Syphilis has become a serious issue for human immunodeficiency virus (HIV)-infected patients worldwide in recent years; however, the studies related to HIV coinfection and syphilis reinfections in Istanbul, Turkey, are limited. Our objective was to determine the seroprevalence of syphilis among HIV-infected men in the city which has one of the highest HIV prevalence rates in Turkey. Two hundred and forty four (244) HIV-positive men were evaluated at Istanbul Medical Faculty, Department of Medical Microbiology from March to June 2018. Serum samples were screened for the presence of antibodies against Treponema pallidum using the chemiluminescent microparticle immunoassay (CMIA). Samples found to be positive were investigated with the rapid plasma reagin (RPR) test and the T. pallidum hemagglutination assay (TPHA). The patients completed a questionnaire for sociodemographic data. The mean age was found to be 41.8 years; 35.6% were men who have sex with men (MSM). The overall seroprevalence of syphilis among the patients was 19.3%. MSM had a significantly higher seroprevalence than heterosexual patients (28.7%). In Turkey, there is a high seroprevalence of syphilis in HIV-infected patients, MSM being the most affected group. Therefore, HIV-infected patients should be screened for syphilis at least annually and should be informed about sexually transmitted diseases (STDs).
En los últimos años, la sífilis se ha convertido en un problema grave para los pacientes infectados por el virus de la inmunodeficiencia humana (HIV) en todo el mundo; sin embargo, los estudios relacionados con la coinfección por HIV y las reinfecciones por sífilis en Estambul, Turquía, son limitados. Nuestro objetivo fue determinar la seroprevalencia de la sífilis entre los hombres infectados por el HIV en Estambul, ciudad con las tasas de prevalencia del HIV más altas de Turquía. Se evaluaron 244 hombres con HIV entre marzo y junio de 2018 en la Facultad de Medicina de Estambul, Departamento de Microbiología Médica. Las muestras de suero se analizaron para detectar la presencia de anticuerpos contra Treponema pallidum con un inmunoensayo de micropartículas quimioluminiscentes (CMIA). Las muestras que resultaron positivas en dicha prueba se investigaron con la prueba de reagina plasmática rápida (RPR) y el ensayo de hemoaglutinación T. pallidum (TPHA). Los pacientes completaron un cuestionario de datos sociodemográficos. La media de la edad fue de 41,8 años; 35,6% eran hombres que tienen sexo con hombres (HSH). La seroprevalencia global de sífilis entre los pacientes fue del 19,3%. Los HSH tuvieron una seroprevalencia significativamente mayor que los pacientes heterosexuales (28,7%). En Turquía, existe una alta seroprevalencia de la sífilis en pacientes infectados por el HIV y los HSH son el grupo más afectado. Por lo tanto, los pacientes infectados por el HIV deben someterse a la detección de sífilis al menos una vez al año y deben ser informados sobre las enfermedades de transmisión sexual (ETS).
Sexually transmitted diseases (STDs) are a growing public health concern all over the world. Serious complications can arise unless early diagnosis and treatment of STDs are performed8. International guidelines, which are also valid in Turkey recommend that human immunodeficiency virus (HIV)-infected individuals in particular should be routinely screened for STDs at least once a year and even more frequently in the case of high-risk individuals18.
In particular, venereal syphilis still remains a worldwide public health problem. Around 5.6 million people are newly infected every year20. Furthermore, recent reports show that the frequency of syphilis is increasing especially among HIV-positive patients in many countries3,22. To make matters worse, syphilis associated with ulcerations cause damage to epithelial and mucosal barriers, facilitating the transmission of HIV virions. Proinflammatory components of the bacterial pathogen have been shown to stimulate the expression of CCR5 (HIV co-receptor) on human monocytes within chancres, thereby increasing the susceptibility of human monocytes to HIV infection24. Certain sexual behaviors that put people at an elevated risk of acquiring STD also increase their risk of acquiring HIV. Local epidemiological studies strongly implicate that STD/HIV infection rates are especially high among men who have sex with men (MSM)7. Early syphilis was detected in 4.6% and past syphilis in 44.5% of the HIV+MSM14. Untreated infections can lead to a variety of life-threatening complications following a long asymptomatic latent stage26. Studies reveal that individuals suffering from syphilis show a 2 to 9-fold increased risk of HIV infection15. Interestingly, HIV infections also significantly increase the risk of primary as well as secondary syphilis. In this context, monitoring HIV-positive patients, especially MSM, for syphilis is of vital importance for the development of appropriate intervention strategies11. Further investigations of syphilis in HIV-positive patients will certainly help to characterize infection patterns, which will greatly aid in developing the aforementioned intervention measures in case of the presence of a co-infection. Determining the rate of syphilis is important in improving the awareness of the real threat of acquiring both HIV and syphilis. Most intriguingly, previous studies showed that syphilis seropositivity is higher in HIV-positive males than in HIV-positive females28. Therefore, considering the limited number of studies performed in our country, this study was conducted in a patient group consisting exclusively of HIV-positive male individuals. The total number of HIV-positive patients has increased by more than 2-fold from December 2011 to June 201612,16. However, there are indications highly suggesting that the real number of HIV/AIDS cases in Turkey is actually ten times higher than the officially reported number of cases17. Although there are studies on syphilis with various patient groups2,21, there are only very limited data on syphilis prevalence in HIV-infected men in Turkey4. In this study, the main objectives were to estimate syphilis prevalence and to determine the risk factors among HIV-infected men in the most crowded city of Turkey.
Materials and methodsA cross-sectional study was designed from 244 HIV-infected men at the Istanbul University School of Medicine, Istanbul in 2018. Plasma samples of 84 treatment-naive and 160 treatment-experienced HIV-infected men were used in our study to determine serological prevalence of syphilis.
SamplingVenous blood samples (10ml) were collected from all patients; 5 ml in an EDTA coated tube for HIV-1 RNA and 5ml in an EDTA coated tube for flow-cytometer and 5ml in a simple blood collection tube for syphilis tests. Blood samples were separated by centrifugation at 1600×g for about 20min and divided into aliquots for the determination of HIV-1 RNA and treponemal antibodies.
Syphilis detectionPatients were tested for specific treponemal antibodies with a chemiluminescent microparticle immunoassay (CMIA) (ARCHITECT Syphilis TP™; Abbott, Wiesbaden, Germany). The ARCHITECT Syphilis TP™ assay is a qualitative test for the detection of antibodies (IgG and IgM) directed against Treponema pallidum (Tp) to aid in the diagnosis of syphilis infection. It uses three recombinant antigens (Tp15, Tp17, and Tp47) on microparticle for improved syphilis detection.
Reverse algorithm was used in the diagnosis of syphilis in our study, because it can decrease the number of false positives resulting in improved a specificity and is also more sensitive than the traditional algorithm for detecting cases of primary and latent syphilis infections. Samples found to be positive with the CMIA test were investigated by non-specific treponemal tests using the rapid plasma reagin (RPR) test (Spinreact SA, Girona, Spain) and the T. pallidum hemagglutination assay (TPHA) (Spinreact SA, Girona, Spain).
HIV-1 RNA (viral load) by real-time PCRViral load detection was performed on an artus™ HI Virus-1 kit by QIAsymphony SP/AS and Rotor-Gene Q (QS-RGQ system)(Hilden, Germany). The artus™ HI Virus-1 RG RT-PCR kit is an in vitro nucleic acid amplification test for the quantitation of HIV type 1 (HIV-1) RNA in human plasma. This diagnostic test kit utilizes the reverse transcription polymerase chain reaction (RT-PCR) and is configured to be used with Rotor-Gene Q Instruments. The test can quantitate HIV-1 RNA over the range of 120–1×108HIV-1IU/ml. The HI Virus-1 RG Master A and B contain reagents and enzymes for the reverse transcription and specific amplification of a 93bp region of the HIV-1 genome, and for the direct detection of the specific amplicon in fluorescence channel Cycling Green of the Rotor-Gene Q.
Flow cytometryA T-cell subset was analyzed by a four color multi-test CD3 (FITC)/CD4 (APC)/CD8 (PE)/CD45 (PerCP). The antibodies were procured from BD Biosciences. Samples were obtained on a flow cytometer (Navios, Beckman Coulter, USA) and data were analyzed using the Kaluza flow analysis software (Beckman Coulter, USA).
Ethical approvalThe study was approved by the Ethical committee of the Faculty of Medicine at Istanbul University (reference number: 2017/1181). Informed consents were obtained from all participants. Data were collected through personal interviews with participants taking into consideration data confidentiality. All procedures performed in this study were in accordance with the ethical standards of the Declaration of Helsinki.
Statistical analysisDemographical data of patients presenting seroreactivity were obtained. Statistical analyses were performed in SPSS 23.0 (IBM Corp, Armonk, NY). All statistical tests were 2-tailed and a p value of less than 0.05 was considered statistically significant.
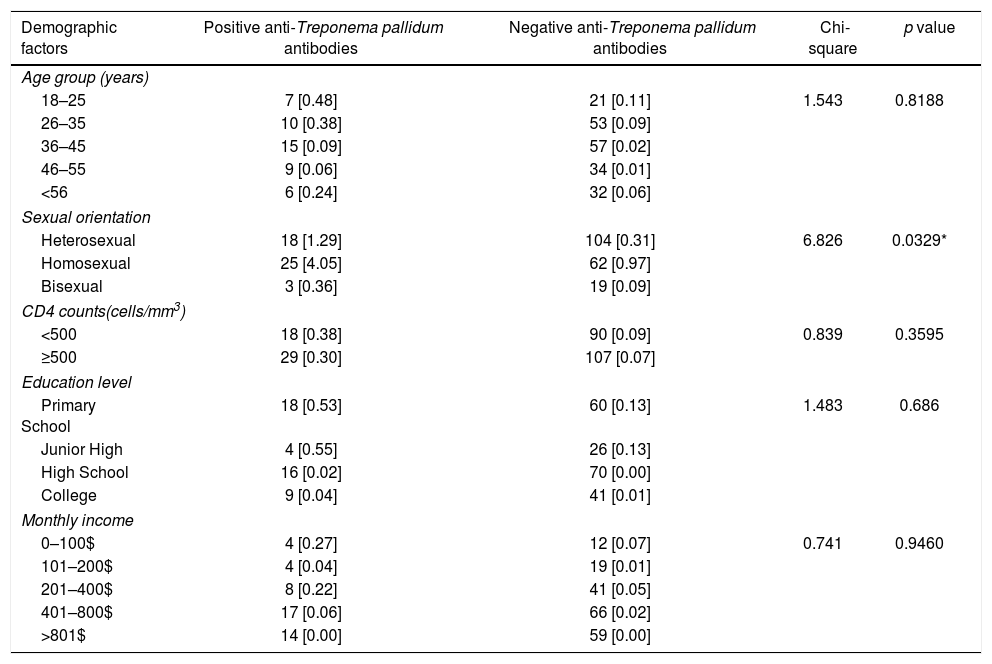
ResultsA total of 244 HIV-infected patients was included in the study between March 2018 and June 2018. Demographical data of the study population are shown in Table 1. No significant difference was detected between the antiretroviral treatment (ART) received (17.8%) and ART-naive patients (22.6%). The ages of the individuals participating in the study ranged from 18 to 71 years old and the mean age was calculated to be 41.8; 35.6% of patients were homosexual, 9% bisexual, 50% heterosexual and 5.3% did not reveal their sexual orientation. The median CD4 cell count was determined to be 565cells/ml and the median viral load was 4.7 log10 copies/ml.
Demographic information about the study population.
| Demographic factors | Positive anti-Treponema pallidum antibodies | Negative anti-Treponema pallidum antibodies | Chi-square | p value |
|---|---|---|---|---|
| Age group (years) | ||||
| 18–25 | 7 [0.48] | 21 [0.11] | 1.543 | 0.8188 |
| 26–35 | 10 [0.38] | 53 [0.09] | ||
| 36–45 | 15 [0.09] | 57 [0.02] | ||
| 46–55 | 9 [0.06] | 34 [0.01] | ||
| <56 | 6 [0.24] | 32 [0.06] | ||
| Sexual orientation | ||||
| Heterosexual | 18 [1.29] | 104 [0.31] | 6.826 | 0.0329* |
| Homosexual | 25 [4.05] | 62 [0.97] | ||
| Bisexual | 3 [0.36] | 19 [0.09] | ||
| CD4 counts(cells/mm3) | ||||
| <500 | 18 [0.38] | 90 [0.09] | 0.839 | 0.3595 |
| ≥500 | 29 [0.30] | 107 [0.07] | ||
| Education level | ||||
| Primary School | 18 [0.53] | 60 [0.13] | 1.483 | 0.686 |
| Junior High | 4 [0.55] | 26 [0.13] | ||
| High School | 16 [0.02] | 70 [0.00] | ||
| College | 9 [0.04] | 41 [0.01] | ||
| Monthly income | ||||
| 0–100$ | 4 [0.27] | 12 [0.07] | 0.741 | 0.9460 |
| 101–200$ | 4 [0.04] | 19 [0.01] | ||
| 201–400$ | 8 [0.22] | 41 [0.05] | ||
| 401–800$ | 17 [0.06] | 66 [0.02] | ||
| >801$ | 14 [0.00] | 59 [0.00] | ||
Forty-seven (19.3%) patients were found to be seropositive. However, syphilis seropositivity was not significantly associated with age, CD4 cell counts, educational level or monthly income, respectively (p=0.818, 0.359, 0.827, 0.946). Seropositivity was determined to be elevated in the MSM group (28.7%) compared to heterosexual HIV-infected individuals (14.7%) (p<0.05). When the RPR titers of 47 patients were examined, 16 were positive at 1 to 1/2 titer,12 were positive at 1/4 to 1/8, 12 were positive at 1/16 to 1/32, 5 were positive at 1/64 to 1/128 and 2 were positive at 1/256 and higher. Eighteen (38.3%) patients were determined to have a coinfection with HIV and syphilis. Seventeen (36.1%) patients had negative RPR results after the HIV diagnosis date and 8 (17.1%) had a syphilis history before the HIV diagnosis. The syphilis history of 4 patients could not be obtained. Clinically evaluated cases with treponemal diagnoses were treated. Primary, secondary, and early latent syphilis cases were treated with 2.4 million units of penicillin G benzathine intramuscularly, whereas late latent syphilis cases were treated with a total of 7.2 million units of penicillin G benzathine administered every 3 weeks intramuscularly. Doxycycline or azithromycin, which are recommended as alternative treatment, were preferred for those patients reporting a previous history of penicillin allergy. Three patients reported penicillin allergy. Therefore, doxycycline was started in two out of three patients and azithromycin in one patient.
DiscussionSyphilis is not only a frequently detected sexually transmitted disease in developing countries but also has an increasing importance for HIV infected individuals as it leads to severe progression. Hence, the early diagnosis of syphilis is of paramount importance for HIV-infected patients. Interestingly, HIV infection incidence has been decreasing recently in Western and Central Europe, America and all over the world except Eastern Europe and Asia13. On the other hand, the incidence of STDs such as syphilis has been increasing in Europe and the USA1,27.
According to the United States Centers for Disease Control and Prevention (CDC), more than half of the homosexual males with primary and secondary syphilis have been infected with HIV1. Regretfully, there is no clear information on this issue for our country5. The international guidelines that are also followed in Turkey, recommend the follow-up of HIV-positive patients for STDs, including syphilis, gonorrhea, chlamydia (urethritis and LGV), HPV, HBV and HCV27. Women were not included in this study for the reason that the prevalence of syphilis in females was shown to be much lower than that of men in a previous study carried out in Turkey4. Moreover, the number of HIV-infected men in Turkey has grown faster than that of women12. Higher rates of seroprevalence detected in our study compared to neighboring countries may be due to differences in the route of transmission in these countries5. Furthermore, syphilis seropositivity was found to have increased in the population between 36–45 years of age and seroprevalence among 18–35 year-old-patients was lower than that of older patients. The low rate of seropositivity among individuals in this group despite being the most sexually active sub-population may be the result of their higher awareness of STDs.
The frequency of syphilis among people infected with HIV determined in this study was found to be in accordance with other studies carried out with the same study design in different parts of the world, reflecting the increasing incidence of syphilis infection in people infected with HIV10,25. In our study, the rate of syphilis was found to be significantly higher in MSM HIV-infected patients (28.7%). This finding is in accordance with other studies conducted among the MSM subpopulation in other countries throughout Europe and the US1,6. A higher frequency of risky sexual behaviors that increase the risk of acquiring STDs, such as sexual relationships with multiple partners and hypersexuality, may be the reason for the high prevalence of syphilis in this group. Syphilis antibodies were detected in patients from CMIA who had no symptoms or a history of infection and whose RPR titers were weak positive. The majority of patients with positive TPHA test and low RPR titers were patients treated by other hospitals. Consumption of antibiotics such as ceftriaxone and azithromycin, for other medical health conditions, may be the reason for low syphilis titers19,23. It is well known that syphilis may heal spontaneously. Hence, another reason for low RPR titers detected in some patients may be that these patients have healed spontaneously9.
This study, in parallel with other studies carried out in different parts of the world, shows the high frequency of syphilis among HIV-infected patients in Turkey. Findings of the study highlight the fact that patients infected with HIV must be screened for syphilis at least annually and must be informed about STDs. In conclusion, the implementation of protective measures for risky populations is a critical step in the prevention of both HIV and syphilis.
ConclusionsThe high prevalence of syphilis observed in HIV-infected males requires the implementation of urgent measures to prevent infection in this patient group. Screening of HIV-infected individuals for syphilis will have clinical and epidemiological significance for the management of infected patients. The results of this study will assist public health authorities in their ongoing effort to control the syphilis epidemic spreading among HIV patients in Turkey more efficiently.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
Authors’ contributionsMOK, HE and AA designed the study.
MOK, OE, SB and HE collected the data.
MOK, HB, SÇ and FK performed the tests.
MOK, BA wrote the draft manuscript.
MOK, BA, HE and AA contributed to the writing of the manuscript.
Conflict of interestThe authors declare that they have no conflicts of interest.