Community-acquired methicillin-resistant Staphylococcus aureus is the first cause of skin and soft tissue infections, but can also produce severe diseases such as bacteremia, osteomyelitis and necrotizing pneumonia. Some S. aureus lineages have been described in cases of necrotizing pneumonia worldwide, usually in young, previously healthy patients. In this work, we describe a fatal case of necrotizing pneumonia due to community-acquired methicillin-resistant S. aureus clone ST30-SCCmecIVc-spat019-PVL positive in an immunocompetent adult patient.
Staphylococcus aureus resistente a meticilina adquirido en la comunidad es la primera causa de infecciones de piel y partes blandas, aunque también puede producir infecciones graves, como bacteriemia, osteomielitis y neumonía necrotizante. Algunos linajes de S. aureus se han asociado a casos de neumonía necrotizante en el mundo, generalmente en pacientes jóvenes previamente sanos. En este trabajo comunicamos un caso fatal de neumonía necrotizante causado por el clon de S. aureus resistente a meticilina adquirido en la comunidad ST30-SCCmecIVc-spat019-LPV positivo, en un paciente adulto inmunocompetente.
Most commonly, community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) produces skin and soft-tissue infections while severe and life-threatening infections such as meningitis, necrotizing pneumonia, and severe sepsis are rare. CA-MRSA strains are globally spread; however, the prevalence and clonal distribution is dynamic.
Unlike hospital-acquired MRSA (HA-MRSA), CA-MRSA strains usually carry SCCmec type IV, produce Panton-Valentine leukocidin (PVL) and show susceptibility to several non-ß-lactam antibiotics13.
Necrotizing pneumonia (NP) is a severe form of lung disease associated with the formation of abscesses and cavitation within the lung parenchyma. This syndrome is characterized by respiratory insufficiency and rapid development of septic shock, in the context of fever, hemoptysis, leukopenia, multilobar necrosis, cavitary lesions and pleural effusion, and it is associated with a high mortality rate14.
Among the several virulence factors related to CA-MRSA, Panton-Valentine leukocidin is a bicomponent toxin that kills leukocytes by creating pores in the cell membrane. Some authors have associated the presence of this toxin with the development of severe necrotizing pneumonia5.
In the present work we describe a case of necrotizing pneumonia with rapid progression to death due to community-acquired methicillin-resistant S. aureus in an immunocompetent male patient.
On February 2nd, 2013, a 50-year-old male patient presented to the hospital emergency room with severe headache, bronchospasm and malaise. He had a history of hypertension treated with enalapril and was overweight. He was then treated with diclofenac, developing generalized urticaria.
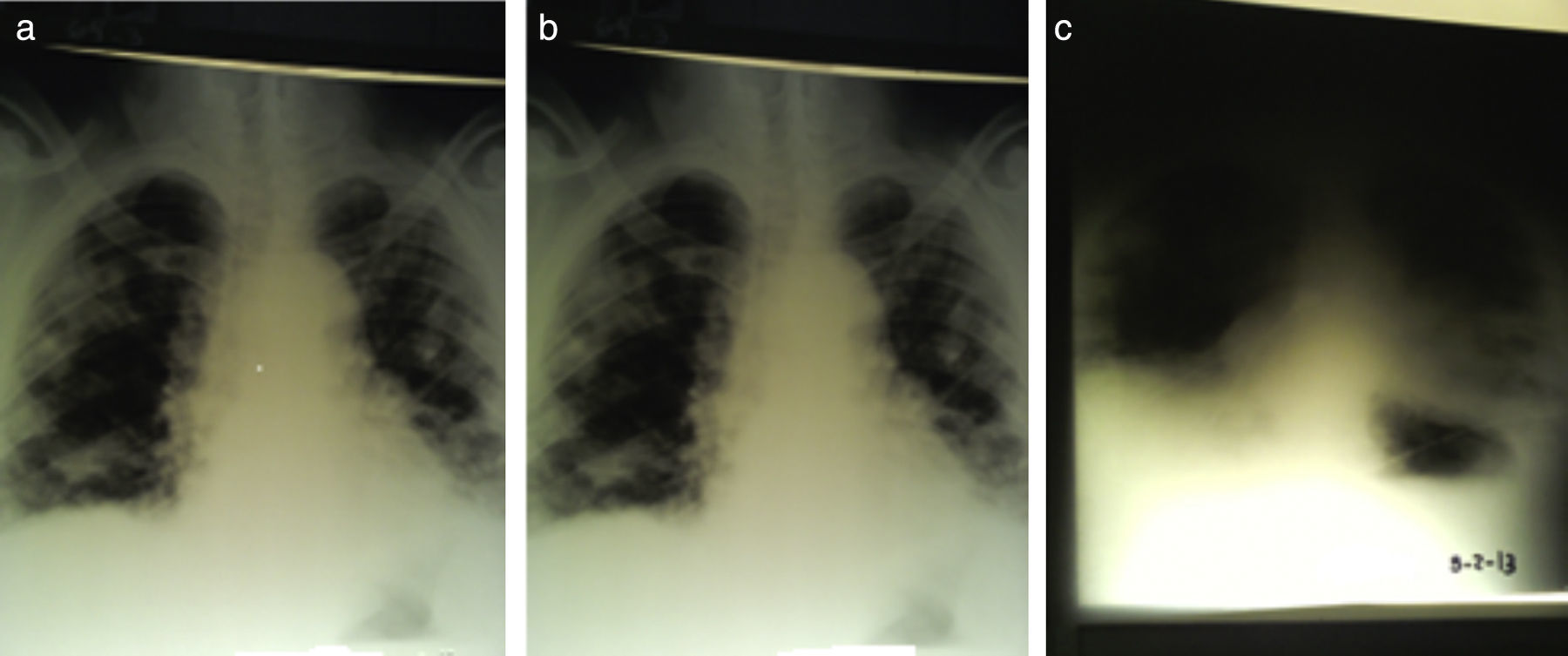
The following day he was admitted to hospital presenting severe bronchospasm and fever. At 12.00 pm, a mild bilateral diffuse infiltrate in the middle and lower lung fields was found on a chest X-ray.
On admission, laboratory tests revealed a leukocyte count of 6300/mm3, hematocrit 53%, blood glucose 218mg/dl, urea nitrogen 91mg/dl and creatinine 2.47mg/dl. It was interpreted as a respiratory sepsis and ceftriaxone and clarithromycin were empirically administered.
In the following hours his condition deteriorated rapidly. At 5.00 pm the patient was admitted to intensive care unit due to clinical worsening and an impairment in ventilatory function. He presented dyspnea grade 3, hypoventilation, fever and normal blood pressure. A new chest X-ray revealed severe bilateral smooth infiltrates in both lungs.
Blood and urine cultures were performed, and blood tests showed leukocyte count 3400/mm3, urea nitrogen 127mg/dl, creatinine 4.33mg/dl, pH: 7.195, pCO2 42.7mmHg, pO2 85.7mmHg, CO3H− 16.2mEq/l and % SatO2 93.6. The Gram stain of blood specimens showed gram-positive cocci in clusters.
The patient exhibited a minimal scrotal lesion, and referred for a bilateral scrotal inflammation for the last three days that was not evidenced at the time of admission.
At 9.00 pm bilateral patched infiltrates in both lungs (necrotizing pneumonia) compatible with staphylococcal infection were observed in a new chest X-ray, whereby a treatment with vancomycin, piperacillin/tazobactam and clarithromycin was established. Serial chest radiographs are presented in Fig. 1.
On February 4th at 1.00 am, the patient remained febrile, oliguric and required mechanical ventilation. Laboratory results at 7.00 am were: leukocyte count 2000/mm3, pH 6.980, pCO2 62.0mmHg, pO2 27.8mmHg, CO3H− 14.2mEq/l, % SatO2 24.7. At 7.40 am, the patient died.
Methicillin-resistant S. aureus (MRSA) grew from the blood culture. The strain was tested for antimicrobial susceptibility by disk diffusion according to CLSI guidelines, and showed resistance to oxacillin and cefoxitin, and susceptibility to erythromycin, clindamycin, rifampicin, minocycline, trimethoprim/sulfamethoxazole, gentamicin and ciprofloxacin. Vancomycin MIC value determined by Etest was 1μg/ml.
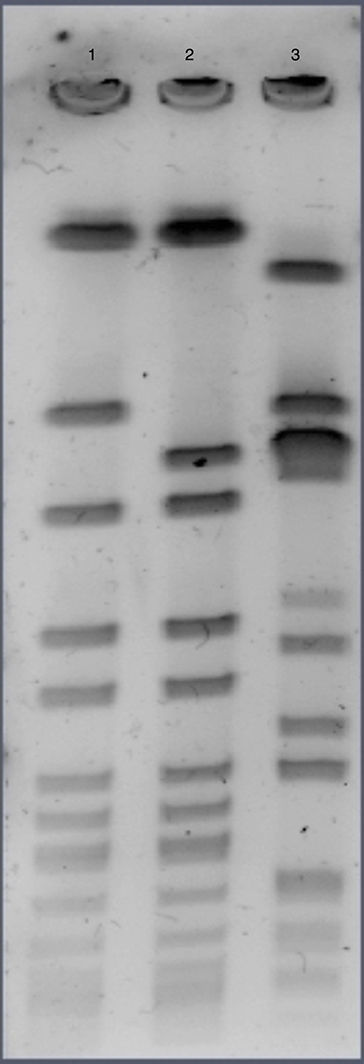
Methicillin resistance was confirmed through the amplification of the mecA gene by the polymerase chain reaction (PCR). Detection of lukS/F-PV (PVL coding genes) and SCCmec typing were done by PCR and the strain was genotyped by pulsed field gel electrophoresis (PFGE), multilocus sequence typing (MLST) and spa typing. MRSA was classified as PFGE type C, sequence type 30, spa type 019, lukS/F-PV positive and carried SCCmecIVc. PFGE photograph is shown in Fig. 2.
Several cases of necrotizing pneumonia due to S. aureus have been described in different countries. Even though it is a rare complication of lung disease, it is known to be aggressive and associated with rapid progression to death.
The strain recovered in blood specimens presented a typical community-acquired phenotype as it was susceptible to most non-beta lactam antibiotics, carried SCCmecIV and PVL coding genes, confirming that CA-MRSA strains are capable of causing severe diseases in immunocompetent patients. Given the low frequency of NP cases, it could also be hypothesized that some specific host characteristics could be necessary to develop this serious infection.
The prevalence of CA-MRSA clones varies geographically, with five globally predominant clones: ST1-IV (USA400), ST8-IV (USA300), ST30-IV (South West Pacific clone), ST59 (Taiwan clone), and ST80 (European clone). Nowadays ST 30 represents one of the most frequently isolated lineages among CA-MRSA strains, and is considered a pandemic clone as it has been isolated repeatedly from every continent9.
Clonal complex 30 is a successful S. aureus lineage, irrespective of its methicillin resistance. It has been associated with an increased risk of infective endocarditis10, increased hematogenous complications3 and persistent S. aureus bacteremia15. In Argentina, methicillin-sensitive S. aureus (MSSA) strains belonging to the ST30 lineage have also been recovered from cases of osteomyelitis in a study conducted by Lattar et al6.
Among the published data of necrotizing pneumonia due to CA-MRSA, different clones have been described, e.g. ST59-SCCmecIV-spat437-PVL positive, ST910-SCCmecIV-spat318, ST398-SCCmecV-spat034, ST1409-SCCmecIV-spat6531, ST8011, showing that there would not be a unique MRSA clone associated with this disease, and could correspond to the most prevalent CA-MRSA clone in each region. Furthermore, we might be missing information due to the lack of molecular typing of S. aureus strains in some previous descriptions of NP cases.
It is not known if certain clones have actually more ability to cause this disease. Here we show that CA-MRSA ST30-IVc-t019-PVL positive is also capable of causing community-acquired necrotizing pneumonia.
CA-MRSA ST30-IV belongs to clonal complex 30 (CC30) and is thought to have evolved from penicillin-resistant phage type 80/81 S. aureus, a clone that became pandemic throughout the 1950s and caused a high number of skin lesions, sepsis, and pneumonia in children and young adults in hospitals and the community12.
In Argentina, MRSA ST30-IVc-t019-PVL positive has been described as the most frequent clone in skin and soft tissues infections (SSTIs) and invasive diseases due to CA-MRSA in adolescent and adult patients, among isolates recovered from two multicenter studies that included 19 hospitals from Buenos Aires and Santa Fe provinces2,7. This clone had been previously detected as a minor clone in community-associated infections in the eastern and northeastern region of Argentina4, but nowadays it has replaced the previously prevalent MRSA ST5-IVa-t311-PVL positive clone in our region and is now apparently well adapted to the Argentinean community2,7.
The MRSA clone ST30-IVc-PVL positive was also responsible for the large outbreak in Uruguay in 2003 that involved more than 1000 patients and at least 12 deaths8.
Therefore, ST30 clone could have better advantages than other CA-MRSA clones for developing severe infections; however, this approach needs to be further investigated in detail.
Although community-acquired necrotizing pneumonia is often associated to bad prognosis and death, there is also evidence of good success of severe PVL positive S. aureus pneumonia cases11, and the authors attributed those results to a high suspicion of this pathogen in the differential diagnosis that could lead to a prompt initiation of an adequate antimicrobial therapy. Therefore, CA-MRSA should be considered in cases of rapid deterioration of lung disease.
The development of a serious infection in a young person without predisposing conditions is a typical feature of CA-MRSA infections. Although in the case presented in this work no microbiological culture was performed from the skin scrotal lesion, it might have represented the initial source of hematogenous spread of CA-MRSA. The rapid evolution and the fatal outcome of this case caused by the prevalent CA-MRSA clone must be considered as an indication of the invasiveness and virulence potential of ST30-SCCmec IVc clone.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflicts of interest.
FundingThis work was partially supported by Grants from UBACyT and ANPCyT to M. Mollerach. M. Mollerach is a member of Carrera del Investigador Científico (CONICET). Silvina Fernandez is a doctoral fellow of Universidad de Buenos Aires.