To investigate the relationship between platelet activation parameters that are involved in the vascular response, the atherothrombotic process, and erectile function, in which epithelial dysfunction plays a significant role.
Materials and methodsA study was performed on patients who had a color Doppler ultrasound (CDUS) of the penis due to erectile dysfunction. The patients were divided into two groups: those with normal CDUS findings, and those with vascular dysfunction on CDUS. Patients were also divided into two groups according to their scores using the International Index of Erectile Function (IIEF). The relationships between platelet activation factors, vascular parameters, and severity of the disorder were analyzed.
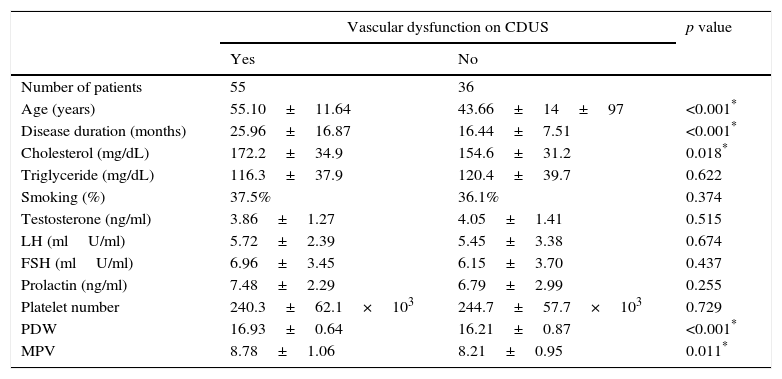
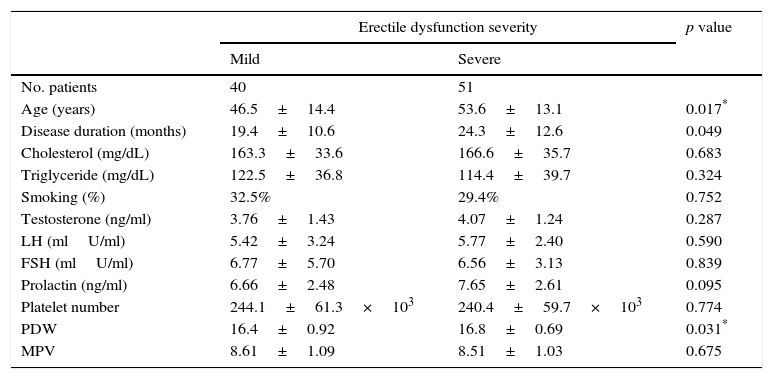
ResultsA total of 91 patients who fulfilled the inclusion criteria were included in the study. CDUS showed vascular dysfunction in 55 patients (Group I), while the findings were normal in 36 patients (Group II). Age, cholesterol level, disease duration, mean platelet volume (MPV), and platelet distribution width (PDW) were compared between Groups I and II, with Group I showing significantly higher values. The parameters that could affect Doppler ultrasound results were analyzed using multivariate regression analysis. This showed that PDW and disease duration were independent prognostic factors (p=.021 and p=.005, respectively). When the patients were divided into two groups according to their IIEF scores, in those with mild (Group A) and severe disease (Group B), it was found that there were significant differences between the groups with age, disease duration, and PDW, while two groups were found similar in terms of MPV, cholesterol levels, and hormone parameters.
ConclusionIt is supposed that increased platelet activation parameters, and PDW in particular, give important information for disease progression and follow-up of vascular dysfunction in erectile dysfunction.
Investigar la relación entre los parámetros de activación de plaquetas involucrados en la respuesta vascular, el proceso aterotrombótico y la función eréctil, en la que la disfunción endotelial desempeña un papel importante.
Material y métodosSe analizaron los pacientes en los que se realizó una ecografía Doppler color (EDC) del pene por disfunción eréctil. Los pacientes fueron divididos en 2 grupos: con resultados normales en la EDC y con disfunción vascular en la EDC. Los pacientes fueron asimismo divididos en 2 grupos en función de las puntuaciones del Índice Internacional de Función Eréctil (IIFE). Se analizaron las relaciones entre los factores de activación plaquetaria, los parámetros vasculares y la gravedad del trastorno.
ResultadosUn total de 91 pacientes que cumplieron los criterios de inclusión fueron incluidos en el estudio. La EDC mostró disfunción vascular en 55 pacientes (grupoi), mientras que los resultados fueron normales en 36 pacientes (grupoii). La edad, el nivel de colesterol, la duración de la enfermedad, el volumen medio de plaquetas (VMP) y la anchura de distribución de las plaquetas (ADP) se compararon entre los gruposi y ii; además, los valores fueron expresivamente más altos en el grupoi. Los parámetros que podrían afectar los resultados de la EDC se valoraron con el análisis de regresión multivariante, lo que demostró que la ADP y la duración de la enfermedad fueron factores pronósticos independientes (p=0,021 y p=0,005, respectivamente). Cuando los pacientes fueron divididos en 2 grupos en función de las puntuaciones IIFE, en aquellos con enfermedad leve (grupo A) y enfermedad grave (grupo B) se encontraron diferencias significativas entre los grupos con la edad, la duración de la enfermedad y la ADP, mientras que ambos grupos fueron similares en términos de VMP, de niveles de colesterol y de parámetros hormonales.
ConclusiónAl parecer, el aumento de los parámetros de activación plaquetar, y especialmente la ADP, proporcionan una importante información para la progresión de la enfermedad y el seguimiento de la disfunción vascular en la disfunción eréctil.
Erectile dysfunction (ED) is defined as inability to provide and/or maintain sufficient erection for sexual activity.1 Although it is not a life-threatening condition, it affects quality of lives of both the patient and his partner. The prevalence of ED has been reported as 19–52%.2,3 The difference among the studies may be related to cultural and religious factors as well as different description of sexual dysfunction among individuals. Penile erection is a complex process that is affected by arterial dilation, smooth muscle relaxation, and veno-occlusive phenomena besides hormonal control.4
Aging, a sedentary life style, diabetes mellitus (DM), cardiovascular diseases (CVD), smoking, invasive surgical procedures performed due to prostate cancer, and chronic neurological diseases are the main risk factors in ED.5,6 Those risk factors cause increased oxidative stress and endothelial damage, and as a result, nitric oxide production decreases.7 Endothelial dysfunction forms the basis of common pathophysiological mechanisms of ED, atherosclerosis, stroke, and coronary artery disease. Platelet activation also plays an important role in inflammatory vascular response and atherothrombotic process.8 Mean platelet volume (MPV) and platelet distribution width (PDW) are the parameters that show platelet activation. Some studies showed correlation of MPV with cardiovascular disorders and metabolic risk factors.9 Two recent studies reported that PDW was a more specific platelet activation marker for atherosclerosis and coronary artery disease when compared to MPV.10,11 In our study, we investigated the relation of platelet activation factors with Doppler ultrasonography findings and disease severity in ED patients.
Materials and methodsIn our study, we retrospectively analyzed 293 patients who had color Doppler ultrasound (CDUS) with the diagnosis of ED between January 2010 and October 2014. The information about CDUS findings, serum glucose, triglyceride, glucose, total testosterone, prolactin, LH, FSH levels, and complete blood counts were obtained from the patients’ files. The patients who had DM, hyperprolactinemia, low testosterone levels or previous radical prostatectomy were excluded, and 91 patients were included in the study. MPV, PDW and platelet counts were derived from complete blood counts of the patients. All patients had a standard-protocol CDUS in our clinic, and their results were analyzed. Doppler ultrasound was performed with high-resolution Toshiba Aplio XG and General Electric Logiq 9 ultrasonography device (using 7.5MHz and 10MHz linear transducers, respectively) when the patient was in supine position. Anatomical structures and presence of fibrous plaques were investigated with longitudinal and transverse scans in gray scale imaging. Papaverine was injected into cavernous body near the root of penis using an insulin syringe, and spectral wave analyses were performed on minutes 5, 10, and 20. Doppler angle was maintained between 30° and 60°, and close to 60° as much as possible. An erection angle ≥90° was considered as normal. A peak systolic rate <35cm/s was regarded as arterial insufficiency, and an end diastolic rate >5cm/s was considered as venous insufficiency. The patients who had arterial insufficiency or venous-occlusive disorder were grouped as the ones with abnormal Doppler parameters, and the other patients were grouped as the ones with normal Doppler findings. The International Index of Erectile Function (IIEF-5) scores were obtained from the patients’ files. The patients with an IIEF score <12 were regarded to have severe disease, and the ones with a score between 12 and 25 were regarded to have mild disease.12
Statistical analysisStatistical analysis was performed using SPSS version 18.0 software (SPSS/IBM, Chicago, IL, USA). The Kolmogorov–Smirnov test and P–P plot were used to verify the normality of the distribution of continuous variables. The results were reported as mean±SD, or in situations in which the distributions were skewed, as the median (min–max). The categorical variables were given as percentages. The differences between the groups were analyzed with Mann–Whitney U test for nonparametric data whereas Chi-square/Fisher's exact tests were used for categorical variables. Any variable having a significant univariate test was selected as a candidate for the multivariate analysis. The logistic regression model was used to assess the statistical significance of the assumed risk factors in multivariate settings. In addition, ROC analysis was performed to define a cut off value for the PDW, which was found as an independent risk factor in the multivariate analysis. The highest point of sensitivity and specificity was determined as the cut-off value. Results were considered significant at p<0.05.
ResultsVascular dysfunction was found in 55 patients on CDUS (arterial insufficiency or veno-occlusive dysfunction) (Group I) while 36 patients had normal ultrasonographic findings (Group II). Those two groups were similar for smoking, levels of triglyceride, total testosterone, LH, FSH, prolactin, and platelet counts. Age, cholesterol level, disease duration, MPV, and PDW were significantly higher in Group I when compared to Group II. The demographic data and laboratory test results are presented in Table 1.
Demographic data and results of laboratory test.
| Vascular dysfunction on CDUS | p value | ||
|---|---|---|---|
| Yes | No | ||
| Number of patients | 55 | 36 | |
| Age (years) | 55.10±11.64 | 43.66±14±97 | <0.001* |
| Disease duration (months) | 25.96±16.87 | 16.44±7.51 | <0.001* |
| Cholesterol (mg/dL) | 172.2±34.9 | 154.6±31.2 | 0.018* |
| Triglyceride (mg/dL) | 116.3±37.9 | 120.4±39.7 | 0.622 |
| Smoking (%) | 37.5% | 36.1% | 0.374 |
| Testosterone (ng/ml) | 3.86±1.27 | 4.05±1.41 | 0.515 |
| LH (mlU/ml) | 5.72±2.39 | 5.45±3.38 | 0.674 |
| FSH (mlU/ml) | 6.96±3.45 | 6.15±3.70 | 0.437 |
| Prolactin (ng/ml) | 7.48±2.29 | 6.79±2.99 | 0.255 |
| Platelet number | 240.3±62.1×103 | 244.7±57.7×103 | 0.729 |
| PDW | 16.93±0.64 | 16.21±0.87 | <0.001* |
| MPV | 8.78±1.06 | 8.21±0.95 | 0.011* |
Analysis of the relation of PDW with other parameters showed that it had a negative correlation with IIEF score, and a positive correlation with disease duration (r=−0.230, p=0.029 and r=0.242, p=0.021, respectively). MPV showed a tendency to increase as disease duration increased, but the relation was not statistically significant (r=0.183, p=0.08). Multivariate regression analysis was performed for the risk factors that could cause pathological CDUS findings, and it was found that PDW and disease duration were independent prognostic factors, but MPV was not (p=0.02, p=0.005 and p=0.742, respectively).
When cut off for PDW was regarded as 16.4 in ROC analysis for pathological CDUS findings, the sensitivity was found as 80%, and the specificity was found as 61.1% (95% confidence interval 0.65–0.85, AUC: 0.75). In addition, age, disease duration and PDW showed significant differences between the groups when the patients were classified as the ones with mild (Group A) and severe (Group B) disease according to their IIEF scores; however MPV, cholesterol level and hormonal parameters did not show any significant differences between the groups. The laboratory parameters and demographic data of Groups A and B are presented in Table 2.
The laboratory parameters and demographic data of patients according to disease severity.
| Erectile dysfunction severity | p value | ||
|---|---|---|---|
| Mild | Severe | ||
| No. patients | 40 | 51 | |
| Age (years) | 46.5±14.4 | 53.6±13.1 | 0.017* |
| Disease duration (months) | 19.4±10.6 | 24.3±12.6 | 0.049 |
| Cholesterol (mg/dL) | 163.3±33.6 | 166.6±35.7 | 0.683 |
| Triglyceride (mg/dL) | 122.5±36.8 | 114.4±39.7 | 0.324 |
| Smoking (%) | 32.5% | 29.4% | 0.752 |
| Testosterone (ng/ml) | 3.76±1.43 | 4.07±1.24 | 0.287 |
| LH (mlU/ml) | 5.42±3.24 | 5.77±2.40 | 0.590 |
| FSH (mlU/ml) | 6.77±5.70 | 6.56±3.13 | 0.839 |
| Prolactin (ng/ml) | 6.66±2.48 | 7.65±2.61 | 0.095 |
| Platelet number | 244.1±61.3×103 | 240.4±59.7×103 | 0.774 |
| PDW | 16.4±0.92 | 16.8±0.69 | 0.031* |
| MPV | 8.61±1.09 | 8.51±1.03 | 0.675 |
Penile erection is a process that occurs with collaboration of neural and vascular functions. Nitric oxide is released from the nerve endings after parasympathetic activation, and it enters into cavernous smooth muscle cells and activates guanylate cyclase and adenylate cyclase enzymes. Phosphorylation of calcium channels and smooth muscle relaxation lead to blood flow into cavernous bodies. Inhibition of blood flow by distention and decreased blood flow into circulation play role in the maintenance of erection.12,13
A number of factors play role in development of ED. DM affects cavernous erectile contractility not only due to peripheral vascular injury, but also by increasing oxidative stress.14 Hypertension, dyslipidemia, DM, and smoking are risk factors not only for ED, but also for atherosclerosis and coronary artery disease. Platelets do not have nuclei (anucleated), they play role in atherosclerosis and inflammatory vascular response, and originate from megakaryocyes.15 MPV and PDW are routinely measured parameters in complete blood count, and they are known as platelet activation markers.16 Two recent studies in the literature reported that MPV increased in ED, however no studies up to date have investigated the relation of PDW with ED.15,17 In our study, we found higher MPV and PDW in patients who had vascular insufficiency in CDUS (p=0.011 and p<0.001; respectively). The difference between the groups for MPV was in correlation with the previous studies.15,17
Ciftci et al. performed a study on 50 patients and 40 controls, and reported that they did not find any correlation of MPV with age of the patient or disease duration.17 In our study, a correlation was found between the age of the patient and MPV (r=0.286, p=0.006). Although MPV tended to increase with increased disease duration, this was not statistically significant (r=0.183, p=0.08). We expected those results due to the association of MPV with both endothelial dysfunction and cardiovascular disease. Different from the aforementioned two studies, we performed a multivariate regression analysis, and found that PDW and disease duration were independent prognostic factors (p=0.02 and p=0.005, respectively), however MPV did not have such a relation. When cut-off for PDW was regarded as 16.4 in ROC analysis for pathological CDUS findings, the sensitivity was found as 80%, and the specificity was found as 61.1% (95% confidence interval 0.65–0.85, AUC: 0.75). PDW represents variations in platelet size, and may give more information than MPV for platelet reactivation.18
Only a few studies investigated the relation between PDW and cardiovascular diseases.19,20 Although some studies showed that MPV was a platelet activation marker in atherosclerosis, Bekler et al. reported that PDW was correlated with the severity of coronary artery disease in patients with acute coronary syndrome, while MPV did not have such a correlation.19,21 Similarly, Adam et al. reported that MPV was only higher in the patients with moderate stenosis on angiography. More than that, although they could not show any correlation between MPV and carotid artery stenosis on correlation analysis, PDW had a correlation, and it was an independent predictor for carotid artery stenosis. The studies in the literature that analyzed the relation of PDW with coronary artery disease and carotid artery stenosis support our findings.
When we grouped our patients as the ones with mild disease and the ones with severe disease according to their IIEF scores, MPV did not show any significant difference between two groups, however two groups showed a statistically significant difference for PDW. In addition to disease severity, PDW showed a positive correlation with duration of the disease. In our study, relation of PDW with disease severity and its correlation with vascular parameters indicate that it is more specific and valuable than MPV in patients with ED. Longer disease duration in patients with pathological Doppler ultrasound results and low IIEF scores indicate a progressive process.
ConclusionPlatelet activation factors such as MPV and PDW playing role in atherothrombotic process increase in ED patients with vascular dysfunction on CDUS. Our study has shown that PDW is a more specific marker compared to MPV, and gives more information about the disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestsThe authors have no conflict of interests to declare.