Lymphangioleiomyomatosis (LAM) is a rare disease that affects women almost exclusively. We aimed to determine the psychological profile in patients with LAM, and their potential association with sociodemographic and clinical features, and to know their role in coping with the disease.
Material and methodsCross-sectional and descriptive study in collaboration with the Spanish Association of LAM (AELAM). The variables measured were: socio-demographic, psychological (anxiety, depression, demoralization, spirituality, resilience, social support), clinical (treatment) and health-related quality of life.
ResultsWe studied 87 LAM patients, with a mean (SD) age of 47.7 (7.7) years, and time since diagnose was 10.1 (5.4) years. 75.9% of patients were receiving sirolimus or everolimus, and oxygen therapy was required in 34.5% of patients. Anxiety was found in 46% of patients, depression in 55%, while only 2% presented demoralization and 14% deficit in spirituality. Social support and resilience were adequate. The “non-severe” group (without oxygen therapy) presented worse results in anxiety. A structural equation model to explore association between variables, showed very adequate fit indices: χ2(14)=29.743 (p=.074); CFI=.983; TLI=.967; SRMR=.058; RMSEA=.075[.000–.128]. The model identifies resilience, spirituality and social support as “protective factors” from anxiety, depression, and demoralization.
ConclusionsThis study performed on a large series of women with LAM describes their psychological profile, in addition to showing how they cope with the disease. We have found that other psychological constructs, such as perceived social support and resilience, are protective factors. Early psychological evaluation and intervention is necessary to reduce comorbidities and prevent mental health problems in women with LAM.
La linfangioleiomiomatosis (LAM) es una enfermedad rara que afecta casi exclusivamente a las mujeres. Nuestro objetivo fue determinar el perfil psicológico en los pacientes con LAM, y su potencial asociación con características sociodemográficas y clínicas, y conocer su papel en el afrontamiento de la enfermedad.
Material y métodosEstudio transversal y descriptivo en colaboración con la Asociación Española de LAM (AELAM). Las variables medidas fueron: sociodemográficas, psicológicas (ansiedad, depresión, desmoralización, espiritualidad, resiliencia, apoyo social), clínicas (tratamiento) y calidad de vida relacionada con la salud.
ResultadosSe estudiaron 87 pacientes con LAM, con una edad media (DE) de 47,7±7,7 años y un tiempo desde el diagnóstico de 10,1±5,4 años. El 75,9% de los pacientes estaban recibiendo sirolimus o everolimus, y el 34,5% de los pacientes requirió oxigenoterapia. La ansiedad se encontró en el 46% de los pacientes, la depresión en el 55%, mientras que solo el 2% presentó desmoralización y el 14% déficit en la espiritualidad. El apoyo social y la resiliencia fueron adecuados. El grupo «no grave» (sin oxigenoterapia) presentó peores resultados en ansiedad. Un modelo de ecuaciones estructurales para explorar asociación entre variables, mostró índices de ajuste muy adecuados: χ2(14)=29,743 (p=0,074); CFI=0,983; TLI=0,967; SRMR=0,058; RMSEA=0,075 (0,000-0,128). El modelo identifica la resiliencia, la espiritualidad y el apoyo social como «factores protectores» contra la ansiedad, la depresión y la desmoralización.
ConclusionesEste estudio realizado en una amplia serie de mujeres con LAM describe su perfil psicológico, además de mostrar cómo afrontan la enfermedad. Hemos descubierto que otros constructos psicológicos, como el apoyo social percibido y la resiliencia, son factores protectores. La evaluación e intervención psicológica temprana es necesaria para reducir las comorbilidades y prevenir problemas de salud mental en mujeres con LAM.
Lymphangioleiomyomatosis (LAM) is a rare disease characterized by diffuse lung cysts that affects women almost exclusively, especially those of childbearing age. LAM incidence is low, frequently in the context of tuberous sclerosis complex (TSC).1,2 It is characterized by an abnormal proliferation of immature smooth muscle cells, so called LAM cells, which grow aberrantly in the airway, parenchyma, lymphatic and pulmonary blood vessels, which evolve towards respiratory failure. It is a multisystemic condition, producing abdominal tumours.3
The most common symptom of LAM is dyspnoea, but fatigue and cough are also frequent. In a majority of patients, a history of pneumothorax is present. Abdominal symptoms are less frequent and most of the times related with renal angiomyolipoma.4,5
Data from a national registry in the U.S. showed that patients with LAM patients frequently experience impairments in quality of life (QoL), with a special impact in physical and mental components, and the activity dimension, measured by SF-36 and SGRQ questionnaires.6 However, to date the emotional and psychological impact on women with LAM has barely been explored. Some studies have found that patients perceive the physical symptoms from LAM to be intrusive and limiting. Women living with LAM are frustrated by their physical limitations, and they worry about what the future will be like if the disease progresses.7 On the one hand, data from LAM patients that undergo lung transplant highlight the presence of anxiety and depressive disorders.8 On the other hand, data from programmes of pulmonary rehabilitation demonstrate the presence of depression in 41% of analyzed patients.9 Anxiety, depression or demoralization, have been identified in other interstitial lung diseases (ILD) such as idiopathic pulmonary fibrosis (IPF).10
Patients with LAM are mainly middle-aged women and the disease affects their everyday activities and motivation. Furthermore, the challenges in diagnosis, management, and the prognosis may associate an emotional and psychological impact for these patients and their families. Anxiety, and depression could also be present in patients with LAM, decreasing their QoL. Understanding the psychological profile and needs of patients with LAM would allow to implement care plans to optimize their management and improving QoL.
The objective of this study was to determine the psychological needs profile in patients with LAM, and their potential association with sociodemographic and clinical features, and to know their role in coping with the disease.
Material and methodsDesign, setting, and participantsWe performed an observational, cross-sectional and descriptive study, with a questionnaire survey in collaboration with the Spanish Association of LAM (AELAM). Inclusion criteria were: diagnosis of LAM based on 2017 ATS//JRS/guidelines.11 The only exclusion criteria were decline to participate or not signing the informed consent. The study protocol followed and endorsed the STROBE criteria,12 and it was approved by the Clinical Research Ethics Committee of Hospital Universitario de la Princesa (Register Number 3775). The authors of the study declare that we have the informed consent of the participants in the study.
ProceduresDuring the annual meeting of the Spanish LAM association, informed consent and questionnaires were distributed to potential participating patients, coming from all over the Spanish territory. Once the questionnaires were answered, the patients sent them electronically to the psychologist responsible for the study, either directly or through the association's secretary.
Clinical and psychological features investigated in the surveySocio demographic, psychological, clinical and QoL information were assessed through different variables. The variables measured and the questionnaires used were:
- -
Socio demographic: Age, location, marital status, educational level, employment status, number of children.
- -
Clinical variables: Time since diagnosis, Treatment (home oxygen therapy, pharmacological, none), The severity of the disease was assessed taking into account the use of long-term oxygen therapy (LTOT). Oxygen therapy is considered necessary when there is a situation of acute or chronic hypoxaemia with pO2 below 55–60mmHg, a figure that corresponds to a haemoglobin saturation of 90%.
- -
The Beck Depression Inventory (BDI) is a 21-item, self-report rating questionnaire that measures characteristic attitudes and symptoms of depression.13 The BDI demonstrates high internal consistency, with alpha coefficients of .87 in its Spanish validation.
- -
State-Trait Anxiety Inventory (STAI). It is made up of two separate self-assessment scales that measure two independent concepts of anxiety, as state and as trait. Trait of anxiety refers to the individual tendency to react anxiously, while the “state of anxiety” refers to transient and fluctuating anxiety It has high reliability indicators (α values between .94 and .98).14
- -
Spirituality (GES). It consists of six open questions designed to create and share a space of intimate communication with the patient and establish a climate of trust, followed by eight items that evaluate spirituality as a general factor with three dimensions: intrapersonal, interpersonal and transpersonal.15 The original Cronbach's alpha of this scale was .72. The eight items are answered with a scale of five Likert-type points, with answers ranging from 0 (nothing) to 4 (much).
- -
Brief Scale of Demoralization. 5 item Likert scale that assesses the demoralization syndrome from 1 (totally disagree) to 5 (totally agree).16 The original Cronbach's alpha was .920.
- -
Brief Scale of Resilient Coping. This scale of four items focuses on the tendency to effectively use coping strategies in flexible, committed ways to actively solve problems despite stressful circumstances.17 It was adapted and validated in Spain with an internal consistency of .79. Each item is scored on a scale of five points, from 1 (totally agree) to 5 (totally disagree), with the highest scores reflecting a greater capacity for recovery.
- -
Duke-UNC. Functional Social Support Questionnaire. Questionnaire of quantitative evaluation of perceived social support in relation to two aspects: people to whom intimate feelings can be communicated and persons expressing positive feelings of empathy.18 It collects values referring to Confidential Support and referrals to Affective Support. Each aspect is evaluated with a Likert scale with 5 options (1 Much less than what I want to 5 As much as I wish). The Spanish version of the questionnaire shows a reliability of .80.
- -
Global Health Status. Two items of the EORTC-QLQ-C30 were used, which make up the Global Health Scale factor.19 The items evaluate the perceived physical quality of life and the global state of health. The QLQ-C30 is currently used in several types of studies in subjects with both cancer and other advanced chronic diseases.
- -
EuroQoL-5D-5L. The EQ-5D-5L assesses five domains: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each domain are scored at different levels of increasing severity from 1 (no problems in the dimension) to 5 (extreme problems).20 The patient is asked to indicate his/her health state by ticking the box next to the most appropriate statement in each of the five domains.
Descriptive statistics were calculated for all variables. Then, Pearson and Spearman correlations were used to test the significance of associations. Analysis of variance (ANOVA) was used to test relationships with categorical variables. T-tests were used to analyze differences between groups by severity. To study the relationship between all the variables, a structural equation model was carried out. To determine the global fit of the model, the Kline21 criteria were taken into account: Chi-square to assess the general fit and the discrepancy between the sample and the adjusted covariance matrices, the comparative fit index (CFI), the Tucker Lewis Index (TLI), the root Mean Square Error of Approximation (RMSEA) and the Standardized Root Mean Residual (SRMR) in addition to the R2 (percentage of variation of the variable). A p value lower than 0.05 was considered for statistical significance.
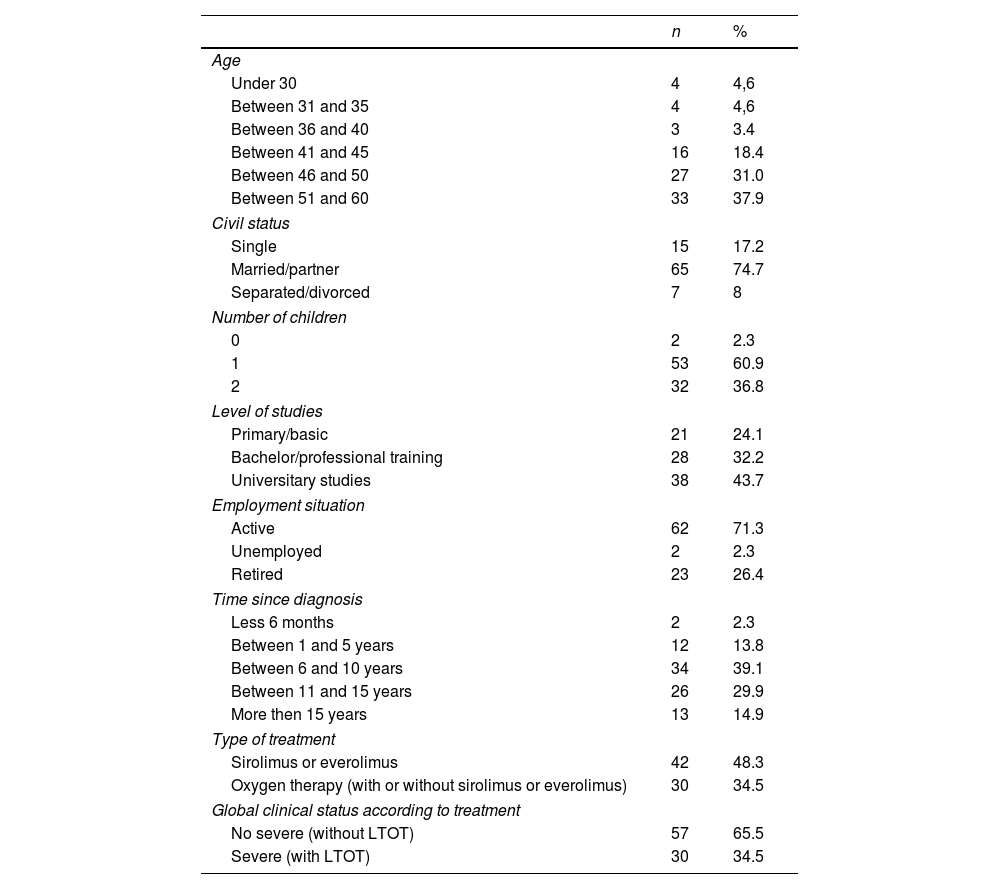
ResultsEighty-seven women diagnosed with LAM participated in the study. The Spanish LAM Patients’ Association includes 140 members from different regions of Spain, which represents 63% of the total number registered in the country. The mean age (SD) was 47.7 (7.7) years and time since diagnose was 10.1 (5.4) years. Most women were mother of one or two children (97%), had a partner or husband (75%), and had completed university studies (44%) or medium level of studies (another 32%). At inclusion in the study, 71% of patients were actively working, and 26.4% were retired. The delay in LAM diagnosis was longer than 6 years in 84% of the patients. Regarding treatment, 75.9% of patients were receiving sirolimus or everolimus, and oxygen therapy was required in 34.5% of patients. None had a lung transplant (Table 1).
Demographic and clinical characteristics of participating LAM patients.
| n | % | |
|---|---|---|
| Age | ||
| Under 30 | 4 | 4,6 |
| Between 31 and 35 | 4 | 4,6 |
| Between 36 and 40 | 3 | 3.4 |
| Between 41 and 45 | 16 | 18.4 |
| Between 46 and 50 | 27 | 31.0 |
| Between 51 and 60 | 33 | 37.9 |
| Civil status | ||
| Single | 15 | 17.2 |
| Married/partner | 65 | 74.7 |
| Separated/divorced | 7 | 8 |
| Number of children | ||
| 0 | 2 | 2.3 |
| 1 | 53 | 60.9 |
| 2 | 32 | 36.8 |
| Level of studies | ||
| Primary/basic | 21 | 24.1 |
| Bachelor/professional training | 28 | 32.2 |
| Universitary studies | 38 | 43.7 |
| Employment situation | ||
| Active | 62 | 71.3 |
| Unemployed | 2 | 2.3 |
| Retired | 23 | 26.4 |
| Time since diagnosis | ||
| Less 6 months | 2 | 2.3 |
| Between 1 and 5 years | 12 | 13.8 |
| Between 6 and 10 years | 34 | 39.1 |
| Between 11 and 15 years | 26 | 29.9 |
| More then 15 years | 13 | 14.9 |
| Type of treatment | ||
| Sirolimus or everolimus | 42 | 48.3 |
| Oxygen therapy (with or without sirolimus or everolimus) | 30 | 34.5 |
| Global clinical status according to treatment | ||
| No severe (without LTOT) | 57 | 65.5 |
| Severe (with LTOT) | 30 | 34.5 |
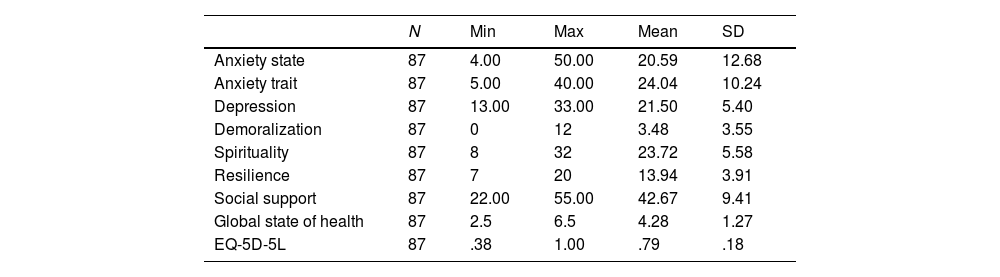
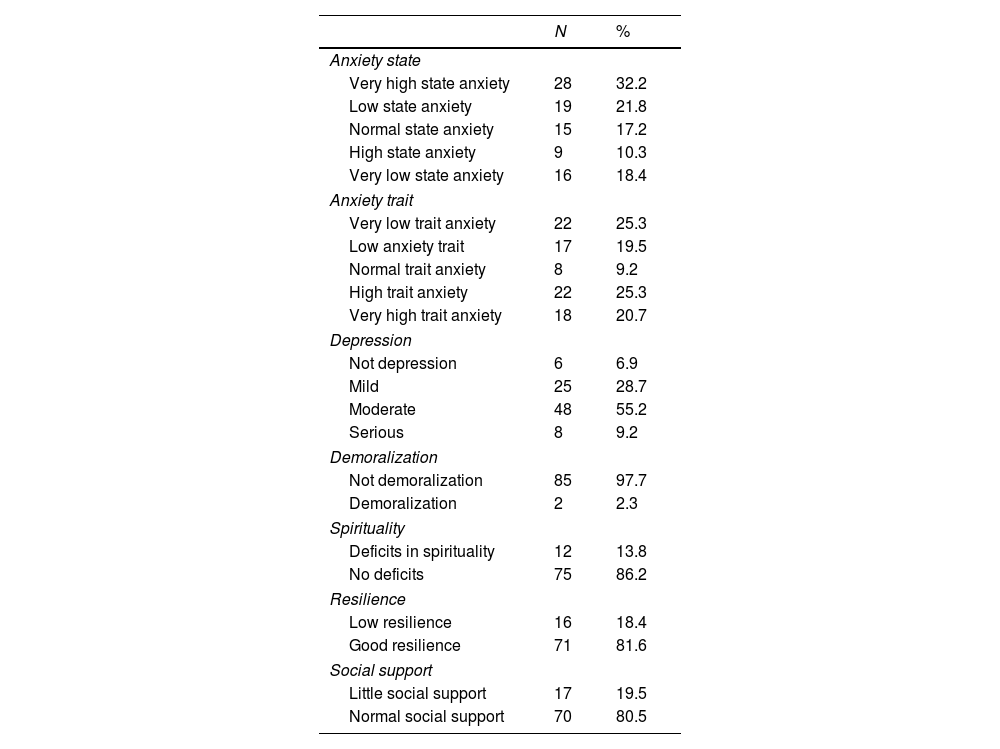
Regarding their psychological evaluation, anxiety and depression were frequently identified. The “trait anxiety” was present as low level in 54% of patients and as high levels in 29%. The “state of anxiety” was also prevalent (90%), in high level (46%) or low level (44%). Regarding depression, the results indicate the presence of moderate depression in 55% of the patients (21.50+5.4), followed by 29% of patients with mild depression. (21.50+5.4). Only 2% of the patients presented demoralization (3.48+3.5) and 14% or deficit in the spiritual area (23.72+5.58). Most patients had adequate social support (80%, 42.68+9.41) and 82% showed good resilience (13.94+3.91) (Tables 2 and 3).
Descriptions of the psychological and quality of life evaluation (scores).
| N | Min | Max | Mean | SD | |
|---|---|---|---|---|---|
| Anxiety state | 87 | 4.00 | 50.00 | 20.59 | 12.68 |
| Anxiety trait | 87 | 5.00 | 40.00 | 24.04 | 10.24 |
| Depression | 87 | 13.00 | 33.00 | 21.50 | 5.40 |
| Demoralization | 87 | 0 | 12 | 3.48 | 3.55 |
| Spirituality | 87 | 8 | 32 | 23.72 | 5.58 |
| Resilience | 87 | 7 | 20 | 13.94 | 3.91 |
| Social support | 87 | 22.00 | 55.00 | 42.67 | 9.41 |
| Global state of health | 87 | 2.5 | 6.5 | 4.28 | 1.27 |
| EQ-5D-5L | 87 | .38 | 1.00 | .79 | .18 |
Psychological evaluation percentages.
| N | % | |
|---|---|---|
| Anxiety state | ||
| Very high state anxiety | 28 | 32.2 |
| Low state anxiety | 19 | 21.8 |
| Normal state anxiety | 15 | 17.2 |
| High state anxiety | 9 | 10.3 |
| Very low state anxiety | 16 | 18.4 |
| Anxiety trait | ||
| Very low trait anxiety | 22 | 25.3 |
| Low anxiety trait | 17 | 19.5 |
| Normal trait anxiety | 8 | 9.2 |
| High trait anxiety | 22 | 25.3 |
| Very high trait anxiety | 18 | 20.7 |
| Depression | ||
| Not depression | 6 | 6.9 |
| Mild | 25 | 28.7 |
| Moderate | 48 | 55.2 |
| Serious | 8 | 9.2 |
| Demoralization | ||
| Not demoralization | 85 | 97.7 |
| Demoralization | 2 | 2.3 |
| Spirituality | ||
| Deficits in spirituality | 12 | 13.8 |
| No deficits | 75 | 86.2 |
| Resilience | ||
| Low resilience | 16 | 18.4 |
| Good resilience | 71 | 81.6 |
| Social support | ||
| Little social support | 17 | 19.5 |
| Normal social support | 70 | 80.5 |
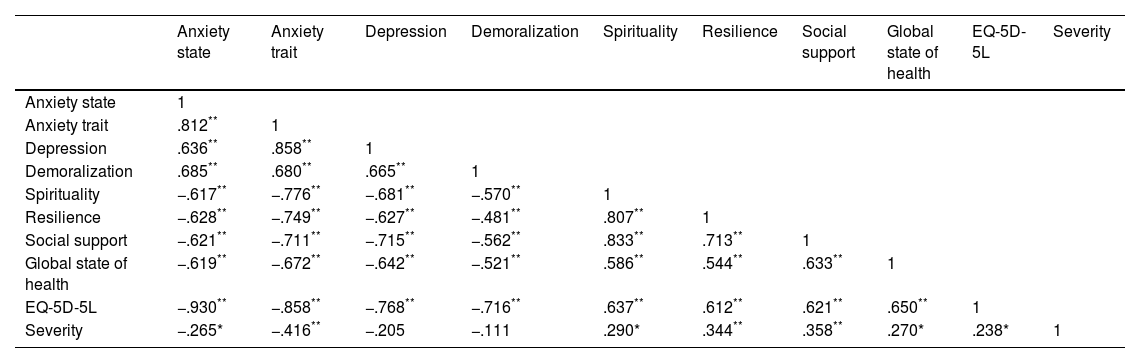
The bivariate correlation map (Table 4) shows statistically significant correlations between all the variables, and in the expected direction. It is observed that patients who present anxiety usually have depression and demoralization, as well as worse resilience, spirituality, deficient social support and worse quality of life, in addition to finding a significant correlation between the presence of psychological problems and severity.
Map of bivariate correlations between psychological variables and LAM severity.
| Anxiety state | Anxiety trait | Depression | Demoralization | Spirituality | Resilience | Social support | Global state of health | EQ-5D-5L | Severity | |
|---|---|---|---|---|---|---|---|---|---|---|
| Anxiety state | 1 | |||||||||
| Anxiety trait | .812** | 1 | ||||||||
| Depression | .636** | .858** | 1 | |||||||
| Demoralization | .685** | .680** | .665** | 1 | ||||||
| Spirituality | −.617** | −.776** | −.681** | −.570** | 1 | |||||
| Resilience | −.628** | −.749** | −.627** | −.481** | .807** | 1 | ||||
| Social support | −.621** | −.711** | −.715** | −.562** | .833** | .713** | 1 | |||
| Global state of health | −.619** | −.672** | −.642** | −.521** | .586** | .544** | .633** | 1 | ||
| EQ-5D-5L | −.930** | −.858** | −.768** | −.716** | .637** | .612** | .621** | .650** | 1 | |
| Severity | −.265* | −.416** | −.205 | −.111 | .290* | .344** | .358** | .270* | .238* | 1 |
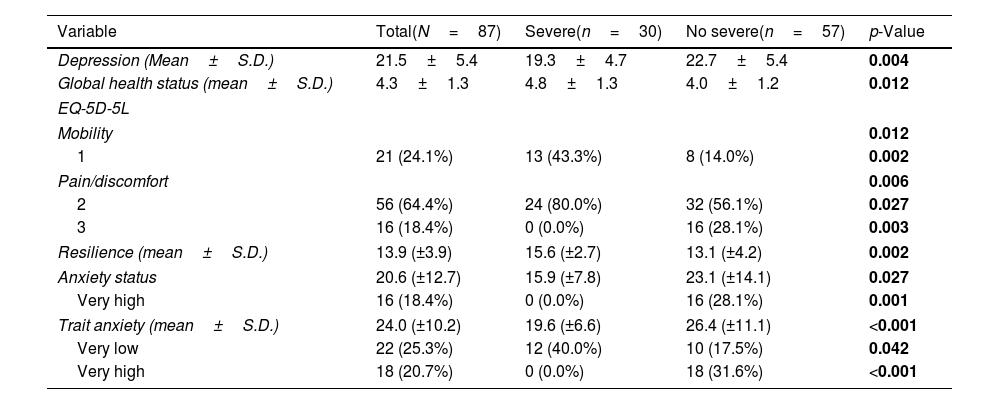
Finally, we explored differences in erent measures described above, by LAM severity. Statistically significant differences were found in quality of life in the dimensions of mobility (p=.012), pain/discomfort (p=.006), depression (p=.004), global state of health (p=.012), resilience (p=.002), and trait anxiety (p=.001). The patients in the group considered “non-severe” presented worse results in state anxiety and trait anxiety, depression, pain/discomfort, while the patients considered “severe” presented less trait anxiety and greater resilience (Table 5).
Differences by severity (only statistically significant results are shown).
| Variable | Total(N=87) | Severe(n=30) | No severe(n=57) | p-Value |
|---|---|---|---|---|
| Depression (Mean±S.D.) | 21.5±5.4 | 19.3±4.7 | 22.7±5.4 | 0.004 |
| Global health status (mean±S.D.) | 4.3±1.3 | 4.8±1.3 | 4.0±1.2 | 0.012 |
| EQ-5D-5L | ||||
| Mobility | 0.012 | |||
| 1 | 21 (24.1%) | 13 (43.3%) | 8 (14.0%) | 0.002 |
| Pain/discomfort | 0.006 | |||
| 2 | 56 (64.4%) | 24 (80.0%) | 32 (56.1%) | 0.027 |
| 3 | 16 (18.4%) | 0 (0.0%) | 16 (28.1%) | 0.003 |
| Resilience (mean±S.D.) | 13.9 (±3.9) | 15.6 (±2.7) | 13.1 (±4.2) | 0.002 |
| Anxiety status | 20.6 (±12.7) | 15.9 (±7.8) | 23.1 (±14.1) | 0.027 |
| Very high | 16 (18.4%) | 0 (0.0%) | 16 (28.1%) | 0.001 |
| Trait anxiety (mean±S.D.) | 24.0 (±10.2) | 19.6 (±6.6) | 26.4 (±11.1) | <0.001 |
| Very low | 22 (25.3%) | 12 (40.0%) | 10 (17.5%) | 0.042 |
| Very high | 18 (20.7%) | 0 (0.0%) | 18 (31.6%) | <0.001 |
The differences found were not explained by the severity itself (F[1]=.009; p=.924) but by the years since diagnosis, both for state anxiety (F[3]=8.325; p<.001), as for resilience (F[3]=6.650; p<.001), as for demoralization (F[3]=4.981; p=.003]); although for depression (F[3]=2.451; p=.069) and global state of health (F[3]=2.297; p=.084) it was not significant. In the post hoc tests, these differences occurred among the patients with more years since diagnosis. In addition, it was found that the greater resilience, the patients presented better mood (F[12]=10,377; p<.001; η2=.194), better anxiety state (F[12]=15,309; p<.001; η2=.713) and better global state of health (F[12]=5995; p<.001; η2=.493).
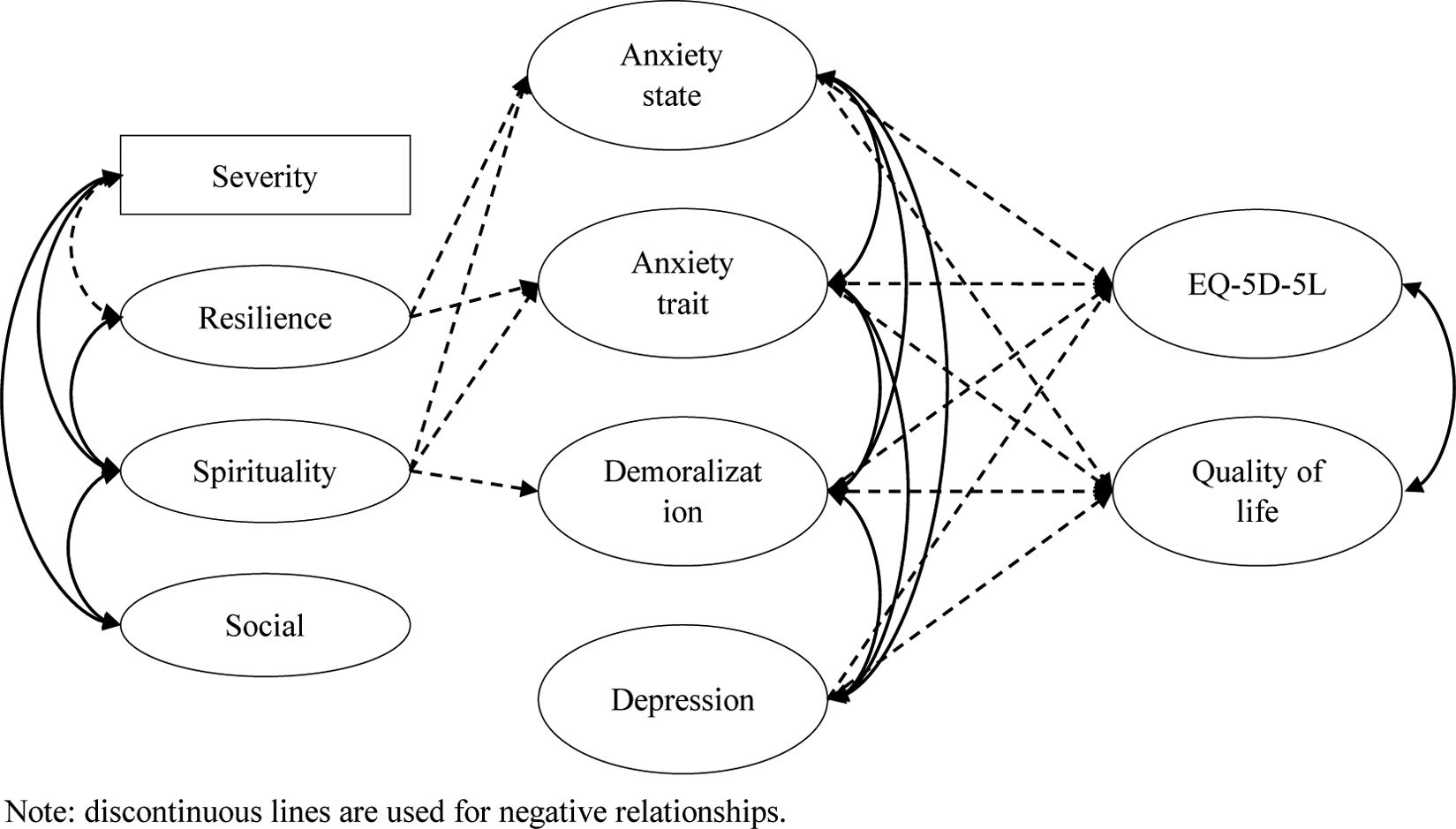
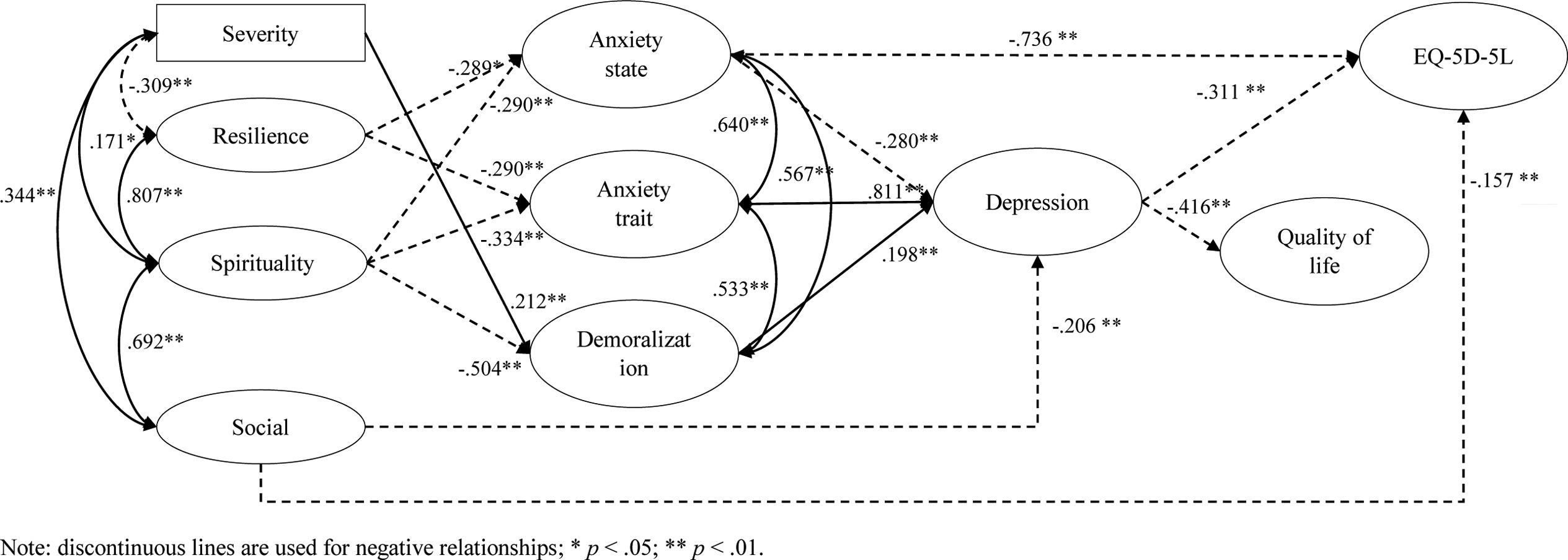
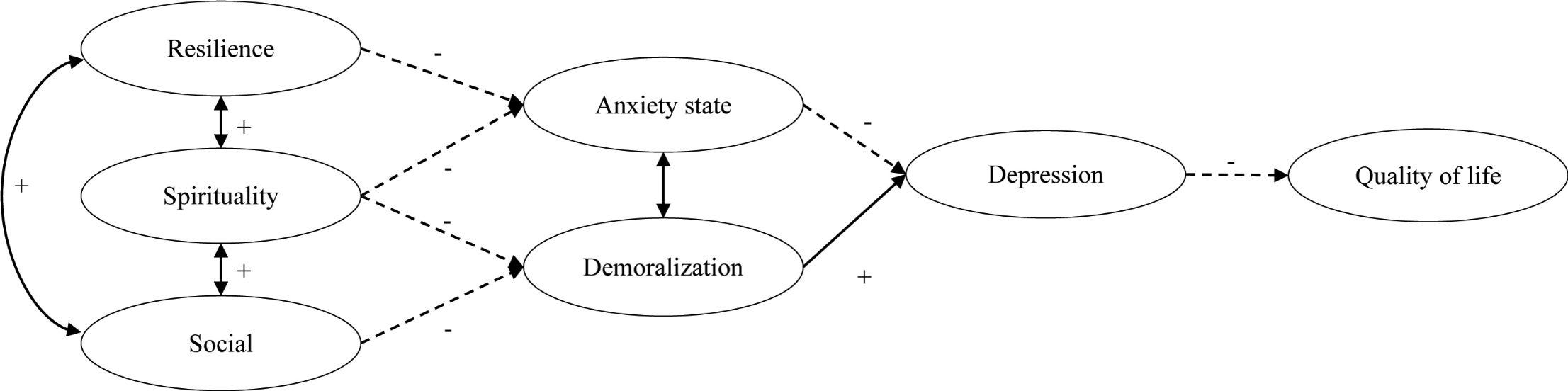
Finally, to assess the association between all variables studied, a structural equation model was used, and Fig. 1 shows the initial proposed model. The hypothesis we evaluated was that patients with worse clinical status (severity) have better resilience and spirituality, as well as better social support. Resilience and spirituality could be understood as “protective factors”, along with social support. These factors cause patients to present less state anxiety, less trait anxiety, less depression and less demoralization; and they in turn increase their quality of life.
The final resulting model is shown in Fig. 2. This model presented very adequate fit indices χ2(14)=29.743 (p=.074), CFI=.983; TLI=.967; SRMR=.058; RMSEA=.075 [.000–.128]. It was found that resilience and spirituality had an ability to explain state anxiety (R2=.417) and trait anxiety (R2=.639). Furthermore, spirituality and severity had the capacity to explain demoralization (R2=.355). In turn, state anxiety, trait anxiety and demoralization explained depression (R2=.785), while depression had the capacity to explain quality of life (R2=.485) and quality of life measured with Euroqol-5D-5L (R2=.916). Regarding this last relationship, it is important to note the statistically significant relationship with social support with depression and with quality of life.
DiscussionThe profile found showed a relationship between the psychological variables: those patients with worse levels of anxiety (state and trait) presented altered mood (depression), demoralization, worse spirituality, and resilience. We found high levels of anxiety and depression in different spectrums, while no demoralization or deficit in the spiritual dimension were found. Sociodemographic data suggest that these patients have adequate social support (80%) and good resilience (82%). They also showed worse quality of life and poor perception of social support. Data were analyzed considering the severity of LAM, and significant differences were found: patients with less severity (no oxygen therapy) had worse mood, worse overall health status (global state of health and EQ-5D-5L), worse resilience and more anxiety. This seems to be related to the time since diagnosis: those women who had been diagnosed with LAM for longer had a better emotional state. In turn, those women with better resilience had a better state of mind, less anxiety, and a higher perception of their overall state of health. It seems that as the years go by, LAM women who improve their resilience are able to better adapt to changes in the disease, with better mood, less anxiety, and a better perception of their disease. It was observed that patients with less severity presented worse mood, worse global health status, worse resilience and more anxiety state.
In general, it seems that patients who present worse clinical status (severity) as measured by the use of oxygen therapy, show better resilience and spirituality, and have better social support. This seems to indicate that resilience, spirituality and social support act as “protective factors”, since when there is a good level in these variables, patients present less anxiety (state and trait), and also have better spirituality, there is less demoralization. In another direction, depression is related to the presence of anxiety, demoralization, and low social support, and is associated with a lower quality of life. This finding indicates the importance of aspects such as resilience, spirituality and social support, which have been shown to favour adaptation to the disease by promoting coping styles22 that are not based on denial, avoidance, fatalism and hopelessness, in the same way that happens to patients with other respiratory diseases such as IPF23 or COPD.24,25
Considering these results, early psychological interventions could have the benefit of reducing the impact of the disease on a psychological level and improving the quality of life of women with LAM. Analyzing the relationships between the psychological variables measured, it seems that aspects such as resilience serve as a protective factor against the appearance of psychological distress. Definitions of resilience are diverse and plentiful. Some researchers have described it as the ability to adapt positively to stressful circumstances,26 while others have defined resilience as being able to remain functionally stable and well despite ongoing stress.27 The American Psychological Society defines resilience as a process of ‘bouncing back’ from difficult experiences and ‘adapting well in the face of adversity, trauma, tragedy, threats or significant sources of stress’.28 Interventions that help develop resilience are based on to address resilience is to introduce the benefits of purpose in life; support individuals in identifying important sources of meaning (e.g. social relationships, work) as well as in setting priorities and guiding values for their life.29 Other interventions promote the understanding of external life challenges, personal beliefs and emotions, and encourage patients to reflect on personal (internal or external) resources and to use them more frequently.30 Psychoeducation on emotions is important, being useful mindfulness techniques and support patients in identifying pleasant activities to enhance positive emotions.31 Also interventions aimed at helping patients recognize their strengths and other sources of self-efficacy32,33 have been shown to be useful in improving resilience.
To achieve these objectives, there are different interventions that focus on psychological aspects. Interventions such as Cognitive-Behavioural Therapy (CBT) are a powerful approach for understanding the impact of our thoughts and beliefs on how we feel and act. CBT has proven useful in interventions with patients with respiratory diseases such as asthma,34 SARS-CoV-2 infection35 or COPD.36 The main problem with this type of intervention is that it requires trained clinical psychologists who should also be familiar with handling conditions such as LAM, sadly not frequent.
Other psychological interventions that may be useful are those aimed at improving resilience.37 Resilience-training programmes have been developed for, and conducted in a variety of clinical and non-clinical populations using various formats, such as multimedia programmes or face-to-face settings, and delivered in a group or individual context.38 These types of programmes have been developed by different health professionals such as nurses or social workers, so a psychologist is not a necessary condition.
Taking these aspects into account, it is necessary to first carry out a screening for possible alterations in the psychological sphere of women with LAM whenever they are diagnosed; As per the results of this study, the possible psychological reactions to the diagnosis may vary over time, so it is necessary to reassess them periodically. Questionnaires such as those used in this study (BDI, STAI...) can be useful, although other questionnaires such as the HADS can also be used due to its ease of administration and its widespread use in the field of health psychology.
The reality is that pulmonology services often do not have psychologists specialized in respiratory diseases, frequently resorting to Mental Health Units. Multidisciplinary teams in pulmonology departments (pulmonologists, nurses, physiotherapists, and even relatives) should be trained in emotional management through communication techniques such as counselling.
Strengths of our study include its size, novelty and internal consistency. However, a number of limitations deserve discussion. The main limitation of this study is that all participants are an opportunity sample from a national patient association, which may be a biased sample towards those coping with the disease, which is neither avoidant nor based on denial. On the other hand, as they were managed in different hospital settings, clinical variables such as FEV1, saturation, etc. were not collected, which does not allow us to know the relationship between the LAM severity, objective assessments and the psychological profile. Although oxygen therapy follow-up has been used as a criterion to identify patients with the worse clinical status, this is something inferred.
ConclusionThis study explores the psychological profile of women with a diagnosis of LAM, and how it influences coping with the disease. This is the first study of its kind to be carried out with a significant number of participants. The relationship of these psychological variables with other psychological constructs such as perceived social support and resilience demonstrates how important is the early detection of LAM and the later support to promote adaptation to the disease. There are interventions that allow us to help in this adaptation, and pulmonology multidisciplinary teams should have training in communication skills and empathy that might help them better meet the psychological needs of women with LAM.
FundingThis study is not funded.
Authors’ contributionsDavid Rudilla and Claudia Valenzuela have defined the study. Claudia Valenzuela has been responsible for requesting approval from the Ethics Committee. Together with David Rudilla and Claudia Valenzuela, María Molina and Álvaro Casanova defined the different study hypotheses. The statistical analyzes have been carried out by David Rudilla, and both the discussion of the results and the conclusions have been the result of a discussion process in which all participants have contributed equally.
Conflicts of interestThe authors declare to have no conflict of interest directly or indirectly related to the manuscript contents.
The authors would like to thank all the women of the Spanish Association of LAM (AELAM) who have so actively and generously agreed to participate in this study.