Low adherence to the pharmacological treatment in chronic diseases is a well-known clinical problem. The adherence rates in asthma and chronic obstructive pulmonary disease (COPD) have been shown to vary widely from 22% to 78%.1 Non-adherence to inhalers is associated with poorer control of disease and higher costs.1 However, improving adherence to treatment in chronic diseases is a complex objective as it is influenced by multiple factors.2–4
Patients’ beliefs about medications have been shown to influence adherence to treatments and could be a potentially modifiable factor for improving adherence.5 Across studies in patients with long-term conditions, higher adherence was associated with stronger perceptions of necessity and fewer concerns about treatment.6 However, in patients with asthma and COPD, few studies have been conducted on the role of medication beliefs in adherence to inhaled therapy, mainly in primary care patients, and the results have sometimes been contradictory.4,7,8 Unlike other treatments for chronic diseases, inhalers have rapidly perceptible effects on patients’ symptoms that can influence the perception and use of these medications.
Validated and translated instruments for measuring patients’ beliefs about medicines are now available and may be applied to our patients.9,10 We considered it of interest to analyze the possible effects of the beliefs of patients with asthma and COPD attended in a specialized hospital service. The results could provide useful information for the design of action plans to improve adherence to inhalers.
This cross-sectional study was conducted on adult patients diagnosed with asthma or COPD, with at least one year of inhaler use, in the Respiratory department of a university teaching hospital. The study was approved by the local Ethics Committee and patients were included after obtaining informed consent.
Adherence to inhalers was determined by two methods, one subjective (Test of the Adherence to Inhalers, TAI)11 and the other objective, with data from the electronic medical record (electronic prescription refill rate, PRR). According to the literature, good adherence was considered when the TAI (questions 1–10) reached 50 points and when the PRR was ≥80%.12 Patients’ beliefs about medicines were assessed with two questionnaires: the Spanish versions of the Beliefs about Medicines questionnaire (BMQ)9 and the Perceived Sensitivity to Medicines scale (PSM).10 BMQ includes differentiate scores on general medication (BMQ general, scores 8–40) and BMQ specific to a particular drug (inhalers in this case). The specific score is divided into two subcategories: necessity of use of inhalers and concerns of use (score 5–25 each). The PSM is a scale that assesses the patient's perception of being very sensitive to the effects of medications (scores 5–25, the higher the score, the greater the perception of sensitivity).
In the statistical analysis, comparisons between categorical groups were conducted using Pearson's chi-square test. For continuous variables, comparisons were made with the Mann–Whitney U test. Cohen's kappa statistic was employed to evaluate agreement. Spearman's correlation coefficient (rho) was used to quantify the correlation between the TAI and the PRR with the results of the different questionnaires. Statistical analysis was performed using the R package (http://www.R-project.org/).
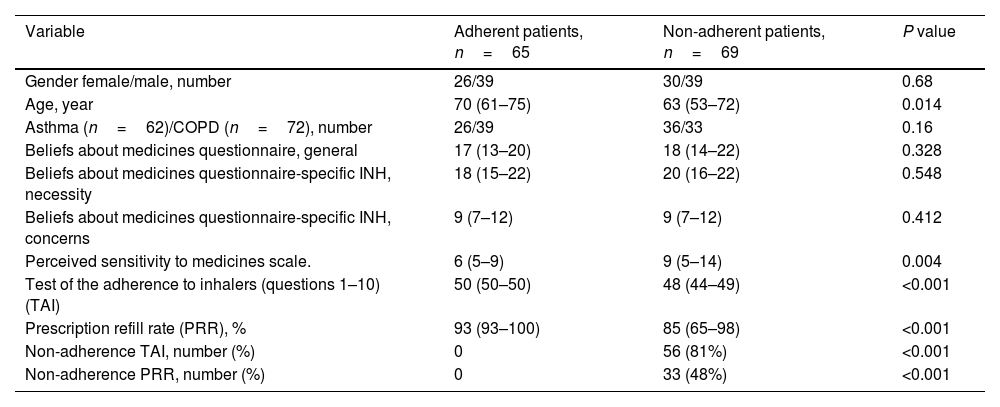
A total of 134 patients were included, 62 with asthma and 72 with COPD. The characteristics of the patients and the results of the questionnaires (adherent vs non-adherent patients according to the combination of subjective an objective measure) are detailed in Table 1.
Patient characteristics according to adherence.
| Variable | Adherent patients, n=65 | Non-adherent patients, n=69 | P value |
|---|---|---|---|
| Gender female/male, number | 26/39 | 30/39 | 0.68 |
| Age, year | 70 (61–75) | 63 (53–72) | 0.014 |
| Asthma (n=62)/COPD (n=72), number | 26/39 | 36/33 | 0.16 |
| Beliefs about medicines questionnaire, general | 17 (13–20) | 18 (14–22) | 0.328 |
| Beliefs about medicines questionnaire-specific INH, necessity | 18 (15–22) | 20 (16–22) | 0.548 |
| Beliefs about medicines questionnaire-specific INH, concerns | 9 (7–12) | 9 (7–12) | 0.412 |
| Perceived sensitivity to medicines scale. | 6 (5–9) | 9 (5–14) | 0.004 |
| Test of the adherence to inhalers (questions 1–10) (TAI) | 50 (50–50) | 48 (44–49) | <0.001 |
| Prescription refill rate (PRR), % | 93 (93–100) | 85 (65–98) | <0.001 |
| Non-adherence TAI, number (%) | 0 | 56 (81%) | <0.001 |
| Non-adherence PRR, number (%) | 0 | 33 (48%) | <0.001 |
Values are median (interquartile range) unless otherwise indicated. INH: inhalers; COPD: chronic obstructive pulmonary disease.
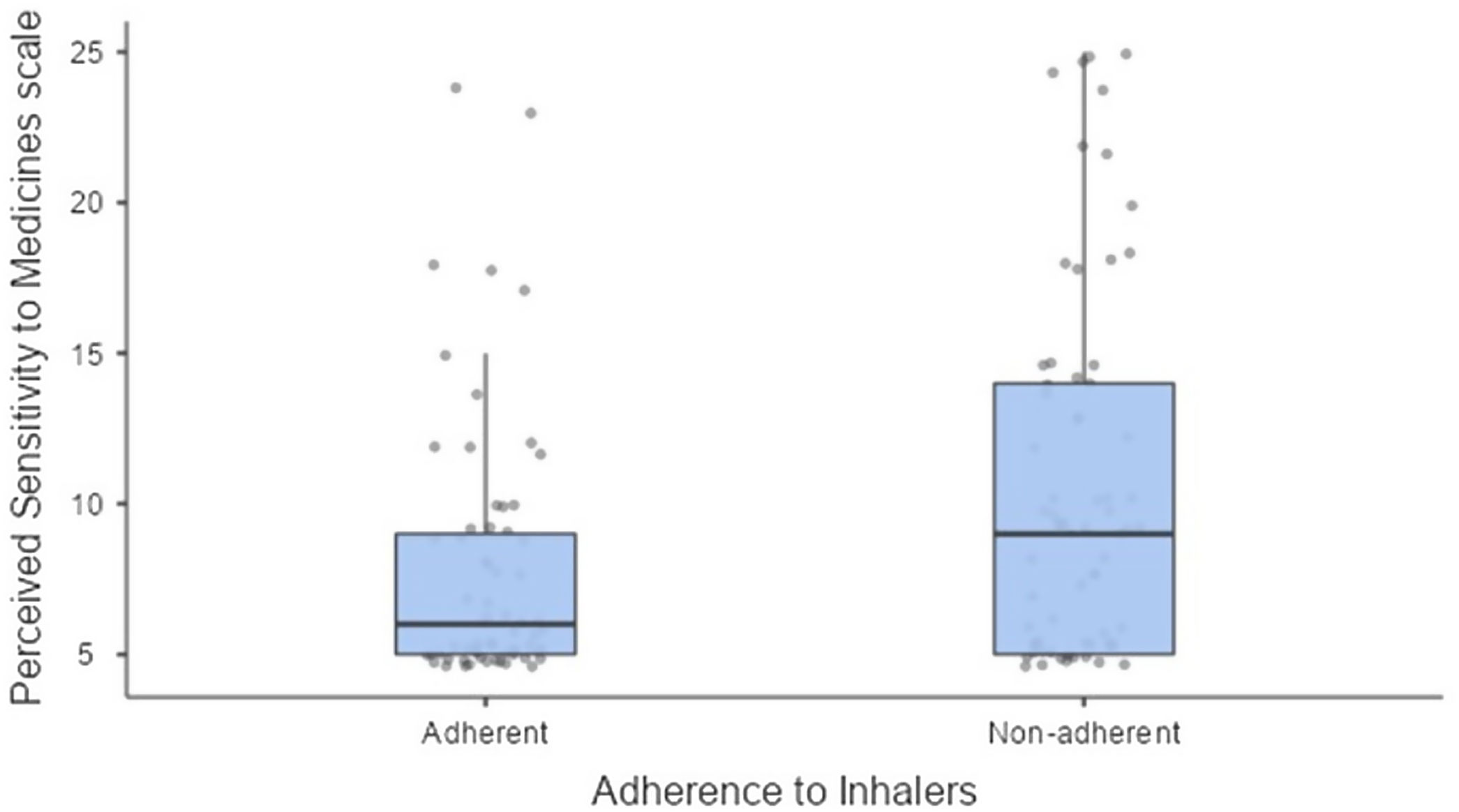
Non-adherence by TAI was observed in 56 out of 134 patients (42%), by PRR in 33 (25%), and by either of the two methods in 69 (51%). The agreement between TAI and PRR was 63% of individuals with a Kappa statistic of 0.20. Among the questionnaires used for evaluating patients’ beliefs (BMQ general, BMQ specific for necessity of inhalers, BMQ specific for concerns of inhalers, and PSM), only the differences in the PSM results were significant (Fig. 1). The best correlations between the results of questionnaires and values of subjective and objective methods of measurement were as follows: PSM and TAI (1–10), rho=−0.16 (p=0.06), and PSM with PRR, rho=−0.18 (p=0.036). Other correlations showed poorer values (p>0.07).
Our results reveal a low therapeutic adherence among patients using inhalers, even though they are receiving care in a specialized hospital setting. Among patients with asthma, 58% were non-adherent, and 46% of patients diagnosed with COPD showed non-adherence. This finding is alarming, especially considering that these individuals are being treated in a specialized center, where presumably more resources are available for patient education and motivation. A higher lack of adherence in patients with asthma compared to those with COPD has been previously described and attributed to sociodemographic characteristics,13 although in our series the difference was not significant.
Subjective or objective measures can be used to analyze therapeutic nonadherence. It has been demonstrated that their information is complementary, making it advisable to use both simultaneously.12 This criterion was applied in this study. As previously described, there is low agreement between subjective and objective measures of nonadherence.12 In our series, the Kappa statistic was only 0.20.
In this study, adherence to inhalers in patients with asthma and COPD is associated with perceived sensitivity to medicines, but not significantly related with other characteristics of the beliefs about medicines questionnaires. This finding differs from descriptions in other chronic diseases. In the general population, the results of both the BMQ questionnaire and the PSM scale were associated with medication use patterns.5 In other chronic conditions, such as stroke, diabetes mellitus, or rheumatoid arthritis, results of the BMQ questionnaire, in addition to PSM, were also associated with adherence to medications.6,14.15 Few studies have evaluated the beliefs about medicines in patients treated with inhalers, and there is significant variability in its association to adherence.4,7,8
The finding that the BMQ questionnaire does not correlate with adherence to inhalers may be attributed to the fact that these drugs have a rapidly detectable symptomatic effect on the patient, unlike other chronic treatments. This effect on symptoms may modulate the influence of beliefs about medicines on drug use. Perceived oversensitivity to medications (in a generic way) has been shown to be associated with reduced adherence to inhalers. This data may help identify patients who require additional measures to improve adherence using the PSM questionnaire. However, the influence of perceived sensitivity on therapeutic adherence is relatively modest, and any corrective measures must include multiple other educational and clinical aspects.
Our results indicate, firstly, a high level of therapeutic nonadherence to inhalers in patients with asthma and COPD attended in a specialized hospital service. Secondly, we confirm the need to use different methods simultaneously to detect nonadherence to medications. Thirdly, and importantly, the perception of oversensitivity to medications has more influence on adherence to inhalers than other aspects of knowledge, such as the belief of the need or risk of their use.
While non-adherence is influenced by multiple factors, these results underscore the importance of addressing patients’ perceived sensitivity to medicines when developing interventions to improve medication adherence.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributionsEGP: Conceptualization, Methodology, Data curation, Formal analysis, Writing-original draft.
JGD, CBM, LZM, MGN: Methodology, Data collection, Formal analysis, Writing-review and editing.
MBV: Conceptualization, Methodology, Formal analysis, Writing-original draft.
All authors have read and provided intellectual input to the manuscript.
All authors have approved the final version of the manuscript and take public responsibility of its content.
Conflicts of interestThe authors state that they have no conflict of interests.