Changes in the traditional approaches to prevention, diagnosis, and therapeutic management of breast cancer are becoming increasingly genetically based. It is therefore important for nurses to have competency in underlying biology of carcinogenesis and the molecular rationale underlying strategies to prevent, diagnose, and treat breast cancer. The risk for breast cancer is increased in individuals carrying a mutation in a predisposing gene and in others with a number of affected relatives with early age of disease onset. The authors investigated perception of nurses on the role of genetics in the development of breast cancer.
Methods and materialA descriptive quantitative research design was adopted as the research design. The instrument for data collection was an adapted, pre-tested semi-structured, and self-administered questionnaire. Study participants were 187 nurses working at a tertiary health institution in Ekiti State. Data were analyzed and summarized using both descriptive and inferential statistics with level of significance set at P < .05.
ResultsThe mean age of respondents was 39 ± 9.1 years and majority (86.2%) were females and B.Sc. (Bachelor of Science) (53.2%), with more than a decade working experience (62.2%). The study revealed that knowledge of the role of genetics in development of breast cancer was low among respondents with only a few (25.6%) having good knowledge. Although majority of the respondents had good perception of genetic counseling, only 40% had good practice of genetic assessment and counseling with a few of them ever using “Family pedigree trees”, “ever referred a breast cancer patient for genetic assessment”, and with many reporting “difficulties guiding breast cancer patients in seeking genetic counselling”…
ConclusionDespite high level of education, knowledge, and practice of genetic counseling and assessment is poor among the respondents, with many reporting difficulties guiding breast cancer patients/relatives in seeking genetic counseling.
Los cambios de los enfoques tradicionales para la prevención, diagnóstico y manejo terapéutico del cáncer de mama se basan cada vez más en la genética. Por tanto, es importante que las enfermeras adquieran competencia en cuanto a la biología subyacente de la carcinogénesis y el fundamento molecular subyacente a las estrategias para la prevención, diagnóstico y tratamiento del cáncer de mama, cuyo riesgo se incrementa en los individuos portadores de mutaciones en genes predisponentes, y aquellos otros con familiares afectados por la enfermedad, con aparición temprana de la misma. Los autores investigaron la percepción de las enfermeras acera del rol de la genética en el desarrollo del cáncer de mama.
Métodos y MaterialSe adoptó un diseño de investigación cuantitativo y descriptivo. El instrumento para la recopilación de los datos fue un cuestionario adaptado, probado previamente, semiestructurado y autoadministrado. Participaron en el estudio 187 enfermeras que trabajaban en una institución sanitaria terciaria del Estado de Ekiti. Los datos fueron analizados y resumidos utilizando estadísticas descriptivas e inferenciales con un nivel de significación establecido en p < 0,05.
ResultadosLa edad media de los respondedores fue de 39 ± 9,1 años, siendo la mayoría mujeres (86,2%) y Licenciadas en Ciencias (53,2%), con más de una década de experiencia (62,2%). El estudio reveló que el conocimiento del papel de la genética en el desarrollo del cáncer de mama fue bajo entre los respondedores, y que solo el 25,6% de ellos tenía un buen conocimiento. Aunque la mayoría de los respondedores tenía una buena percepción del asesoramiento genético, solo el 40% tenía buena práctica sobre evaluación y asesoramiento genético, utilizando pocos de ellos “árboles genealógicos”, “no habían recomendado nunca la evaluación genética a un paciente de cáncer de mama” y reportando muchos de ellos “dificultades para orientar a los pacientes de cáncer a buscar asesoramiento genético”…
ConclusiónA pesar del alto nivel educativo, el conocimiento y la práctica del asesoramiento y la evaluación genética es débil entre los respondedores, reportando muchos que tenían dificultades a la hora de orientar a los pacientes/familiares de cáncer a la hora de buscar asesoramiento genético.
Globally, breast cancer is the most diagnosed cancer among women.1 An estimated 14.1 million new cases and 8.2 million breast cancer-related deaths occurred in 2012, compared to 12.7 million and 7.6 million, respectively, in 2008.1 Women typically present with advanced stages of the illness in low-middle-resource income countries including Nigeria.1 Some breast cancer cases follow a Mendelian inheritance pattern (autosomal dominant) and are characterized as hereditary. Human breast cancer is a clonal disease. This is a single transformed cell, that is the product of a series of somatic or germ line mutations that can eventually express full malignant potential.2 Thus, breast cancer may exist for an extended period as either a non-invasive or invasive but non-metastatic disease. Not more than 10% of human breast cancers can be linked directly to germ line mutations. Knowledge of somatic genetics and genomics will increase broad implications for the oncologist in the identification of new treatments modalities.2
Changes in the traditional approaches to prevention, diagnosis, and therapeutic management of breast cancer are becoming increasingly genetically based. Therefore, to ensure competency in oncology nursing practice at all levels, nurses must incorporate an understanding of the underlying biology of carcinogenesis and the molecular rationale underlying strategies to prevent, diagnose, and treat breast cancer. At the same time, nurses have a central role to play in the multidisciplinary teamwork involved in the care of patients with breast cancer and those at increased risk for the disease. Identification of risk factors for sporadic breast cancer and focus on risk assessment for the genetic aspects of hereditary breast cancers, are challenges for health promotion and cancer prevention within nursing practice. The challenges of genomic medicine indicate that nurses must understand the new technologies and treatments of gene-based health care. Therefore, it is essential to invest in the education and training of nurses, both in the recognition of risk factors and the criteria for referral of patients to maximize risk-reducing practices, especially in high-risk individuals.3,4 Thus, this study sought to assess the perception of nurses on the contribution of genetics to the development of breast cancer. The outcomes of this study might help to identify areas where training is needed to empower nurses to provide the essential role of providing effective assessment, counseling, and wholistic care for their patients.
MethodsStudy designA descriptive quantitative cross-sectional research design was used to elicit information on nurses' perception of role of genetics in development of breast cancer.
Study settingThe study setting was Federal Teaching Hospital (FETHI) Ido-Ekiti, Ekiti-State, South-West Nigeria. It was established in 1998 by Federal Government to provide affordable, qualitative, and accessible medical care to the people at the grassroots, particularly in Ekiti State.
The hospital is one of the fastest growing teaching hospitals in the country. It was upgraded to the status of a Federal Teaching Hospital in 2014. This facility is the only Federal Health Facility in Ekiti State. It is a major primary, secondary, and tertiary health service provider and clinical training institution in Nigeria,
Study populationStudy population consisted of nurses working at FETHI, within the study time frame. The total number of nurses working in Federal Teaching Hospital Ido-Ekiti was 356 nurses, as at the time of study. Data collection occurred between June and October 2021.
Sample size calculation and samplingSample size was determined using Taro Yamane formular:
Where n is the minimum sample size required, N is the total population = 356 for the nurses working in the health facility, and e is the sample error = 0.05. Inputting these values in the above formula, yielded a sample size of 187. To compensate for non-response or poorly filled questionnaire, an additional 10% was added which made the sample size 196. However, 187 responded to the questionnaire thereby, yielding a response rate of 95.4%.
Multistage sampling technique which includes proportionate sampling and simple random sampling technique were employed in the selection of study participants. A total of 187 nurses took part in the survey.
Instrument and method of data collectionThe instrument used for data collection was an adapted pre-tested semi-structured, self-administered questionnaire adapted from previous study.15 The questionnaire was divided into 4 sections, with each section covering each objective area. Section A obtained data on the participant's socio-demographic characteristics; Section B centered on perception measures, that is, nurses' perception of the role or contribution of genetics in development of breast cancer; Section C obtained data on genetic understanding and perception, while Section D concentrated on practice measures, that is, provision of genetic assessment and counseling.
Test–retest method was used to assess the reliability of the instrument. Internal consistency of items showed an intra-class correlation coefficient of 0.85. The questionnaires were administered by the researcher to the nurses in their respective wards/units during their shift periods. Ample time was allowed for questions which were all addressed by the researcher. Informed consent was obtained from study participants before administering the questionnaires.
Ethical considerationEthical approval was obtained from the Research and Ethics Committee of Federal Teaching Hospital, Ido-Ekiti (Protocol number: ERC/2021/02/19). where the study was carried out. All participants were aware of their rights and responsibilities as study participants. Verbal and written informed consents were obtained from the respondents before data collection. All methods were performed in accordance with the relevant guidelines and regulations.
Data analysisAfter data collection, questionnaire was rechecked for accuracy and completeness. A master sheet was prepared to enter data. Data were tabulated as per number of responses in master sheet for each item on the questionnaire and were arranged and entered in SPSS 25.0 version for further analysis. Descriptive statistics and inferential statistics (chi-square test) were used for the analysis of data after entering it into master sheet.
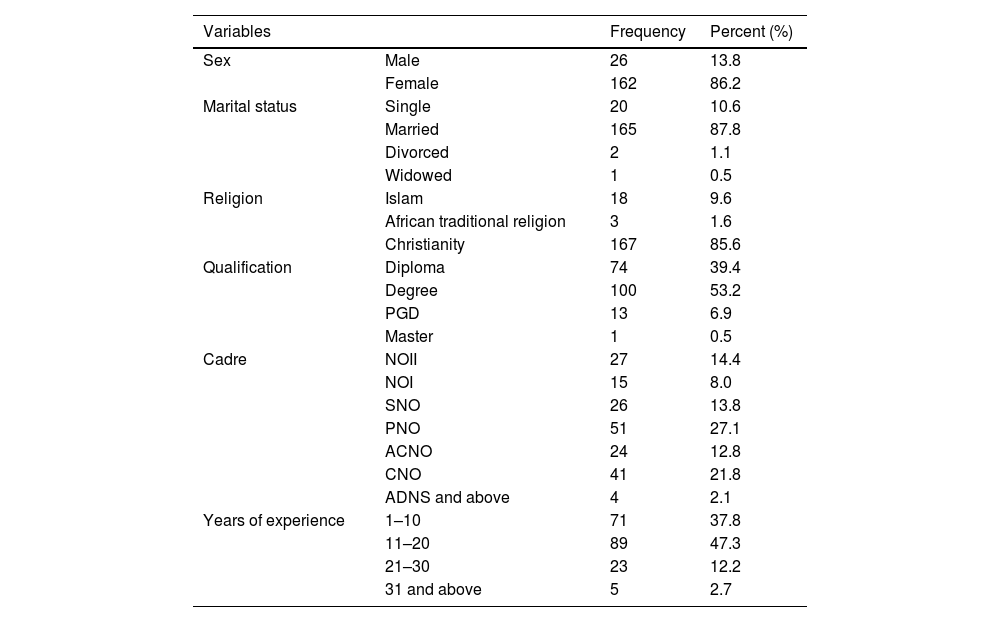
ResultsTable 1 depicts the socio-demographic characteristics of the respondents. The mean ± SD age of respondents was 39 ± 9.08 years. Majority (85.6%) of the nurses were Christians and married. The majority (85.1%) of the nurses were also females. Nurses with diploma certificates were more than one-quarter (39.4%) and those with degree were more than half (53.2%). A higher percentage (62.2%) of the respondents had more than 10 years working experience.
Socio-demographic characteristics of the respondents.
| Variables | Frequency | Percent (%) | |
|---|---|---|---|
| Sex | Male | 26 | 13.8 |
| Female | 162 | 86.2 | |
| Marital status | Single | 20 | 10.6 |
| Married | 165 | 87.8 | |
| Divorced | 2 | 1.1 | |
| Widowed | 1 | 0.5 | |
| Religion | Islam | 18 | 9.6 |
| African traditional religion | 3 | 1.6 | |
| Christianity | 167 | 85.6 | |
| Qualification | Diploma | 74 | 39.4 |
| Degree | 100 | 53.2 | |
| PGD | 13 | 6.9 | |
| Master | 1 | 0.5 | |
| Cadre | NOII | 27 | 14.4 |
| NOI | 15 | 8.0 | |
| SNO | 26 | 13.8 | |
| PNO | 51 | 27.1 | |
| ACNO | 24 | 12.8 | |
| CNO | 41 | 21.8 | |
| ADNS and above | 4 | 2.1 | |
| Years of experience | 1–10 | 71 | 37.8 |
| 11–20 | 89 | 47.3 | |
| 21–30 | 23 | 12.2 | |
| 31 and above | 5 | 2.7 |
***CNO = Chief Nursing Officer; SNO = Senior Nursing Officer; PNO = Principal Nursing Officer; ADNS = Assistant Director of Nursing Service; PGDE = Post Graduate Diploma in Education; NOI = Nursing Officer 1; NOII = Nursing Officer 2.
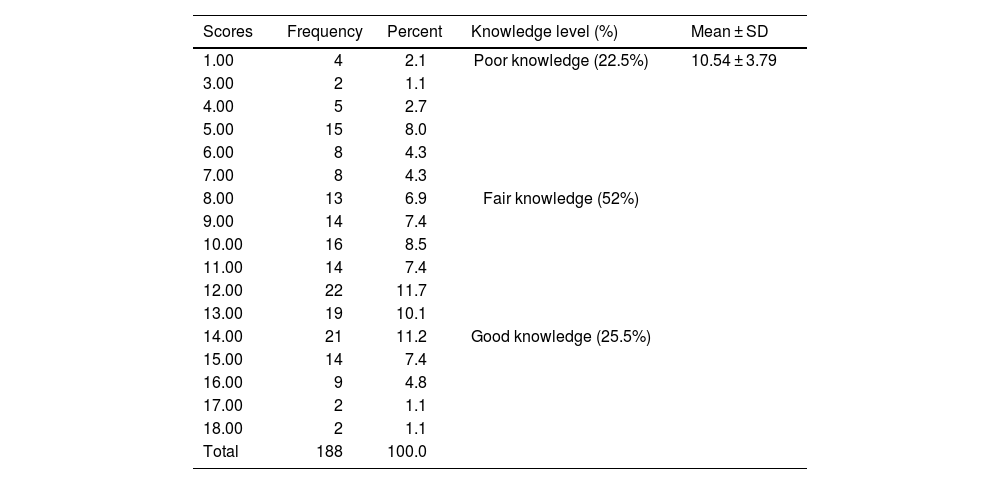
The results on knowledge level of nurses on the role genetics plays in development of breast cancer is presented in Table 2. The mean scale was adopted to categorize the knowledge into 3 levels: poor, fair, and good. Respondents who scored far below mean score of 10.54 were considered to have poor knowledge(1–7 marks), those who scored above the mean score (15–18 marks) were considered to have good knowledge and those with scores around the mean score were considered to have fair knowledge. Results reveled that almost one-quarter (22.5%) of the respondents had poor knowledge, while more than half (52%) had fair knowledge level, and one-quarter (25.6%) of the respondents had good knowledge respectively.
Performance of respondents on knowledge's questions.
| Scores | Frequency | Percent | Knowledge level (%) | Mean ± SD |
|---|---|---|---|---|
| 1.00 | 4 | 2.1 | Poor knowledge (22.5%) | 10.54 ± 3.79 |
| 3.00 | 2 | 1.1 | ||
| 4.00 | 5 | 2.7 | ||
| 5.00 | 15 | 8.0 | ||
| 6.00 | 8 | 4.3 | ||
| 7.00 | 8 | 4.3 | ||
| 8.00 | 13 | 6.9 | Fair knowledge (52%) | |
| 9.00 | 14 | 7.4 | ||
| 10.00 | 16 | 8.5 | ||
| 11.00 | 14 | 7.4 | ||
| 12.00 | 22 | 11.7 | ||
| 13.00 | 19 | 10.1 | ||
| 14.00 | 21 | 11.2 | Good knowledge (25.5%) | |
| 15.00 | 14 | 7.4 | ||
| 16.00 | 9 | 4.8 | ||
| 17.00 | 2 | 1.1 | ||
| 18.00 | 2 | 1.1 | ||
| Total | 188 | 100.0 |
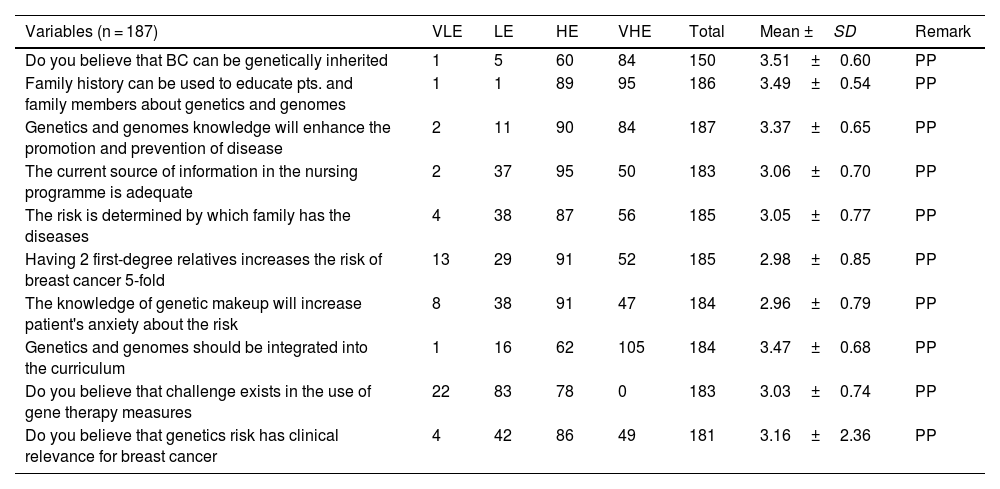
Table 3 present the results on perception of nurses towards the role of genetic in breast cancer development. All the 10 items on perception revealed that respondents had good perception of the role of genetics in breast cancer development. The mean values ranging from 2.96 to 3.51, which is far above weighted mean of 2.5.
Perception of respondents towards genetic role to breast cancer development.
| Variables (n = 187) | VLE | LE | HE | VHE | Total | Mean ±SD | Remark |
|---|---|---|---|---|---|---|---|
| Do you believe that BC can be genetically inherited | 1 | 5 | 60 | 84 | 150 | 3.51±0.60 | PP |
| Family history can be used to educate pts. and family members about genetics and genomes | 1 | 1 | 89 | 95 | 186 | 3.49±0.54 | PP |
| Genetics and genomes knowledge will enhance the promotion and prevention of disease | 2 | 11 | 90 | 84 | 187 | 3.37±0.65 | PP |
| The current source of information in the nursing programme is adequate | 2 | 37 | 95 | 50 | 183 | 3.06±0.70 | PP |
| The risk is determined by which family has the diseases | 4 | 38 | 87 | 56 | 185 | 3.05±0.77 | PP |
| Having 2 first-degree relatives increases the risk of breast cancer 5-fold | 13 | 29 | 91 | 52 | 185 | 2.98±0.85 | PP |
| The knowledge of genetic makeup will increase patient's anxiety about the risk | 8 | 38 | 91 | 47 | 184 | 2.96±0.79 | PP |
| Genetics and genomes should be integrated into the curriculum | 1 | 16 | 62 | 105 | 184 | 3.47±0.68 | PP |
| Do you believe that challenge exists in the use of gene therapy measures | 22 | 83 | 78 | 0 | 183 | 3.03±0.74 | PP |
| Do you believe that genetics risk has clinical relevance for breast cancer | 4 | 42 | 86 | 49 | 181 | 3.16±2.36 | PP |
***VLE = Very low extent; LE = Low extent; HE = High extent; VHE = Very high extent.
PP = Positive perception; NP = Negative perception; BC = Breast cancer.
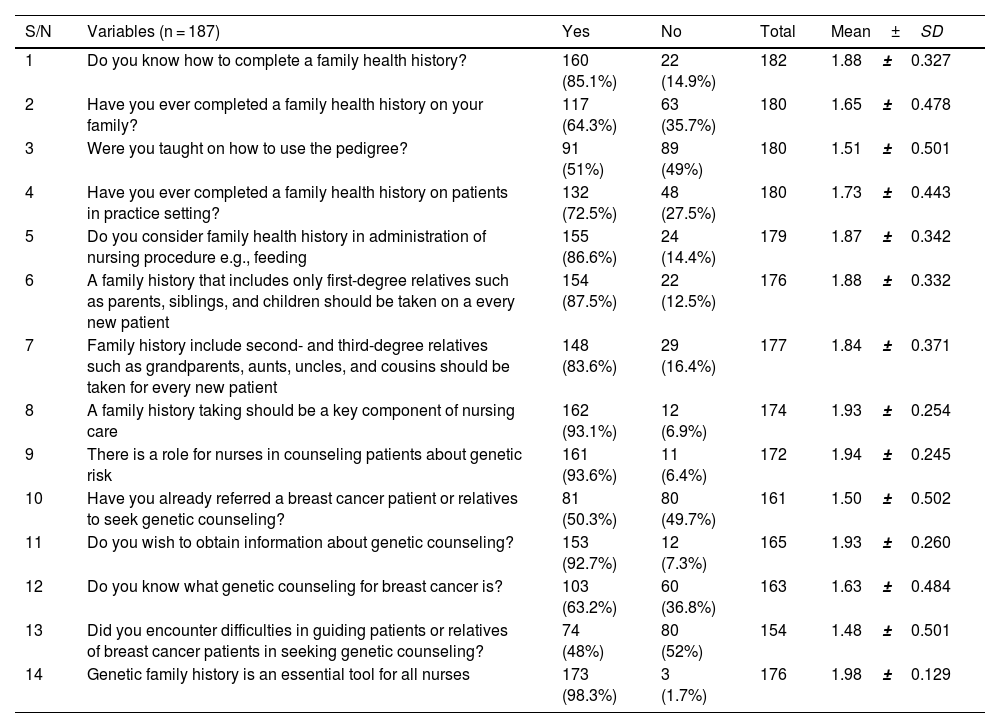
Table 4 reveals the results on the practice of nurses in genetic assessment and counseling of patient with breast cancer. Majority (85.1%) of the respondents claimed to know how to complete a family health history, however, only 64.3% had ever completed a family health history. Furthermore, only about average (51%) have been taught on how to use family pedigree, ever referred a breast cancer patients/relative for genetic assessment (50.3%) and less than average (48%), said they encountered difficulties guiding patients/relatives of breast cancer patients in seeking genetic counseling. Moreover, almost all the participants (92.7%) said they wish to obtain information/education on genetic counseling and assessment. The composite score for practice was graded on a 3-point scale (good practice, fair practice, and poor practice). The scale consists of the levels of practice; the maximum value was 2 and the minimum value was 1. Poor practice had any value less than or equal to 1.60 (≤1.60), fair practice ranges from 1.61 to 1.80; while good practice includes all values above 180 (1.81–2.00). The overall summary index for practice of genetic counseling and assessment among respondents revealed that 40% of the respondents had good practice, 43% had fair practice while 17% had poor practice.
Assessment of practice genetic counseling among respondents.
| S/N | Variables (n = 187) | Yes | No | Total | Mean±SD |
|---|---|---|---|---|---|
| 1 | Do you know how to complete a family health history? | 160 (85.1%) | 22 (14.9%) | 182 | 1.88±0.327 |
| 2 | Have you ever completed a family health history on your family? | 117 (64.3%) | 63 (35.7%) | 180 | 1.65±0.478 |
| 3 | Were you taught on how to use the pedigree? | 91 (51%) | 89 (49%) | 180 | 1.51±0.501 |
| 4 | Have you ever completed a family health history on patients in practice setting? | 132 (72.5%) | 48 (27.5%) | 180 | 1.73±0.443 |
| 5 | Do you consider family health history in administration of nursing procedure e.g., feeding | 155 (86.6%) | 24 (14.4%) | 179 | 1.87±0.342 |
| 6 | A family history that includes only first-degree relatives such as parents, siblings, and children should be taken on a every new patient | 154 (87.5%) | 22 (12.5%) | 176 | 1.88±0.332 |
| 7 | Family history include second- and third-degree relatives such as grandparents, aunts, uncles, and cousins should be taken for every new patient | 148 (83.6%) | 29 (16.4%) | 177 | 1.84±0.371 |
| 8 | A family history taking should be a key component of nursing care | 162 (93.1%) | 12 (6.9%) | 174 | 1.93±0.254 |
| 9 | There is a role for nurses in counseling patients about genetic risk | 161 (93.6%) | 11 (6.4%) | 172 | 1.94±0.245 |
| 10 | Have you already referred a breast cancer patient or relatives to seek genetic counseling? | 81 (50.3%) | 80 (49.7%) | 161 | 1.50±0.502 |
| 11 | Do you wish to obtain information about genetic counseling? | 153 (92.7%) | 12 (7.3%) | 165 | 1.93±0.260 |
| 12 | Do you know what genetic counseling for breast cancer is? | 103 (63.2%) | 60 (36.8%) | 163 | 1.63±0.484 |
| 13 | Did you encounter difficulties in guiding patients or relatives of breast cancer patients in seeking genetic counseling? | 74 (48%) | 80 (52%) | 154 | 1.48±0.501 |
| 14 | Genetic family history is an essential tool for all nurses | 173 (98.3%) | 3 (1.7%) | 176 | 1.98±0.129 |
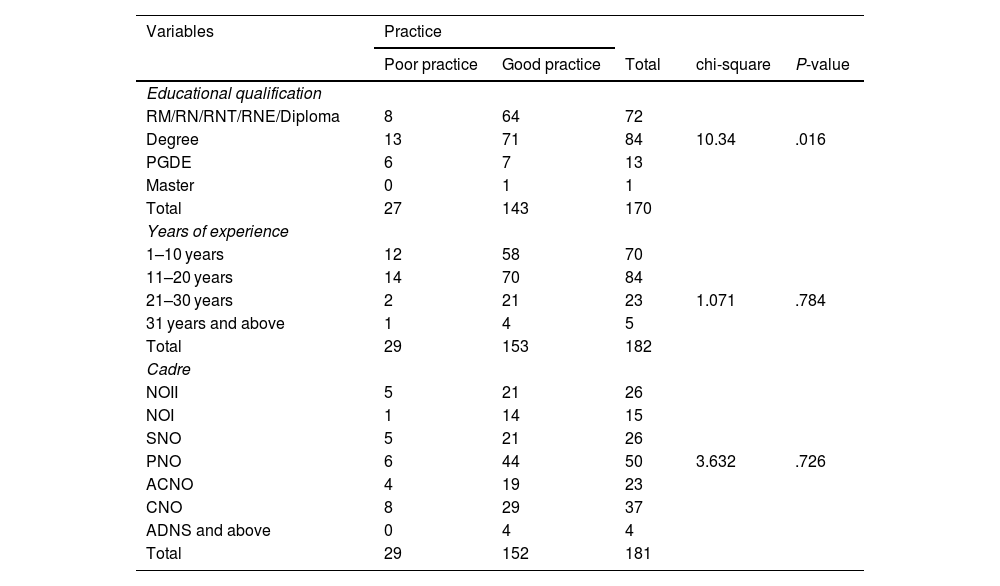
Bivariate analysis testing association between respondents' socio-demographic characteristics (cadre, year of experience, and highest educational qualification) and the practice of genetic counseling is presented in Table 5. Only educational attainment of respondents was significantly associated with the practice of genetic counseling.
Relationship between practice and some socio-demographic characteristics.
| Variables | Practice | ||||
|---|---|---|---|---|---|
| Poor practice | Good practice | Total | chi-square | P-value | |
| Educational qualification | |||||
| RM/RN/RNT/RNE/Diploma | 8 | 64 | 72 | ||
| Degree | 13 | 71 | 84 | 10.34 | .016 |
| PGDE | 6 | 7 | 13 | ||
| Master | 0 | 1 | 1 | ||
| Total | 27 | 143 | 170 | ||
| Years of experience | |||||
| 1–10 years | 12 | 58 | 70 | ||
| 11–20 years | 14 | 70 | 84 | ||
| 21–30 years | 2 | 21 | 23 | 1.071 | .784 |
| 31 years and above | 1 | 4 | 5 | ||
| Total | 29 | 153 | 182 | ||
| Cadre | |||||
| NOII | 5 | 21 | 26 | ||
| NOI | 1 | 14 | 15 | ||
| SNO | 5 | 21 | 26 | ||
| PNO | 6 | 44 | 50 | 3.632 | .726 |
| ACNO | 4 | 19 | 23 | ||
| CNO | 8 | 29 | 37 | ||
| ADNS and above | 0 | 4 | 4 | ||
| Total | 29 | 152 | 181 | ||
***RN = Registered Nurse; RM = Registered Midwife; RNT = Registered Nurse Tutor; RNE = Registered Nurse Educator; CNO = Chief Nursing Officer, SNO = Senior Nursing Officer, PNO = Principal Nursing Officer; ADNS = Assistant Director of Nursing Service; PGD = Post Graduate Diploma; ACNO = Assistant Chief Nursing Officer; NOI = Nursing Officer 1; NOII = Nursing Officer 2.
Almost one-quarter (22.5%) of the respondents had poor knowledge by scoring below 8 marks, more than half (52%) of the respondents had fair knowledge by scoring between 8 and 13 marks, while one-quarter (25.6%) had good knowledge about the role of genetics in development of breast cancer by scoring above 14 marks. This finding is in contrast with study of Alfayyad et al. 5 who reported that health care professionals demonstrated fair knowledge and only 1.5% had good knowledge and the study findings of Balekouzoou et al.,6 who discovered that 13.9% had good knowledge and 17.1% had poor knowledge. This current study finding also contradicted Andegiogish et al.7 who indicated that nurses had low knowledge and Ngene et al.8 findings of 15.3% score, a value below average in knowledge items.
Nurses perception on the role of geneticsThe findings of the study on perception of nurses on the role of genetics in the development of breast cancer revealed a good perception. Thirteen (13) items on perception indicated good perception while only 1 item indicated poor perception. This finding also correlates with higher practice of genetic counseling. This study outcome supports the suggestion of Tilburt et al.9 that perception of risk can either increase or decrease use of screening and preventive services. Higher risk perceptions are generally associated with higher levels of screening.10,11
Nurses' practice of genetic assessment and counselingFrom the 14 items that elicited their practice, the mean score of 13 items were above the expected mean of 1.5 while the mean score of only 1 item was below the expected mean. This implies that the nurses had good practice. Nurses in the studied population engage in a great deal of genetic assessment and counseling of patient with breast cancer. This finding is at variance with the findings of Gallas12 where majority (73.8%) of the respondents had poor practice of breast cancer screening. The reason might have explained the recent increase in the incidence of breast cancer recorded in Tunisia which indicated that if early detection of breast cancer had been effective, the increase in incidence of breast cancer might not have arisen.
The practice of genetic assessment and counseling among patient with breast cancer by nurses with respect to designation of nurses and years of experience were found to be non-significant but relationship between practice and level of education was found to be significant at 0.05 level of significance. Idvaii et al.13 in a study on nurses' socio-demographic background and assessment of individualized care revealed that background experience like educational level, cadre, age, length of working experience, and race were not significant variables.
Association between selected socio-demographic characteristics and nurses' perceptionThe null hypothesis on association between socio-demographic (educational level and year of experience) and perception of nurses was not rejected. Sakai et al.14 accounted for a significant relationship between perception of health care professionals and educational level, the participants had a diverse perception which contradicted to the findings of this study.
Balekouzou et al.6 reported that there was no statistically significant association observed between different cadres on knowledge level of role of genetics in development of breast cancer. The report agreed with findings of this study by affirming mean score between cadres of nurses was not significant.
The study concludes that the nurses had poor knowledge of the role of genetics in breast cancer development. They practice a fair level of genetic assessment and counseling of breast cancer patients, although participants had good perception of genetic counseling and assessment. This practice level significantly relates with their educational qualification on the contribution of genetics in the development of breast cancer. However, there is need for frequent continuous educational updates in these areas.
RecommendationsBased on the outcomes of this study, it is recommended that seminars and conferences on the role of genetics in development of breast cancer among nurses should be organized to improve nurses' knowledge. Nurses in FETH, Ido-Ekiti should continue to update their counseling skills to provide effective care and services for their clients.
FundingThis study did not receive any specific grant from funding agancies in the public, commercial, or not-for-profit sectors.
Ethical considerationsEthical approval was obtained from the Research and Ethics Committee of Afe Babalola University, Ado-Ekiti, Ekiti State and Research and Ethics Committee of Federal Teaching Hospital, Ido-Ekiti, (Protocol number: ERC/2021/02/19). where the study was carried out. All participants were aware of their ethical rights and responsibilities as study participants. Verbal and written informed consents were obtained from the respondents before data collection. All methods were performed in accordance with the relevant guidelines and regulations.
Author contributionsAll authors made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
The authors acknowledge and thank all the participants in this study.