Researchers have found growing evidence for the comorbidity link between bulimia and emotional symptoms among Chinese female youth. However, the prospective effect of one on the other is still unclear. Therefore, a cross-lagged model was used to examine the possible underlying mechanism between bulimia and two typical emotional problems (i.e., anxiety symptoms and depressive symptoms), respectively, in the present study.
MethodsA total of 471 female college students participated in the three waves of the present study. Self-reported questionnaires were delivered to assess their bulimia, anxiety symptoms, and depressive symptoms.
ResultsAfter controlling for earlier levels of symptoms, our finding indicated that anxiety symptoms triggered more bulimia symptoms from Time 1 to Time 2. In turn, the reciprocal cycles occurred between anxiety symptoms and bulimia symptoms from Time 2 to Time 3. More interestingly, a similar pattern was found between depressive symptoms and bulimia.
ConclusionsThe persistence and reciprocal cycle between bulimia and emotional symptoms are worthy of attention. Specifically, female youth with higher levels of emotional symptoms appear to be more profound at high risk for eating-related problems afterward. Further eating-related intervention programs may also need to take the level of female youth's emotional symptoms into consideration.
Bulimia nervosa is an eating disorder characterized by a cycle of binge eating and compensatory behaviors to the over-concern with body shape and weight gain (Li et al., 2021). As one of the alarming health issues among female youth (Campbell & Peebles, 2014; Elran-Barak & Goldschmidt, 2021), bulimia has been significantly associated with a series of impairments in an individual's psychological and social functions, such as heart disorders, interpersonal problems, and even suicidal behaviors (Puttevils et al., 2021). Thus, exploring the underlying mechanism for the persistence and maintenance of bulimia among female youth is timely and important.
Substantial research has addressed which factors are implicated in the maintenance and deterioration of bulimia. Among all the factors, the evidence for the co-occurrence between bulimia and emotional symptoms is quite strong (Bulik et al., 2006; Godart et al., 2007; Li et al., 2021; Polanczyk et al., 2015). For example, a meta-analysis found that the prevalence of depression among individuals with an eating disorder was 57% (Khraisat et al., 2022). In addition, over 50% of adolescents with eating disorders have also reported a lifetime anxiety symptoms disorder. The co-occurring symptoms may hamper the recovery efforts. For example, the persisting emotional symptoms after the single treatment for bulimia symptoms would increase the risk of relapse, as individuals with high emotional distress may still revert to former eating behaviors (Sander et al., 2021). Thus, the association between bulimia and emotional symptoms warrant our attention.
Previous studies have indicated the intricate relationships between bulimia and emotional symptoms. On the one hand, several studies suggested that emotional symptoms may initiate later eating problems. The framework of eating disorders suggests that individuals may use disordered eating behaviors as one of the most maladaptive strategies to regulate and avoid undesired feelings (Mallorquí-Bagué et al., 2018). For instance, individuals with higher levels of anxiety symptoms and depressive symptoms were found to use disordered eating as a dysfunctional regulation strategy to cope with their emotion (Sander et al., 2021). Similarly, broaden-and-build theory explains that negative emotions can narrow an individual's cognitive and behavioral systems and restrict their ability to perceive ability psychological resources (Johnson et al., 2021), especially for the youth. Thus, an individual with anxiety symptoms or depressive symptoms may demonstrate greater sensitivity to negative experiences and ruminate unpleasant events (Catalino et al., 2017). Moreover, the individual is unable to construct sustainable development resources, which would lead to more maladaptive behaviors, such as bulimia. On the other hand, eating problems may also trigger later emotional symptoms. Specifically, female youth with bulimia may have a more negative perception about themselves as well as their appearance, and they may feel guilty and shame, thus increasing the risk of the persistence and maintenance of later depressive symptoms (Ivarsson et al., 2006; Jones & Griffiths, 2015). Another explanation is that caloric deprivation during the compensatory behaviors would lead to a corticotropin-releasing hormone, which triggers negative emotional symptoms (O'Brien & Vincent, 2003). In line with this explanation, Stice et al. (2000, 2004) found that eating disturbance, including bulimia, predicted later depression among female adolescents. Marmorstein et al. (2008) also found that eating problems can solely predict later depressive symptoms among adolescent girls in the United States by using the cross-lagged model.
The link between bulimia and emotional symptoms among female adolescents have a bidirectional effect. However, a substantial amount of previous research has only focused on a single direction of the relationship between eating problems or emotional symptoms. For example, the prospective reciprocal effects were found between eating disorders and depressive symptoms moods among French youth by using the cross-lagged model (Boujut & Gana, 2014). In line with this finding, Presnell and colleagues determined that an individual's depressive symptoms would predict later eating problems; moreover, these eating problems likewise predicted later depressive symptoms (Presnell et al., 2009). These mixed findings between eating problems and emotional symptoms warrant our attention, especially as limited studies have hinted on the possible directional effect between bulimia and different types of emotional symptoms, including depression and anxiety symptoms. In addition, previous studies have been largely based on youth samples from the US (Mojtabai et al., 2016), the UK (Patalay & Gage, 2019), and Finland (Filatova et al., 2019). However, few studies have been explored among the Chinese youth, where people take more externalizing behaviors to tolerate their feelings (Wu et al., 2021). A national study reported an increasing persistence rate of bulimia among the Chinese youth compared with the decreasing rate in Western countries (Wu et al., 2020). Hence, this research gap must be filled by using the Chinese female youth, as understanding the possible mechanisms of both can help make better interventions.
To summarize, theoretical and empirical evidence has shown that emotional symptoms can promote an individual's later bulimia symptoms. Some evidence has also indicated that bulimia triggers the subsequent emotional symptoms. Moreover, a number of studies have pointed out the reciprocal effects of this condition. The mixed findings may be due to previous studies mainly adopting cross-sectional data or a short-term longitudinal design (Elran-Barak & Goldschmidt, 2021; Levinson et al., 2017; Şahan et al., 2021), as well as the diverse cultural and social backgrounds across studies. To disentangle the possible prospective relationships between bulimia and emotional symptoms among the Chinese youth, the present study uses three years’ worth of longitudinal tracking design to explore the following three research questions:
Q1: What is the prospective relationship between bulimia and depressive symptoms?
Q2: What is the prospective relationship between bulimia and anxiety symptoms symptoms?
Q3: Do certain similarities exist between these two relationships?
Participants in the study were recruited from a medical college located in Heze, China using a convenience sampling method. In total, 471 female students participated in all three collections over three years and completed the full scales of the Eating Disorder Inventory (EDI) and SCL-90 measures to assess bulimia nervosa, anxiety symptoms, and depressive symptoms. These students were included in the current analyses. The mean age of students was 18.60 years old (SD = 0.84, range = 16-24), and the average body mass index (BMI) was 20.27 (SD = 3.17); also, 79% of these students had at least one sibling.
Students completed a paper-and-pencil questionnaire. Before the test, school teachers and psychologists introduced the study purpose and provided prompt instructions to the participants. No compensation was provided. Written informed consent was obtained from all participants, and ethics approval was granted.
MeasurementCovarianceStudents’ demographic information was measured by a questionnaire, including their age, with siblings or not (0 = only child, 1 = with siblings), and body mass index (BMI = kg/m2, calculated by dividing the weight by the height squared). In the present study, only BMI and age were correlated with our key study variables (p <.05). Thus, they were included as a covariate in analyses.
BulimiaEDI is a standardized self-reported questionnaire that taps into various eating disorder symptoms, including drive for thinness, body dissatisfaction, ineffectiveness, perfection, interpersonal distrust, interoceptive awareness, maturity fears, and bulimia. In the current study, we used the bulimia subscale to assess the individual's bulimia symptoms (Garner, 2004; Garner et al., 1983). Examples included “I eat or drink in secrecy.” Items were rated on a six-point Likert scale ranging from 1 (never) to 6 (always). The seven items were summed to create a total score, and a higher total score indicated a higher risk of bulimia symptoms. In the present study, the subscale showed good internal consistency coefficients: α >.74 at both T1, T2, and T3; McDonald's omega was more than 0.74 at each of the three waves.
DepressionSCL-90 is a multidimensional questionnaire developed, and the subscale scores are used as indicators for specific emotional symptoms and psychopathological features, including, somatization, obsessive compulsion, interpersonal sensitivity, depression, anxiety symptoms, hostility, phobic anxiety symptoms, paranoid ideation, and psychoticism (Derogatis & Savitz, 1999; Wang, 1984). In the present study, the depression subscale in SCL-90 was used to assess an individual's depression during the past four weeks. Example items included “feeling blue,” “feeling low in energy or slowed down,” and “feeling everything is an effort.” Students were asked to rate each item on a five-point Likert scale ranging from 0 (not at all) to 4 (extremely). A higher total score on this subscale indicated a higher level of depression. Cronbach's alphas were more than 0.89 at each of the three waves. Furthermore, McDonald's omega were 0.90 over three waves in the present study.
Anxiety symptomsThe anxiety symptoms subscale in SCL-90 was used to assess an individual's anxiety symptoms during the past four weeks (Derogatis & Savitz, 1999). Example items included “spells of terror or panic,” “feeling so restless you cannot sit still,” and “trembling.” Items were rated on a five-point Likert scale ranging from 0 (not at all) to 4 (extremely). In this study, the subscale showed good internal consistency values: α >0.85 at both T1, T2, and at T3; and McDonald's omega ranged from 0.85 to 0.86 across three waves.
Statistical analysisThe descriptive and correlation analyses were performed using IBM SPSS. Next, measurement invariance testing was conducted to examine whether the constructs of bulimia nervosa, anxiety symptoms, and depression remained invariant over three years (van de Schoot et al., 2012). To test our main hypothesis, we used the cross-lagged panel model, which is based upon structural equation modeling, to test the relationship between bulimia and anxiety symptoms or depressive symptoms over three periods. Models were run with AMOS V.23 using full information maximum likelihood estimation. The model fit was evaluated using several fit indexes: 1) the chi-square (χ2) test of model fit, 2) the root mean square error of approximation (RMSEA), 3) the comparative fit index (CFI), 4) the Tucker-Lewis index (TLI), and 5) the standardized root mean square residual (SRMR). A non-significant χ2, normed chi-square (χ2/df) < 5, RMSEA with values less than 0.08, CFI and TLI values equal to or greater than 0.9, and SRMR values below 0.08 indicated a good model fit (Kline, 2011). Given the multiple pathways, the Benjamini and Hochberg (1995) used false discovery rate correction to correct the p-values and maintain the Type I error rate below 0.05.
ResultsPreliminary analysisThere were no significant difference in socio-demographic characteristics of those who were followed up (n = 471) and those who were missing in the first and second wave surveys (n = 1032), including ages, t = 0.57, p = .57, and whether they had siblings or not χ2 = 1.6, p = .46. Results of the descriptive and correlation were presented in Table 1, all variables at each time point had a positively significant correlation (p <.001).
Pearson correlations between bulimia, anxiety and depression at T1, T2 and T3 (N = 471).
| Variables | Mean (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Bulimia T1 | 12.32 (4.97) | - | - | - | - | - | - | - | - |
| 2. Bulimia T2 | 11.60 (4.33) | .49*** | - | - | - | - | - | - | - |
| 3. Bulimia T3 | 12.05 (4.61) | .36*** | .50*** | - | - | - | - | - | - |
| 4. Anxiety T1 | 4.47 (4.75) | .27*** | .32*** | .24*** | - | - | - | - | - |
| 5. Anxiety T2 | 4.54 (4.31) | .17*** | .40*** | .30*** | .57*** | - | - | - | - |
| 6. Anxiety T3 | 4.42 (4.39) | .22*** | .34*** | .39*** | .49*** | .58*** | - | - | - |
| 7. Depression T1 | 5.84 (6.32) | .22*** | .25*** | .18*** | .82*** | .52*** | .45*** | - | - |
| Depression T2 | 6.05 (5.95) | .16*** | .37*** | .28*** | .49*** | .85*** | .53*** | .53*** | - |
| Depression T3 | 6.30 (6.05) | .20*** | .34*** | .39*** | .47*** | .59*** | .85*** | .49*** | .62*** |
Note: Anxiety = Anxiety, Depression = Depression. T1= Time 1; T2 = Time 2; T3 = Time 3.
The Harman's single factor analysis was used to test common method variance effect. The total variance by one factor was less than or equal to the recommended threshold of 50% (Chang et al., 2010), which indicating that the common method biases was not an issue for this study.
Measurement invarianceMeasurement invariance between bulimia and anxiety symptoms, as well as, depression at three-time points were examined. In line with previous studies, change of CFI (△CFI)(Chen, 2007) was a stable indicator for model comparison due to the less influenced by sample sizes and model parameters. For instance, if △CFI ≤ .01 the models would be determined to be invariant. In this study, model comparison suggested that both bulimia and anxiety symptoms, as well as depression showed measurement invariance across three-time points (△CFI ≤ .01, see Table 2), thus a cross-lagged model could be carried out in the next step.
Model fitting results of measurement invariance for study variables.
Note: M0, configural invariance model; M1, factor loading invariance model; M2, residual invariance model.
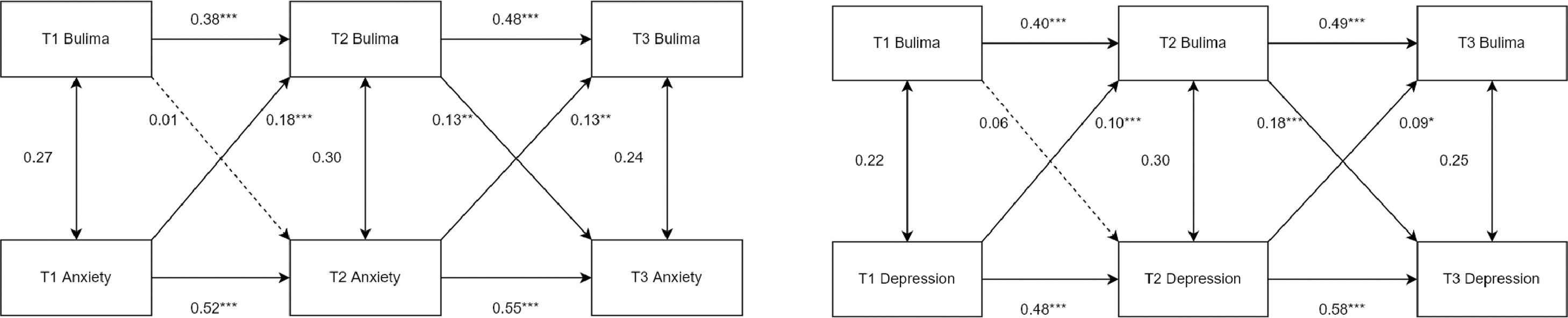
The model with acceptable fit, χ2/df = 3.99, p < .001, CFI = 0.95, TLI =0.90, RMSEA =0.08, SRMR =0.04 (see Figure 1). After controlling for age and BMI, the autoregressive path coefficients of bulimia were 0.38 and 0.48, respectively; and the autoregressive path coefficients of anxiety symptoms were 0.52 and 0.54 respectively. The results indicated a relatively strong autoregressive effect for both bulimia and anxiety symptoms over 3 years. As for the cross-lagged effect, anxiety symptoms at T1 significantly predicted bulimia at T2 (b = 0.18, p <.001, adjusted p = .002), and anxiety symptoms at T2 also significantly predicted bulimia at T3 (b = 0.13, p =.01, adjusted p = .01). Meanwhile, bulimia at T2 significantly predicted anxiety symptoms at T3 (b = 0.13, p =.002, adjusted p = .003). However, the prediction of bulimia at T1 on anxiety symptoms at T3 was not significant (b = 0.01, p = .67, adjusted p = .67).
The cross-lagged panel model of bulimia and anxiety (1a) and the cross-lagged panel model of bulimia and depression (1b). Note. To simplify the model, the predictive pathways of the control variables at three-time points are not shown. Anxiety = anxiety symptoms. Depression = depression. T1 = Time 1, T2 = Time 2, T3 = Time 3. Solid line = significant coefficient; Dotted line = non-significant coefficient. All coefficients were unstandardized. **p <.01, ***p <.001.
The model with acceptable fit, χ2/df = 4.06, p < 0.001, CFI = 0.95, TLI =0.89, RMSEA =0.08, SRMR =0.04 (see Figure 2). After controlling for age and BMI, the autoregressive path coefficients of bulimia were 0.40 and 0.49, respectively; and the autoregressive path coefficients of depression were 0.49 and 0.58 respectively. The results indicated a relatively strong autoregressive effect for both bulimia and depression over 3 years. As for the cross-lagged effect, depression at T1 significantly predicted bulimia at T2 (b = 0.10, p <.001 adjusted p = .001), and depression at T2 also significantly predicted bulimia at T3 (b = 0.09, p =.01, adjusted p = .001). Meanwhile, bulimia at T2 significantly predicted depression at T3 (b = 0.18, p <.001, adjusted p = .001). However, the prediction of bulimia at T1 on depression at T3 was not significant (b = 0.06, p = .22, adjusted p = .22).
DiscussionThe present study used a sample of Chinese female youths to investigate the association between bulimia and anxiety symptoms as well as bulimia and depressive symptoms with three waves of data. Results first suggested that emotional symptoms may trigger dysfunctional regulation, such as bulimia, from T1 to T2; a reciprocity circle between bulimia and emotional symptoms was activated later from T2 to T3. In addition, similar pathways exist for the longitudinal association between bulimia and anxiety symptoms, as well as depressive symptoms.
With regard to the cross-lagged design, anxiety symptoms at T1 predicted an individual's bulimia symptoms at T2. Then. the reciprocal cycles between bulimia and anxiety symptoms were found later. The anxiety symptoms contributing to the later persistence of bulimia was consistent with previous findings (Rosenbaum & White, 2015; Swinbourne & Touyz, 2007). Given that individuals are often encouraged to control and suppress their emotional expression within Chinese culture (Dere et al., 2013; Lim, 2016), the Chinese female youth may engage in bulimic behaviors as a defense mechanism for avoiding more negative feelings when they are faced with stress (Johnson et al., 2002) rather than directly expressing their feelings (Wu et al., 2021). Additionally, we found the reciprocal cycles between bulimia and anxiety symptoms later. One possible explanation is that bulimia may worsen individuals’ immune system and their body appearance, reduce their self-esteem and feel worthless, thus increasing their desire to gain the approval of others and developing a fear of rejection (Mason et al., 2022). These effects further lead to emotional vulnerability (Puttevils et al., 2021), such as increasing anxiety symptoms (Bulik et al., 1996). Meanwhile, anxiety symptoms continues to trigger more maladaptive behaviors as a way to divert attention (Gaspar & McDonald, 2018). In this way, bulimia may later co-occur with anxiety symptoms in a mutually self-enhancing and upholding cycle.
Similar to the underlying mechanism between bulimia and anxiety symptoms, bulimia can be triggered by depressive symptoms, thus leading to reciprocal effects. These findings corroborate with previous research (Bardone-Cone et al., 2010; Fitzsimmons & Bardone-Cone, 2011), including the notion that individuals with depressive symptoms tend to develop more bulimia symptoms (Johnson et al., 2002), which may subsequently increase the risk of social isolation (Godart et al., 2000) and trigger more subsequent depressive symptoms. However, our findings are partially consistent with Marmorstein and colleagues’ findings (Marmorstein et al., 2008), who only found the earlier levels of eating disorder symptoms. Depression among adolescent girls was predicted later using cross-lagged analysis. The discrepancy between the severity and types of eating problems may be among the critical factors in these two studies. For example, the genomic factor varies across anorexia nervosa, bulimia nervosa, and binge-eating disorders (Hübel et al., 2021). Specifically, prior research has demonstrated that anorexia nervosa and bulimia nervosa also report decreased individual's quality of life, and these detriments are related to comorbid psychopathology in bulimia nervosa, such as anxiety symptoms and depression (Ágh et al., 2016; Singleton et al., 2019). Future studies could take a deeper investigation of the shared and unique mechanism between different types of eating problems and emotional symptoms.
The mechanisms and models of the longitudinal effect between bulimia and emotional symptoms (e.g., depressive symptoms and anxiety symptoms) are similar. That is, Chinese female youths with emotional symptoms tend to trigger more maladaptive coping strategies, such as bulimia. In turn, this way of coping may trigger a negative cycle between their negative feelings and maladaptive behaviors. Hence, it may provide an explanation for the high relapse and long resistance of bulimia during the treatment (Berends et al., 2018). Individuals with emotional symptoms tend to be more psychologically unstable and are thereby likely to use a similar maladaptive defense mechanism (e.g., complementary behaviors) against negative feelings, frustration, and uncertainty (Puttevils et al., 2021). Another possible explanation is that anxiety symptoms and depression are also two of the most frequent comorbid mental health disorders among the youth (Garber & Weersing, 2010), which may not be sensitive enough to detect the difference between the two mood disorders. Hence, we particularly used two subscales from SCL-90 in the present study. Our study also relied on variable theory from the traditional disease framework and neglected the possible interaction at symptom levels (e.g., depression: lack of sleep, fatigue, and low energy; anxiety symptoms: restlessness, irritability, and difficulty controlling feelings of worry [Honeycutt et al., 2021]). The bridge symptoms between bulimia and depression may be different than the bridge between bulimia and anxiety symptoms at the symptom level (e.g., the bridge symptoms in network analysis). Therefore, further exploration on the directional effect among bulimia, depression, and anxiety symptoms at the symptom level by using directional network analysis is necessary.
Taken together, our findings have unfolded a more comprehensive picture of the dynamic relationship between bulimia (a specific type of eating problem) and different emotional symptoms in a Chinese female sampling. These findings also contribute to further prevention and intervention practices (Hildebrandt et al., 2012). We first found that the emotional symptoms may first trigger an individual's bulimia symptoms, as a maladaptive behavior, which implies that emotional symptoms may need to be targeted ahead of bulimia symptoms in the future prevention programs and may help alleviate an individual's suffering in the face of comorbid conditions. In line with this finding, a meta-analysis of randomized controlled trails shows that the significant reduction in depressive symptoms through cognitive behavior therapy (CBT) can be associated with greater improvement in bulimia (Linardon et al., 2017). Bäck and colleagues later found that the reduction in depressive symptoms also reduces eating problems through interpersonal psychotherapy (Bäck et al., 2020). These findings also shed light on further clinical practice, in which health workers are encouraged to alleviate their patients’ negative feelings, as these emotional symptoms may hamper the therapeutic alliance, as well as the process with the eating problems and the maintenance of the co-occurring symptoms (Fairburn et al., 2003).
Strengths and limitationsEvidently, a longitudinal study that collects data at three time points and covers a wide range of age groups is one of the strengths of this study. Subscale measures to assess bulimia, anxiety symptoms, and depressive symptoms over three years clearly reveal the directional and negative cycles between bulimia and emotional symptoms. In addition, previous literature has focused on young adults from Western countries, while the association between mood disorders and bulimia in Chinese culture remains unknown. Furthermore, we found similar pathways between bulimia and anxiety symptoms, as well as bulimia and depressive symptoms.
Some limitations are also worth mentioning here. First, the present study involves community samples who have not been clinically diagnosed with bulimia nervosa or mood disorders and have subsequently not undergone medical treatment. The association between bulimia nervosa and mood disorders may be different among the clinical samples. Therefore, caution should be taken when generalizing the findings reported in this study. Second, this study was carried out in a Chinese culture sampling. As the notion of the ideal body varies in different cultures (Warren et al., 2005), our findings may not be transferable to other contexts. Thus, cross-cultural studies are needed to compare bulimia in different cultures, as bulimia is an internal and subjective process. Third, the present study used self-reports and subscales, which might lead to potential measurement bias, which is an issue that should be addressed in future studies (Hu & Cheung, 2021). Lastly, although bulimia is more common in females, men have gradually shown several related problems, as attitudes toward men have shifted in recent years. Gender differences in the relationship between bulimia and mood disorders can be explored in future studies.
ConclusionOverall, the present study offers a full picture of the longitudinal relationship among bulimia, anxiety symptoms, and depressive symptoms. Moreover, the study provides new evidence for the framework of eating disorders and broaden-and-build theory by indicating that emotional symptoms may trigger the later persistence of bulimia and create a negative co-occurring loop between emotional symptoms and bulimia. On the one hand, health practitioners should be aware that female youth with anxiety symptoms or depressive symptoms may engage in bulimic behaviors as a maladaptive emotional coping strategy. Hence, professionals should not only care about the current negative feelings of individuals but also teach them how to cope with stress effectively. On the other hand, these findings contribute ideas to aid in the future prevention and intervention programs of female youth with bulimia symptoms, in which the components of the reduction of emotional symptoms should also be integrated into the traditional treatments for bulimia to minimize the risk of relapse triggered by emotional distress (Bearman et al., 2003).
This research was supported by Award Number 2021M701429 from China Postdoctoral Science Foundation, 2021GJ005 from Guangdong Committee of the Communist Youth League and 22JNZS19 from Guangdong Industrial Development and Guangdong-Hong Kong-Macao-Taiwan Regional Cooperation Research Center.