so that ADHD would be an independent risk factor for substance use disorder, although the ADHD+CD combination would increase the risk.
Less attention has been devoted to research on the contribution of mood or anxiety disorders to substance disorder vulnerability in ADHD. The systematic examination carried out by Wilens and colleagues (2011) concluded that, despite relatively high rates of major depressive (42%-52%) and anxiety (23%-24%) disorders at baseline (ages 6-17), neither of these comorbidities predicted the overall category of SU at the 10-year follow-up. In fact, mood disorders predicted drug-use disorders, but not overall SU, alcohol use disorders, or cigarette smoking. These findings partly supported the idea that depression was not associated with SU.
The purpose of this study is to increase the knowledge about ADHD when it co-exists with addictive behaviors that have an impact on the lives of the individuals affected and the people around them. Despite a growing body of literature, it is necessary to identify more precisely the substances consumed by adults with a childhood diagnosis of ADHD combined-subtype and explore the relationship of these use patterns with the comorbidities associated with the disorder. The specific aims of the current study were:
- 1)
To determine the use of alcohol, tobacco, marijuana and other illegal drugs in adults with ADHD compared to adults without ADHD (no ADHD).
- 2)
To compare adults with ADHD plus SU and adults with ADHD without SU on problems commonly associated with the disorder, that is, oppositional defiant disorder, conduct disorder, anxiety disorder, depression, sleep disorder, and antisocial personality disorder.
- 3)
To investigate the capacity of ADHD symptoms and externalizing problems (ODD and CD) symptoms to predict the use of alcohol, tobacco, marijuana and other illegal drugs in adults with ADHD.
We predicted that the prevalence of SU in ADHD young adults would be higher than in the comparison group. We also predicted that ADHD young adults with SU could experience more mental disorders than ADHD young adults without SU. Finally, we hypothesized that ADHD symptoms co-occurring with CD and ODD would be associated with a greater risk of SU.
MethodParticipantsThe sample was composed of 93 young adults, 43 without ADHD (no ADHD) and 50 with ADHD, who were part of the Spanish sample of the Multicenter ADHD Genetics (IMAGE) study. When the ADHD participants were first evaluated between 2003 and 2006, were between 5 and 16 years old and presented a clinical diagnosis of ADHD combined-subtype, according the international diagnostic criteria for this subtype from the revised fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR; American Psychiatric Association, APA, 2000) (see description of the sample in Müller et al., 2011). Fifty of 81 subjects from original sample of IMAGE study participated in the current follow-up evaluation, which took place on average 10.1 years later, between 2013 and 2015. Fourteen subjects (17%) did not participate because of loss of their localization (changes in the family address or contact telephone), 7 participants declined to attend to the evaluations (9%), and 10 participants were less than 17 years old (12%).
The ADHD group had between 17 and 24 years (M=18.7, SD=1.4) and had an IQ between the normal range (M=104.21, SD=15.41). Additionally, 65% of these participants according to the subjects themselves and 60% according to the observer had 5 or more ADHD symptoms of inattention and/or hyperactivity/impulsivity considering the 5 symptoms cut-off based on the recent version of the DSM (DSM-5; APA, 2013) criteria for ADHD in adults.
The 43 participants without ADHD were not part of the previous sample and they were selected according to the criteria of the National Institute of Statistics of Spain for the distribution of the population, based on their grade level and employment status in the age range of 17-24 years. We contacted these individuals by disseminating information about this research project in Universities, vocational training schools, and secondary schools and their participation was voluntary. They also had to meet the following criteria: 1) No history of significant problems of inattention or hyperactivity / impulsivity; 2) T scores below 65 on both the DSM-IV inattention and hyperactivity/impulsivity subscales of the CAARS observer and self-report versions; 3) Absence of neurological disorders, sensory or motor deficits (paralysis, deafness, blindness), autism or psychosis; and 4) an IQ equal to or greater than 70. Eight participants were removed for meeting 5 or more symptoms of inattention or hyperactivity/impulsivity according to the DSM-5 criteria. The group without ADHD had a mean age of 19.26 (SD=1.83) and a mean IQ of 103.02 (SD=11.57) (see Table 1).
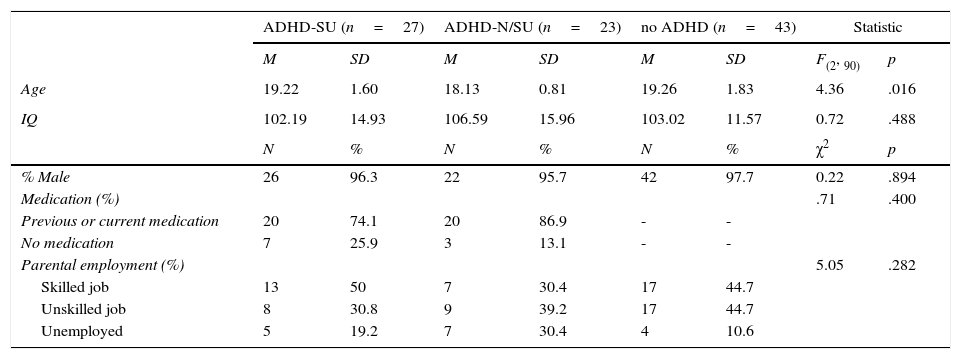
Sociodemographic characteristics.
| ADHD-SU (n=27) | ADHD-N/SU (n=23) | no ADHD (n=43) | Statistic | |||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | F(2, 90) | p | |
| Age | 19.22 | 1.60 | 18.13 | 0.81 | 19.26 | 1.83 | 4.36 | .016 |
| IQ | 102.19 | 14.93 | 106.59 | 15.96 | 103.02 | 11.57 | 0.72 | .488 |
| N | % | N | % | N | % | χ2 | p | |
| % Male | 26 | 96.3 | 22 | 95.7 | 42 | 97.7 | 0.22 | .894 |
| Medication (%) | .71 | .400 | ||||||
| Previous or current medication | 20 | 74.1 | 20 | 86.9 | - | - | ||
| No medication | 7 | 25.9 | 3 | 13.1 | - | - | ||
| Parental employment (%) | 5.05 | .282 | ||||||
| Skilled job | 13 | 50 | 7 | 30.4 | 17 | 44.7 | ||
| Unskilled job | 8 | 30.8 | 9 | 39.2 | 17 | 44.7 | ||
| Unemployed | 5 | 19.2 | 7 | 30.4 | 4 | 10.6 | ||
Note. ADHD-SU=ADHD with substance use; ADHD-N/SU=ADHD without substance use; no ADHD=Without ADHD; IQ=Intelectual quocient.
The two groups, with ADHD and no ADHD, were matched for age, t (91)=- 1.56, p=.121 and sex, χ2 (1, N=93)=.208, p=.649, with 96.8% being males. The difference between the two groups in estimated IQ, using the vocabulary and block design tests from the Wechsler Adult Intelligence Scale (WAIS III; Wechsler, 1999), was not significant, t (91)=.42, p=.679.
Parents and participants reported drinking alcohol or consumption of tobacco, marijuana and other illegal drugs (e.g., cocaine, ecstasy, opiates, etc.) in the previous twelve months. This information was adopted as the criterion for splitting ADHD participants into two groups: a group with substance use (ADHD-SU) and a group without substance use or with low risk of substance use (ADHD-N/SU). We classified a participant in the former group when either he or his parents reported: 1) frequent consumption (2 drinks per day) or very frequent alcohol consumption (more than 2 drinks per day or more than 4 during the week); 2) any amount of smoking daily; 3) marijuana at least once a week; or 4) occasional use (at least once a month) of other illegal drugs, such as cocaine, heroin and opiates. A subject was classified in the latter group if both he and his parents reported that there was no SU or only very occasional consumption of alcohol or tobacco (e.g., at parties or other special occasions).
By dividing the ADHD group into two groups, one with SU and one without it, statistically significant differences in age were found (F(2,90)=4.36, p=.016); therefore, age was introduced in the analysis as a covariate.
MeasuresPresence and severity of ADHD symptomsThe presence and severity of ADHD symptoms was evaluated with the long version of the Conners Adult ADHD Rating Scale-Observer version (CAARS; Conners, Erhardt, & Sparrow, 1999), which consists of 66 items divided into nine subscales. It includes the 18 ADHD symptoms from the DSM-IV, measured on a 4-point Likert-type scale and grouped in two subscales: DSM-IV-Inattention and DSM-IV-Hyperactivity/ impulsivity. The T-scores of these two subscales were used as dependent variables in this study. T-scores greater than or equal to 65 were considered clinically significant. DSM-IV-Inattention subscale difficulties include trouble concentrating, difficulty planning or completing tasks, forgetfulness, absent-mindedness, and being disorganized. The hyperactivity/impulsivity subscale includes items related to problems with working on the same task for long periods of time, feeling more restless than others seem to be, and fidgeting. This instrument has satisfactory reliability and validity. Internal reliability of the factor scales ranged from .86 to .92; test-retest reliabilities ranged from .88 to .91 (Erhardt, Epstein, Conners, Parker, & Sitarenios, 1999).
Presence and severity of comorbidity symptomsQuestionnaire on Comorbidity-Weiss Symptom Record (WSR; Weiss, 2010). This clinical screening questionnaire is not psychometrically validated but is based on the DSM-IV-TR criteria (APA, 2000). Although it is not a diagnostic scale, it serves the useful purpose to identify adult mental disorders by collecting information about Axis I and Axis II mental disorders in any age group and from any informant. In this research was use the subscales used were Opositional Defiant Disorder (ODD), Conduct Disorder (CD), Anxiety, Depression, Sleep Disorder, and Antisocial Personality Disorder. The items have different response options; “0-Not at all”, “1-somewhat”, “2-pretty much” and “3-very much” (usually interpreted as “this is a problem that causes great difficulty”). A sum of the score on each item of the disorders mentioned above was used as dependent variable in the analysis dichotomized as “absence”(0, 1) or “presence” (2, 3). To evaluate clinical information about the pattern of SU, both the parents and young adults filled out the WSR subscale for Substance Use Disorder. This subscale is composed of 5 items about the consumption of alcohol, tobacco, marijuana and other street drugs, as well as the abuse of prescription drugs. In the current study, we did not use “abuse of prescription drugs” because none of the participants used these drugs.
ProcedureIn the current study, the Weiss comorbidity questionnaire to evaluate the clinical information on manifestations of psychopathologies was filled out by adults with ADHD and adults without ADHD. In addition, parents or a family member of the ADHD group participants completed the CAARS Scale adult ADHD-observer version to assess the presence and severity of symptoms of inattention and hyperactivity / impulsivity. The assessment was performed by ADHD experts trained in the administration and rating of the interviews and questionnaires used. Evaluators strictly followed the same method to apply and correct assessment test. All the participants gave their written consent after being informed of the study goals and funding. They were given 30 Euros for their participation.
Statistical analysesAnalyses were conducted using IBM SPSS Statistics, version 21.0 (SPSS Inc., Chicago, IL, USA). Chi-square (χ2) analyses were conducted to test group differences in SU between adults with and without ADHD. A multivariate analysis of covariance (MANCOVA) was used to study differences in the comorbid problems of ADHD adults with and without SU. For this purpose, ADHD substance use status (ADHD-SU, ADHD-N/SU) was used as the fixed factor, and symptoms of comorbid problems (ODD, CD, anxiety, depression, sleep disorder, and antisocial personality disorder) were used as dependent variables. Age was included in the model as a covariate. Given the significant main effect in the MANCOVA model, individual tests of between-subject effects were examined to identify which comorbid problems significantly differed by group. The level of significance was set at .008, after using Bonferroni correction for multiple comparisons. Effect sizes were calculated using partial Eta squared values (according to Cohen (1988): eta squared, .06=small; .06-.14=medium, .14=large effect size). In addition, some ODD and CD symptoms were categorized as “presence/absence”. Chi-square analyses were conducted to test for differences between ADHD adults with and without SU in the proportion of participants classified as “presence” for each comorbid symptom. Finally, to investigate which symptoms (ADHD or conduct problems) best predicted substance use (alcohol, tobacco, marijuana, other illegal drugs), binomial logistic regression analysis was performed. The data were entered into the logistic regression model in three blocks: Block 1 - age; Block 2 – ODD and CD symptoms (continuous variables); and Block 3: ADHD inattention and hyperactivity/impulsivity symptoms (continuous variables). The ORs, 95% confidence intervals and the R2 value (Nagelkerke-adjusted value) for the overall models are reported.
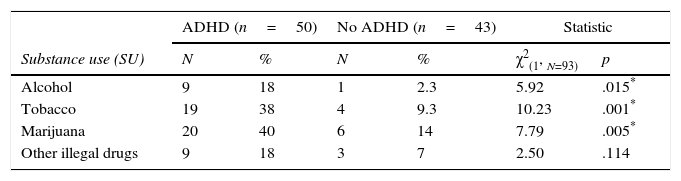
ResultsSubstance use in adults with and without ADHDThe first aim of this study was to compare the SU of young adults with and without ADHD. Chi-square analysis showed statistically significant differences between the groups in the use of alcohol [χ2 (1, N=93)=5.91, p=.015], tobacco [χ2 (1, N=93)=10.22, p=.001] and marijuana [χ2 (1, N=93)=7.79, p=.005]. In all cases, SU percentages were higher in the ADHD group than in the no ADHD group. Differences in other illegal drugs, like cocaine or opiates, did not reach statistical significance [χ2 (1, N=93)=.250, p=.114] (see Table 2).
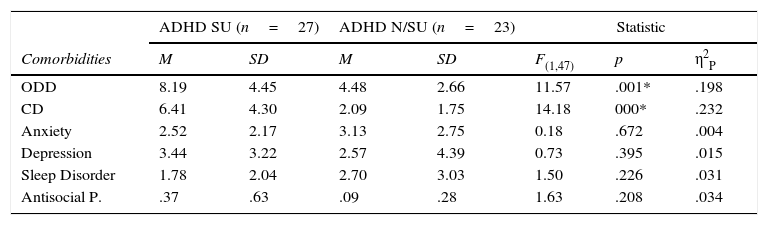
Comparison of comorbidities between ADHD groups with and without substance useTable 3 shows that 54% (n=27) of ADHD adults consumed some kind of substance (ADHD-SU group) versus 46% (n=23) who did not (ADHD-N/SU group). Comorbid problem symptomatology in the two ADHD groups (with and without SU) was compared. MANCOVA results revealed statistically significant differences [Wilks’ Lambda (Λ)=.69, F (6, 42)=3.07, p=.014, η2p=.305]. ANCOVA results indicated statistically significant differences for ODD and CD. In both cases, the ADHD-SU group presented significantly higher comorbidity scores than the ADHD- N/SU group. However, ADHD-SU and ADHD- N/SU did not differ significantly on anxiety, depression, sleep disorder, or antisocial personality disorder (see Table 3).
Differences in comorbid problems between ADHD adults with and without substance use.
| ADHD SU (n=27) | ADHD N/SU (n=23) | Statistic | |||||
|---|---|---|---|---|---|---|---|
| Comorbidities | M | SD | M | SD | F(1,47) | p | η2P |
| ODD | 8.19 | 4.45 | 4.48 | 2.66 | 11.57 | .001* | .198 |
| CD | 6.41 | 4.30 | 2.09 | 1.75 | 14.18 | 000* | .232 |
| Anxiety | 2.52 | 2.17 | 3.13 | 2.75 | 0.18 | .672 | .004 |
| Depression | 3.44 | 3.22 | 2.57 | 4.39 | 0.73 | .395 | .015 |
| Sleep Disorder | 1.78 | 2.04 | 2.70 | 3.03 | 1.50 | .226 | .031 |
| Antisocial P. | .37 | .63 | .09 | .28 | 1.63 | .208 | .034 |
Note. ADHD-SU=ADHD with substance use; ADHD-N/SU=ADHD without substance use ODD=Oppositional defiant disorder; CD=Conduct disorder; Antisocial P.=Antisocial personality disorder. *p<.008 (Bonferroni correction of critical p values when performing multiple comparisons).
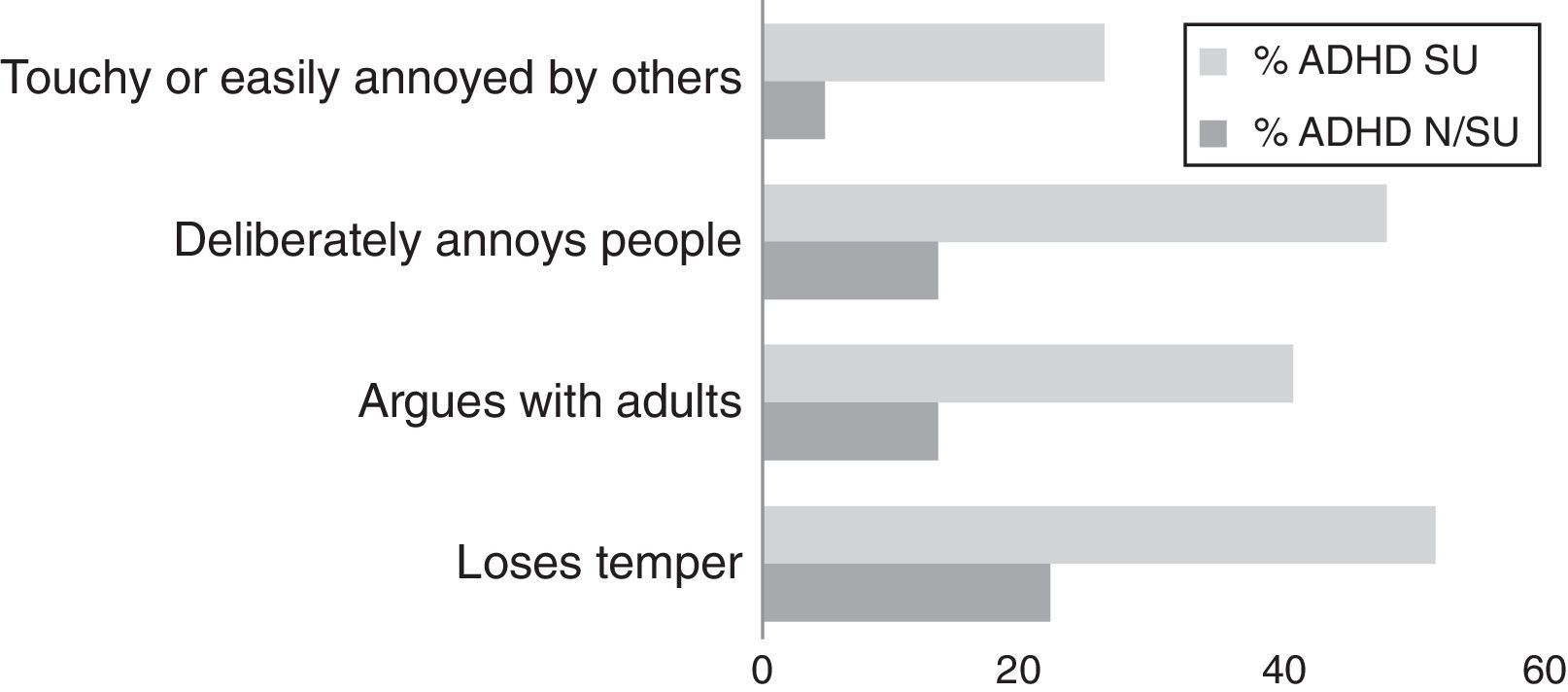
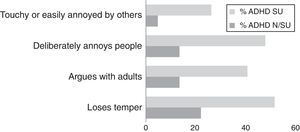
Next, an analysis was performed of possible differences in ODD and CD manifestations in the two groups of subjects with ADHD. Specifically, there were statistically significant differences between ADHD adults with and without SU on some specific ODD symptoms, such as “Touchy or easily annoyed by others” [χ2 (1, N=50)=4.30, p=.030]; “Deliberately annoys people” [χ2 (1, N=50)=7.03, p=.008]; “Argues with adults” [χ2 (1, N=50)=4.72, p=.030] and “Loses temper” [χ2 (1, N=50)=4.78, p=.029]. There were no significant differences in the other ODD manifestations (see Figure 1).
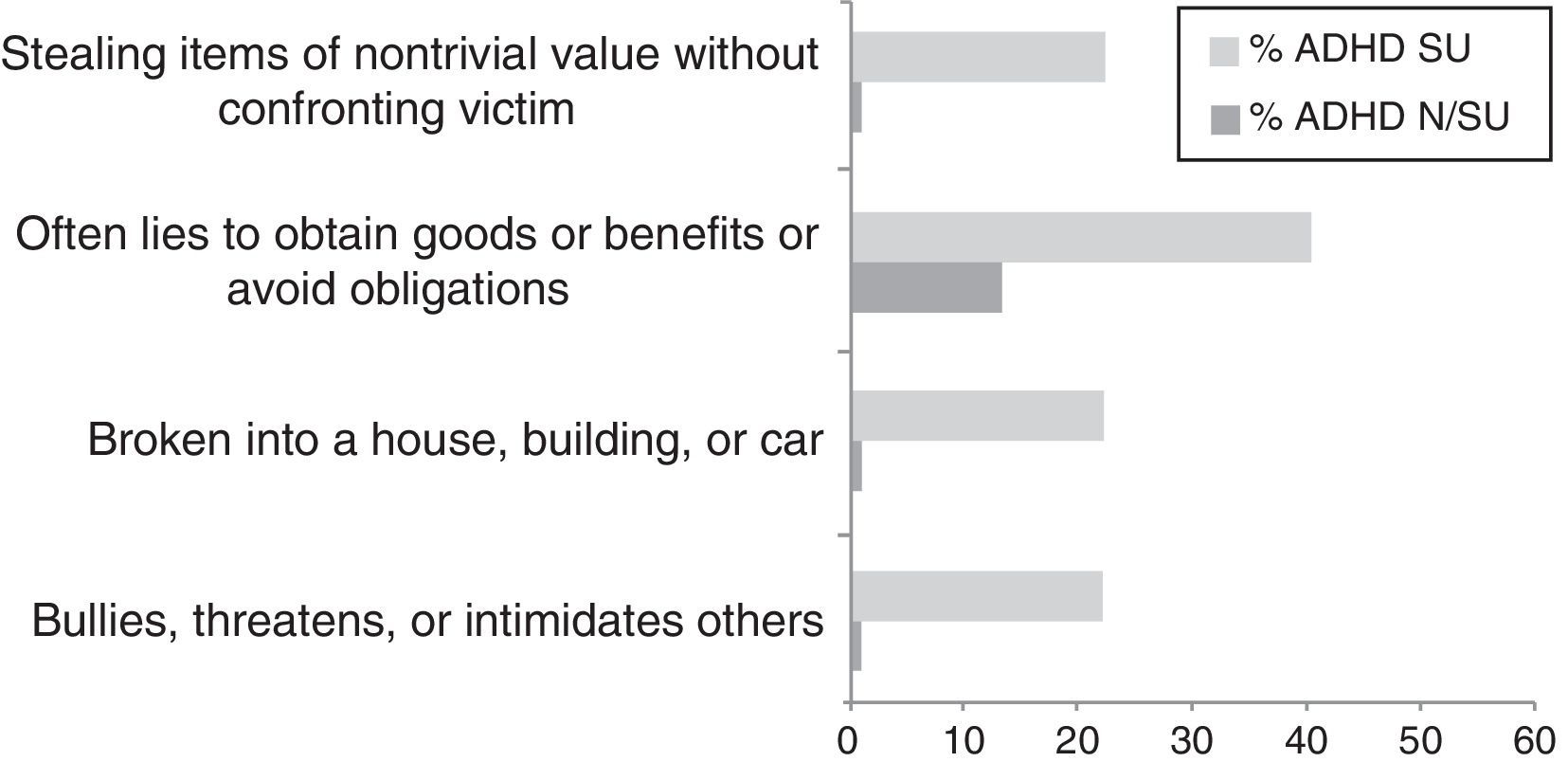
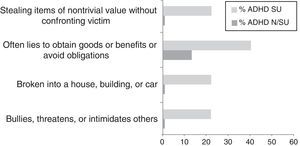
There were also differences between the groups in some specific CD symptoms: “Stealing items of nontrivial value without confronting victim” [χ2 (1, N=50)=5.81, p=.016]; “Often lies to obtain goods or benefits or avoid obligations” [χ2 (1, N=50)=4.71, p=.030]; “Broken into a house, building, or car” [χ2 (1, N=50)=3.78, p=.05]; “Bullies, threatens, or intimidates others” [χ2 (1, N=50)=3.79, p=.05] (See Figure 2).
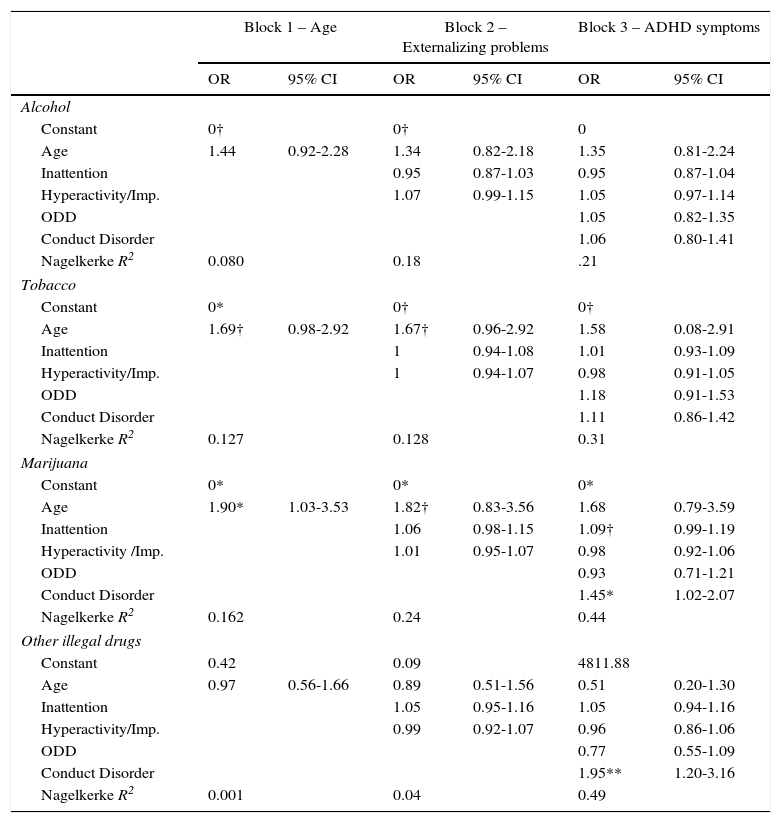
Relationship between ADHD symptoms, externalizing problems (ODD and CD) and substance useLogistic regression analyses were conducted to examine the relationships among ADHD symptoms, externalizing problems (ODD and CD) and the risk of SU (see Table 4). The final models, where age, ADHD symptoms and externalizing problems were introduced, explained 21.2%, 31.5%, 44.3% and 49.6% of the variances in alcohol, tobacco, marijuana use and illegal drug use, respectively. These analyses revealed that neither ADHD symptoms nor conduct problems were associated with alcohol or tobacco use. The only variable that significantly distinguished the SU groups was conduct disorder, which was associated with both marijuana use (p=.038; OR=1.45; CI=1.02-2.07) and the use of other illegal drugs (p=.007; OR=1.95; CI=1.20-3.16). ADHD symptoms did not contribute significantly to any of the four final models; although inattention had a nearly significant association with marijuana use (p=.056; OR=1.09; CI=0.99-1.19).
Logistic regression analyses of predictors of use of tobacco, alcohol, marijuana and other illicit drugs.
| Block 1 – Age | Block 2 – Externalizing problems | Block 3 – ADHD symptoms | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Alcohol | ||||||
| Constant | 0† | 0† | 0 | |||
| Age | 1.44 | 0.92-2.28 | 1.34 | 0.82-2.18 | 1.35 | 0.81-2.24 |
| Inattention | 0.95 | 0.87-1.03 | 0.95 | 0.87-1.04 | ||
| Hyperactivity/Imp. | 1.07 | 0.99-1.15 | 1.05 | 0.97-1.14 | ||
| ODD | 1.05 | 0.82-1.35 | ||||
| Conduct Disorder | 1.06 | 0.80-1.41 | ||||
| Nagelkerke R2 | 0.080 | 0.18 | .21 | |||
| Tobacco | ||||||
| Constant | 0* | 0† | 0† | |||
| Age | 1.69† | 0.98-2.92 | 1.67† | 0.96-2.92 | 1.58 | 0.08-2.91 |
| Inattention | 1 | 0.94-1.08 | 1.01 | 0.93-1.09 | ||
| Hyperactivity/Imp. | 1 | 0.94-1.07 | 0.98 | 0.91-1.05 | ||
| ODD | 1.18 | 0.91-1.53 | ||||
| Conduct Disorder | 1.11 | 0.86-1.42 | ||||
| Nagelkerke R2 | 0.127 | 0.128 | 0.31 | |||
| Marijuana | ||||||
| Constant | 0* | 0* | 0* | |||
| Age | 1.90* | 1.03-3.53 | 1.82† | 0.83-3.56 | 1.68 | 0.79-3.59 |
| Inattention | 1.06 | 0.98-1.15 | 1.09† | 0.99-1.19 | ||
| Hyperactivity /Imp. | 1.01 | 0.95-1.07 | 0.98 | 0.92-1.06 | ||
| ODD | 0.93 | 0.71-1.21 | ||||
| Conduct Disorder | 1.45* | 1.02-2.07 | ||||
| Nagelkerke R2 | 0.162 | 0.24 | 0.44 | |||
| Other illegal drugs | ||||||
| Constant | 0.42 | 0.09 | 4811.88 | |||
| Age | 0.97 | 0.56-1.66 | 0.89 | 0.51-1.56 | 0.51 | 0.20-1.30 |
| Inattention | 1.05 | 0.95-1.16 | 1.05 | 0.94-1.16 | ||
| Hyperactivity/Imp. | 0.99 | 0.92-1.07 | 0.96 | 0.86-1.06 | ||
| ODD | 0.77 | 0.55-1.09 | ||||
| Conduct Disorder | 1.95** | 1.20-3.16 | ||||
| Nagelkerke R2 | 0.001 | 0.04 | 0.49 | |||
Note. ODD=Oppositional defiant disorder; CI=confidence interval; OR=odds ratio. † < .10; * p<.05; ** p<.010.
The first objective of the current study was to confirm that children with ADHD combined-type have an increased risk of SU in young adulthood. Coinciding with a large body of literature, we found a significantly higher prevalence of SU in the group with ADHD compared to the group without ADHD (Breyer et al., 2014; van Emmerik-van Oortmerssen et al., 2012), according to our prediction: alcohol, tobacco and marijuana. Only the rates of use of illicit drugs other than marijuana were not significantly different from the control group although they were high.
In fact, with regard to illegal drugs, the 40% of the participants with ADHD had used marijuana, versus 14% of the group without ADHD, which matches the percentage provided by the OEDT (14% for young people between 15 and 24 years old). Various mechanisms could be operating in the overrepresentation of SU identified in this sample, such as a common genetic predisposition between ADHD and SU. Particularly regarding dependence on alcohol (Edwards & Kendler, 2012) some data suggest that shared genetic risk factors explain 64% of the overlap between ADHD and alcohol (Capusan et al., 2015). Self-medication of ADHD symptoms and personality factors, such as impulsivity, anger or high levels of sensation seeking, are other possible explanations proposed for the propensity of SU in people with ADHD (Arias et al., 2008; Ballon, Brunault, & Cortese, 2015). There are also diverse psychosocial factors, including academic failure, social problems or a permissive and tolerant parenting style (Cerezo, Méndez, & Ato, 2013; Cortese et al., 2015; Molina & Pelham, 2014).
According to the results, our second prediction was partially confirmed. ADHD-SU and ADHD- N/SU groups did not differ significantly on anxiety, depression or sleep disorder symptoms (Wilens et al., 2011). However, supporting our hypothesis, the ADHD-SU group presented significantly higher comorbidity scores than the ADHD- N/SU group on externalizing disorders. As in other studies (Brinkman et al., 2015; Nogueira et al., 2014; Symmes et al., 2015), the manifestations of ODD and CD in individuals with childhood ADHD and SU were clearly more prevalent than in the ADHD group that did not consume. More specifically, there were statistically significant differences in ODD symptoms of irritability, such as “Touchy or easily annoyed by others” and “Loses temper”, or headstrong behaviors, such as “Deliberately annoys people” and “Argues with adults”. There were also differences between the groups in some specific CD symptoms related to deceitfulness or theft, such as “Stealing items of nontrivial value without confronting the victim” and “Often lies to obtain goods or benefits or avoid obligations”, in non-aggressive manifestations of CD, “Broken into a house, building, or car”, and on an item related to aggression toward people, “Bullies, threatens, or intimidates others”.
Finally, concerning our third prediction, neither ADHD symptoms severity nor externalizing problems were associated with alcohol or tobacco use in the ADHD adults. However, the manifestations of conduct disorder significantly predicted both the use of marihuana and the use of other illegal drugs. Of the ADHD symptoms, only inattention had a nearly significant association with marijuana use. These results suggest that CD symptoms, rather than ADHD symptoms, are the strongest predictor of substance use, especially more severe drugs like marijuana and cocaine, according with several studies (Rodgers et al., 2015; Serra-Pinheiro et al., 2013).
Limitations and futures directionsThe results from this study should be considered in the context of several unique study features and limitations. The group of young adults with ADHD was relatively small and had clinical remission. Therefore, it would be interesting to replicate the study with a larger sample. In addition, all of the participants in the sample with ADHD were diagnosed with the combined type from the DSM-IV, so generalization of the results should generally not extend beyond this subtype. Especially because both ADHD subtypes differs significantly in attention and in state and trait anxiety (González-Castro, Rodriguez, Cueli, García, & Alvarez-García, 2015). Moreover, comorbid problems were reported using a screening measure. These results should be replicated using instruments to establish a clinical/psychiatric diagnostic. In this study, the moderating role of socio-environmental risk variables was not examined either, such as parents’ educating styles or friends’ attitudes towards consumption and easy access to drugs, among others.
Overall, the relevance of our findings consists of their contribution to underscoring that young adults with an ADHD diagnosis have an increased risk of SU, specifically tobacco and marijuana, and therefore require preventive and early intervention efforts. Comorbid ADHD and SU produce significant and unique treatment challenges, including less likelihood of successful treatment completion, a longer time to SU recovery, and earlier SU relapse. Unfortunately, ADHD medication does not protect the individual from the risk of SU (Molina et al., 2013), and its efficacy in the treatment of co-occurring ADHD and SU is only modest (Cunill, Castells, Tobias, & Capellà, 2015), which suggests the need to identify alternative or adjunct approaches to substance abuse prevention and ADHD treatment.
Psychotherapeutic intervention in addition to pharmacological treatment can be beneficial. Cognitive behavioral therapy may be of particular interest, and neurofeeedback (given preliminary evidence suggesting its possible efficacy in adolescents with comorbid ADHD and SU (Thurstone, Riggs, Salomonsen-Sautel, & MikulichGilbertson, 2010).
We thank Dr. Faraone for inviting us to collaborate in the IMAGE project, and all the families who kindly participated in this research