With the advances in assisted reproduction techniques and above all thanks to the implementation of vitrification, there are more and more surplus pre-embryos in assisted reproduction cycles.
Material and methodsRetrospective observational study.
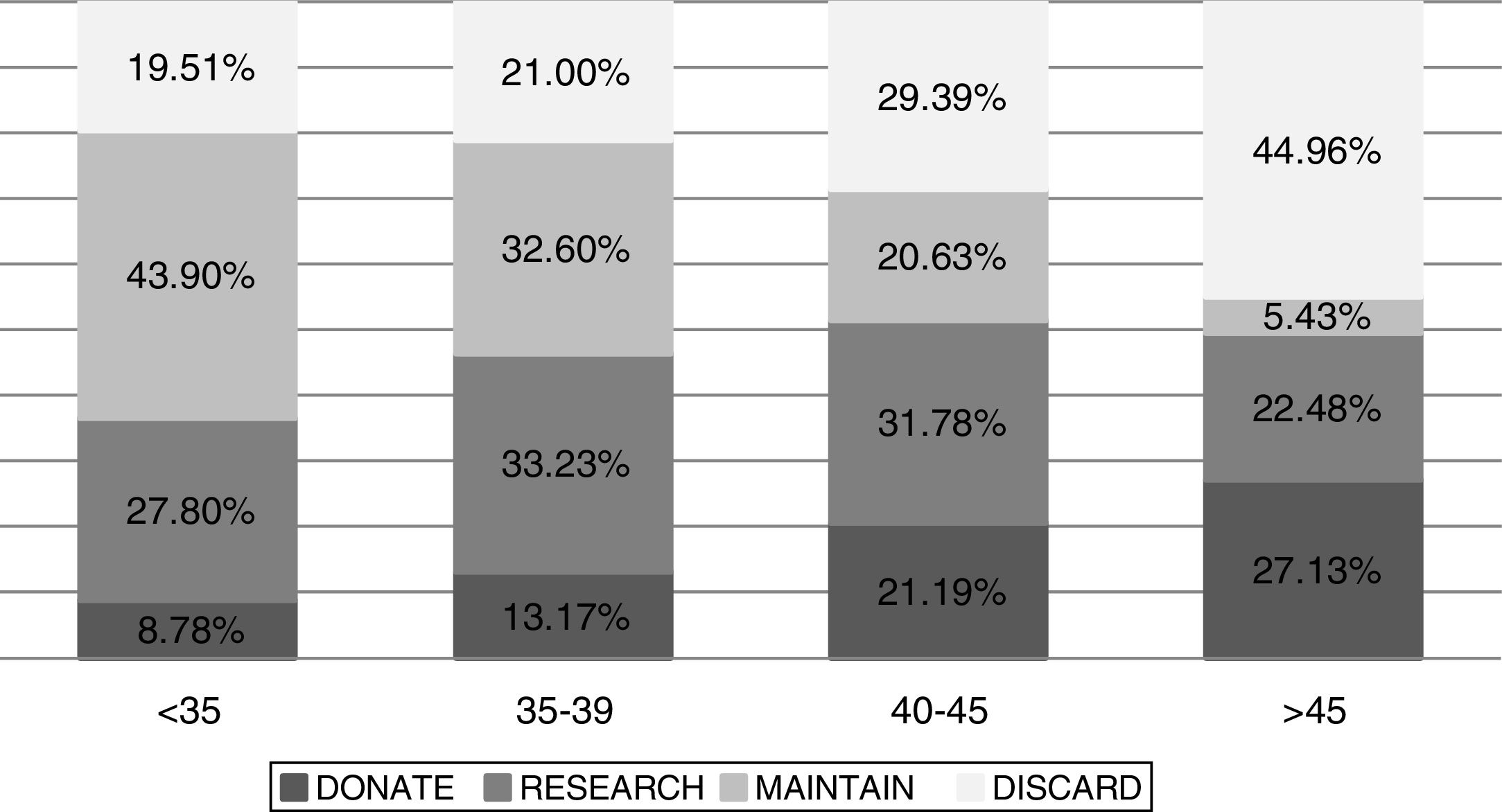
ResultsThe maternal age of patients who decided to donate their pre-embryos to other patients (41.38±4.55) was higher than those who preferred to donate to research (39.56±4.89), keep them for future use (37.38±4.72), or discard them for no other purpose (40.87±5.21) p-value: <0.05.
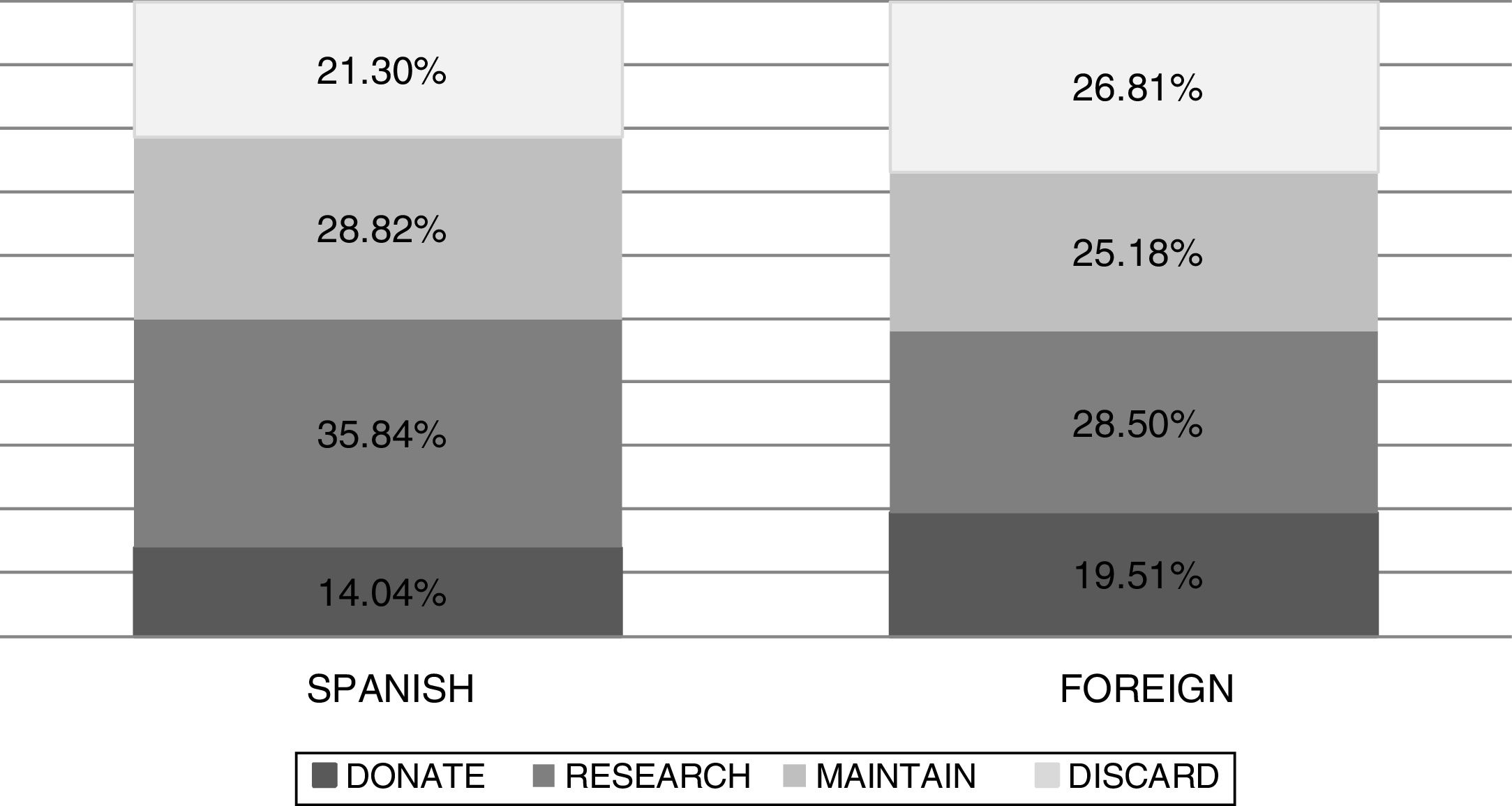
International patients decide to discard their pre-embryos for no other purpose (26.81% vs 21.30%; p-value: <0.05) or donate them to other couples (19.56% vs 14.04; p-value: <0.05) in greater proportion than national patients. In contrast, the percentage of national patients who decide to donate their embryos to research is greater than that of international patients (35.84% vs 28.50%; p-value: <0.05).
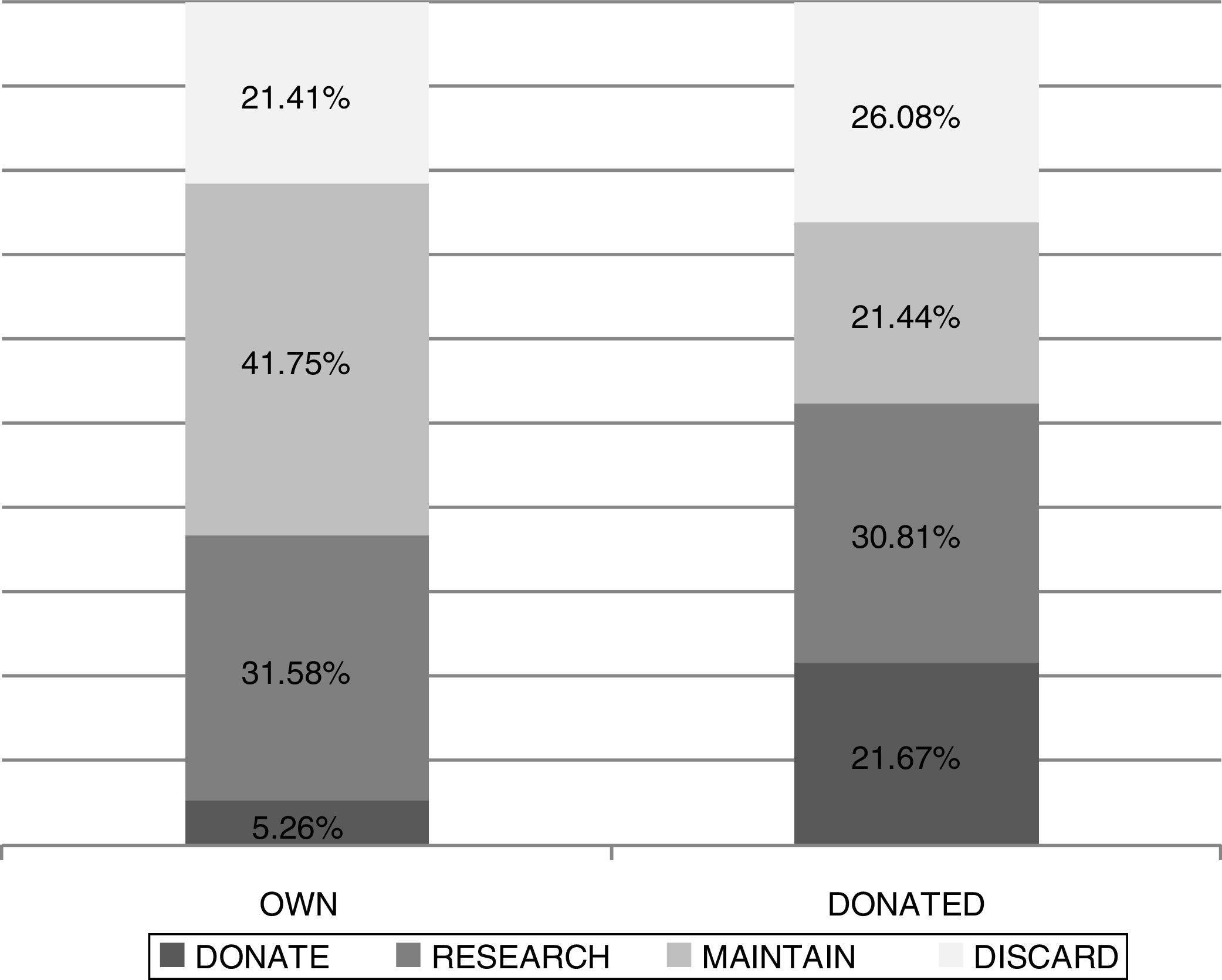
When we compared the responses obtained in terms of the origin of the oocytes (own or donated), we found that those who used donated oocytes decided to donate them to other couples in a higher percentage than those who used their own oocytes (21.67% vs 5.26%; p-value: >0.05). Patients who used donated oocytes decided to keep their pre-embryos in a lower percentage than patients who used their own oocytes (21.44% vs 41.75; p-value: <0.05).
ConclusionsAccording to this study, maternal age, nationality and origin of the oocytes are factors that can influence patients’ decisions about what to do with their surplus embryos from assisted reproduction cycles. In addition, it reiterates as in other studies that an improvement in the processes and circuits is necessary to obtain a greater number of responses from patients more.
Con los avances en las técnicas de reproducción asistida, y sobre todo gracias a la implementación de la vitrificación, cada vez son más los preembriones excedentes en los ciclos de reproducción asistida.
Material y métodosEstudio observacional retrospectivo.
ResultadosLa edad materna de las pacientes que decidieron donar sus preembriones a otras pacientes (41,38 ± 4,55) fue superior que la de aquellas que prefirieron donar a investigación (39,56 ± 4,89), mantenerlos para futuro uso (37,38 ± 4,72) o descartarlos sin ningún otro fin (40,87 ± 5,21); p-valor: < 0,05.
Las pacientes internacionales decidieron descartar sus preembriones sin ningún otro fin (26,81 vs. 21,30%; p-valor: < 0,05) o donar a otras parejas (19,56 vs. 14,04%; p-valor: < 0,05), en mayor proporción que las pacientes nacionales. En cambio, el porcentaje de pacientes nacionales que decidieron donar sus embriones a investigación fue mayor que el de las internacionales (35,84 vs. 28,50%; p-valor: < 0,05).
Cuando comparamos las respuestas obtenidas en función del origen de los ovocitos (propios o donados), se encontró que las que usaron ovocitos donados decidían en mayor porcentaje donarlos a otras parejas, que las que usaron ovocitos propios (21,67 vs. 5,26%; p-valor: > 0,05). Las pacientes que usaron ovocitos donados decidían, en menor porcentaje, mantener sus preembriones, que las pacientes que usaron ovocitos propios (21,44 vs. 41,75%; p-valor: < 0,05).
ConclusionesSegún este estudio, edad materna, nacionalidad y origen de los ovocitos son factores que pueden influir en la decisión de las pacientes sobre qué hacer con sus embriones excedentes de ciclos de reproducción asistida. Además reitera, como en otros estudios, que es necesaria una mejora de los procesos y circuitos para obtener un mayor número de respuestas, por parte de las pacientes, con mayor rapidez.
The number of surplus embryos from in vitro fertilization (IVF) cycles is increasing due to advances in Assisted Reproduction Techniques (ART) and to vitrification implementation. According to the 2014 National Activity Registry of the Spanish Fertility Society (SEF), on December 31st, 2014 there were a total of 364.765 stored embryos in our country (Registro Nacional de Actividad 2015-Registro SEF, 2015).
In order to avoid long embryo storage, in Spain the IVF patients must be informed by clinicians of the options offered by the Assisted Reproduction Spanish Law 14/2006. According to this law, patients must choose what to do with their surplus embryos in case they have. Those patients who do not want to use their cryopreserved embryos can donate them to other patients, to research projects, or stop their storage with no other finality. Before the donation of embryos to a research project, patients have to be informed of the project's goal and sign an informed consent approving the use of their embryos for that specific project.
Those patients who want to donate their embryos to other patients for reproductive use have to meet some requirements such as not suffering any serious inherited disease, having negative serologies for HIV, hepatitis B, hepatitis C, and syphilis, and the maternal age has to be under or equal to 35 years at the time of cryopreservation of the embryo. Clinical experts must decide if patients can donate their embryos for reproductive uses after the assessment of their medical histories. Patients can also decide not to give any use to their cryopreserved embryos and thus stop their storage and conservation. At the same time, embryo storage and conservation will also stop if doctors in charge and external independent medical specialists consider that patients do not meet the clinical requirements to perform IVF techniques.
Centers must contact every two years with patients possessing cryopreserved embryos to revalidate or renew their decision about their embryos. Patients can change their mind at any time, as long as embryos are available. In the case that patients do not reply to two consecutive renewals for the disposition of their cryopreserved embryos, these embryos will remain at the center's disposal. In this case, centers will be able to use them for any purpose.
The main goal of this study is to describe decisions taken by patients referring to their cryopreserved embryos. Moreover, it also answers if factors such as nationality, maternal age, the origin of the oocytes, marital status, and previous cycle outcome are correlated both, to the frequency of replying and with the patients’ decision.
MethodsThis is a retrospective observational study that analyzes the decisions of 2898 patients about their cryopreserved embryos. A letter was sent to patients two years after the IVF cycle, asking them to select an option for the disposition of their cryopreserved embryos. IVF cycles for these patients were performed at our center between April 2008 and December 2014.
In our center, when patients decide to donate their embryos for reproductive uses, clinical histories are assessed by a team of embryologists, doctors, and psychologists. Patients will be asked to sign a contract where they accept to carry out that donation and to perform a psychological test. Patients that wish to donate their embryos to research projects will receive a letter with the project's information, and thus accept or reject their participation.
The factors that were correlated with patients’ decisions were: patients’ age and nationality (Spanish or not), the origin of the oocytes (own or donated), and the delivery of a living newborn after the IVF cycle. The origin of international patients was Italian (52%), French (18%), British (12%), Swiss (6%), German (4%), other nationalities (8%).
IBM SPSS Statistics for Windows version 19 (IBM corp., Armonk N.Y. the USA) was used for the statistical study. All variables in this study are categorical, and thus Chi-square Test was applied, except for the study of maternal age, where the Anova Test was used. p<0.05 was considered statistically significant. The sample size concept was not applied in this study, as all the population available was included, 2898 patients with cryopreserved embryos who received the letter to choose their disposition.
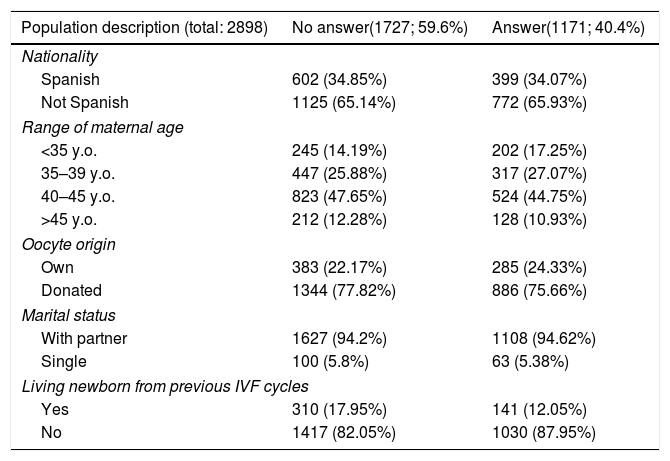
ResultsA total of 1171 replies to the letters were received, corresponding to 40.42% of the contacted patients. Due to this low percentage in answers, we decided to study if there was any factor affecting the decision of replying (Table 1).
Percentages of responses to letters according to social characteristics.
| Population description (total: 2898) | No answer(1727; 59.6%) | Answer(1171; 40.4%) |
|---|---|---|
| Nationality | ||
| Spanish | 602 (34.85%) | 399 (34.07%) |
| Not Spanish | 1125 (65.14%) | 772 (65.93%) |
| Range of maternal age | ||
| <35 y.o. | 245 (14.19%) | 202 (17.25%) |
| 35–39 y.o. | 447 (25.88%) | 317 (27.07%) |
| 40–45 y.o. | 823 (47.65%) | 524 (44.75%) |
| >45 y.o. | 212 (12.28%) | 128 (10.93%) |
| Oocyte origin | ||
| Own | 383 (22.17%) | 285 (24.33%) |
| Donated | 1344 (77.82%) | 886 (75.66%) |
| Marital status | ||
| With partner | 1627 (94.2%) | 1108 (94.62%) |
| Single | 100 (5.8%) | 63 (5.38%) |
| Living newborn from previous IVF cycles | ||
| Yes | 310 (17.95%) | 141 (12.05%) |
| No | 1417 (82.05%) | 1030 (87.95%) |
No significant differences were detected according to patients’ nationality (national patients 60.13%; international patients 59.30%), maternal age (<35 years 54.81%; 35–39 years 58.51%; 40–45 years 61.10%; >45 years 62.35%), oocytes origin (own oocytes 57.33%; donated oocytes 60.27%) or marital status (with partner 59.49%; without partner 61.35%). Interestingly, patients with at least a living newborn from previous IVF cycles presented a significantly higher answer rate to letters asking for the disposition of their embryos, than patients with negative results in previous IVF cycles (42.09% vs 31.26%; p<0.05).
When patients replayed, no significant differences were detected between the different options for embryo disposition: keeping for future use 26.39%, donate for reproductive use 17.68%; donate for research projects 31.00%; discard embryos with no further use 24.93%.
Maternal age was found to be higher in those patients that decided to donate their embryos to other patients (41.38±4.55), than in those that preferred to donate them to research (39.56±4.89), keep for further use (37.38±4.72) or discard them (40.87±5.21) p-value<0.05. Comparing decisions within age groups (Fig. 1), younger patients prefer to keep embryos for further reproductive use, and this percentage decreases with maternal age increase. Older patients are more prone to discard their embryos with no further use.
Concerning patients’ nationality (Fig. 2), we found that international patients are more predisposed to discard their embryos (26.81% vs 21.30%; p-value: <0.05) or donate them to other couples (19.56% vs 14.04; p-value: 0.05) than national patients. At the same time, the number of Spanish patients that prefer to donate their embryos for research purposes is higher than that of international patients (35.84 vs 28.50%; p-value: <0.05).
When comparing answers according to oocyte origin (own or donated) (Fig. 3), patients with donated oocytes were more prone to donate their cryopreserved embryos to other couples than those that got the embryos with their own oocytes (21.67% vs 5.26%; p-value: >0.05). Regarding the decision to keep or not the embryos, those patients who used donated oocytes decided to maintain their embryos in a lower proportion than the patients who used their own oocytes. (21.44% vs 41.75; p-value: <0.05).
Having a newborn did not influence the response rate to the letter we sent to patients asking for their decisions about what to do with the remaining embryos.
DiscussionEmbryo cryopreservation supposed a great advance in the IVF field, and it has become a routinely used technique since 1983 when the first child conceived by cryopreserved embryo transfer was born (Trounson and Mohr, 1983). From its implementation, embryo cryopreservation allowed the conservation of surplus embryos for their use in future cycles, increasing the success rate for each stimulation cycle and decreasing multiple pregnancy rates. Several protocols have been developed from the beginning of human embryo cryopreservation. These protocols differ in cryoprotectant concentration, equilibration time, cooling time, and used devices. The two techniques used more commonly are slow freezing and vitrification (Rienzi et al., 2017). The vitrification for human embryo preservation improved embryo survival results as well as accumulated results in IVF cycles. This is due to the use of high cryoprotectant concentrations, which solidify cells and allow lower cooling time. This step avoids crystal formation, which damages cells and leads to their degeneration (AbdelHafez et al., 2010).
The high survival rates in embryo vitrification allow a deferred transfer. In these cases, pre-embryo transfers are carried out in a different cycle than the stimulation one, which permits a higher control of the parameters allowing embryo implantation. Recently, embryo cryopreservation has been key to cycles of preimplantation genetic testing in the blastocyst stage, since the transfer is postponed until the genetic analysis is performed (Rienzi et al., 2017) and the transferable embryos are identified.
In our study, we found a very high percentage of patients (60% approximately) did not reply to the disposition of their cryopreserved embryos. This seems to be common in IVF centers around the world according to what several authors have been described in similar studies (De Lacey, 2007; Hammarberg and Leesa, 2006; Luna et al., 2009; McMahon and Sanders, 2009). In a recent USA's study, it is described that the percentage of no reply increased proportionally with the time that embryos had been cryopreserved. In that study, 73.6% of answers were obtained when embryos had been cryopreserved for a year, while this percentage decreased to 45.9% when embryos had been cryopreserved for 5 years (Apte et al., 2015). According to previously published data (Hammarberg and Leesa, 2006) together with our results, less than 50% of patients answer after 2 years. As expected, patients with negative results in previous IVF cycles are mostly represented in the no answer group.
The low response rate supposes an extra cost in embryos maintenance, storage problems (more space and cryogenic storage equipment needed), and a loss of time for the centers’ staff. The IVF centers should propose alternative circuits and improve processes to get the highest number of replies within the shortest time.
Reviewing the bibliography, we can consider that all countries give similar options for surplus embryos to their patients. The options to disposal, donate to research, and donate to other couples are available for example in the USA (Apte et al., 2015), Australia (Hammarberg and Leesa, 2006), France (Bruno et al., 2016), and Denmark (Bangsbøll et al., 2004). In Israel, couple's disposition form contains these three options: to continue the storage for fee, donation for research and discarding (Raz et al., 2016). Although no statistically significant differences in answers were identified in our study, the most chosen one was the donation for research consistent with other studies that described 42% (Hammarberg and Leesa, 2006), and 59% (Lanzendorf et al., 2010) of patients selected this option among the others. However, the decision of donating embryos could depend on patients’ age.
A previous study (Lanzendorf et al., 2010) observed that patients choosing to discard had a mean age of 35.9 years and patients choosing to donate to research had a mean age of 37.1 years, but the information included only 149 disposition requests. In our cohort of 1171 patients, we found that younger patients are more predisposed to maintain their embryos for themselves and that older patients prefer to donate them to other patients or simply discard them.
Other factors may influence patients’ decisions as the elapsed time since embryo cryopreservation or the origin of the oocytes (donated or own oocytes). Patients with cryopreserved embryos for a period of 2–4 years preferred to maintain them for further reproductive uses, and that patients with cryopreserved embryos for more than 10 years choose to interrupt their maintenance or donate them to research (Luna et al., 2006). In concordance with our study, the same authors who described this observation about the elapsed time also observed that patients who used donated oocytes were more prone to donate their embryos to other patients.
Around 75% of our patients come to our center to undergo oocyte donation cycles, which is permitted and anonymous in Spain. That could be the reason why those patients are more predisposed to discard their pre-embryos or donate them than the national ones.
One limitation of our study is that the software registering patient data only allows a patient's most recent decision to be exported for analysis. Therefore, we were unable to explore the initial decisions of those patients who changed their decisions.
ConclusionsIn conclusion, our results point out that the profile of patients who donate their embryos for reproductive uses are older women from other countries that had undergone IVF treatment with donated oocytes. This group of patients is also the most likely to discard their surplus embryos, probably due to the lower emotional attachment to them. The data reiterates the need for IVF centers in considering alternative protocols and improve processes to get the largest number of responses possible, since embryo storage is a growing problem.
DeclarationsEthics approval and consent to participateWritten informed consent was obtained from all participants, and the study was approved by the Hospital Clinic of Barcelona's Clinical Research Ethics Committee (project reference HCB/2015/0743, approved 18 September 2015).
Consent for publicationNot applicable.
Availability of data and materialsAll data generated or analyzed during this study are included in this published article.
FundingFunding was not required to perform the project.
Conflict of interestsNone of the authors declares competing for financial interests.
The authors want to thank the whole center team, especially the people from the different departments in charge of vitrified pre-embryo maintenance renewals.