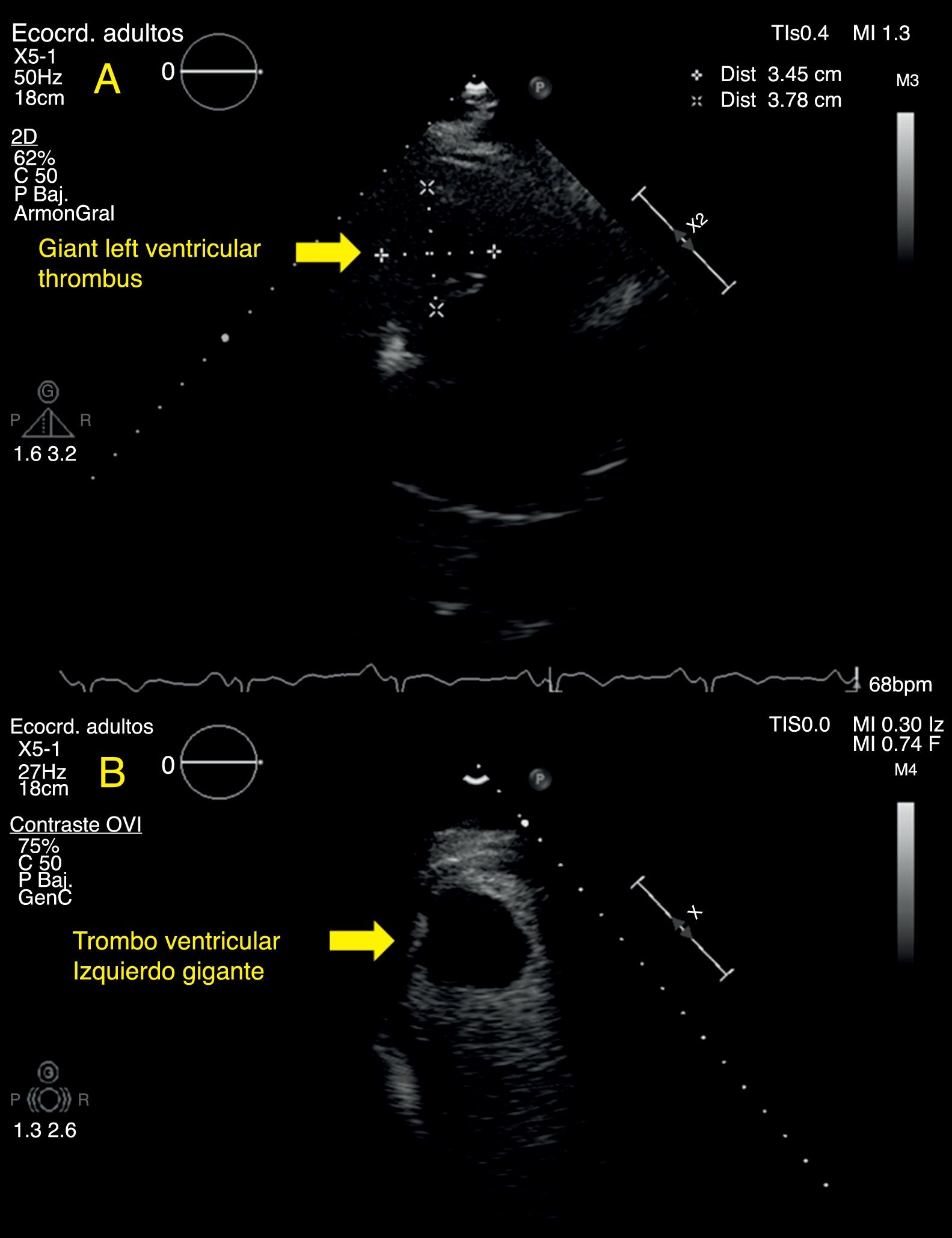
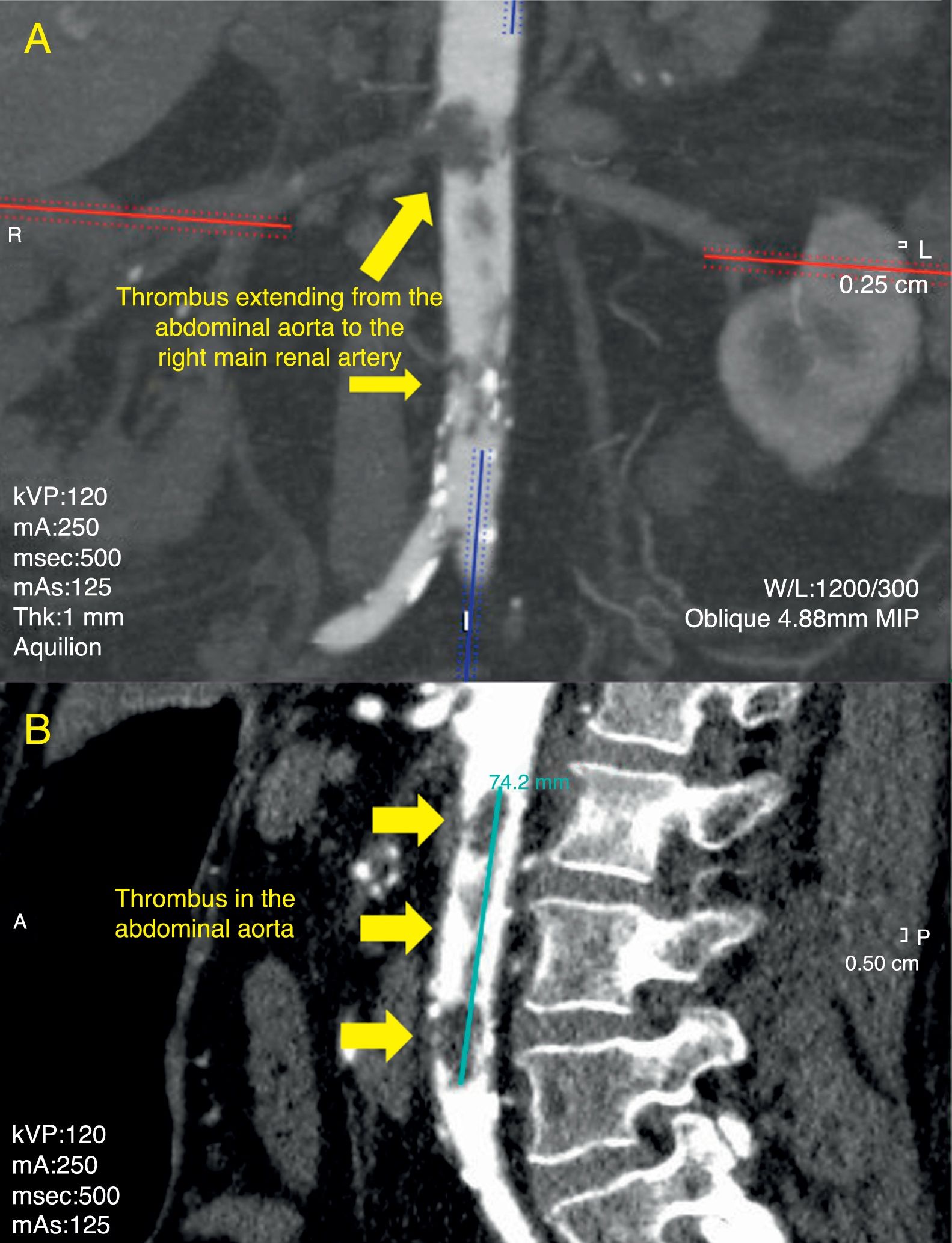
array:24 [ "pii" => "S2341192918300982" "issn" => "23411929" "doi" => "10.1016/j.redare.2018.06.004" "estado" => "S300" "fechaPublicacion" => "2018-08-01" "aid" => "914" "copyright" => "Sociedad Española de Anestesiología, Reanimación y Terapéutica del Dolor" "copyrightAnyo" => "2018" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Revista Española de Anestesiología y Reanimación (English Version). 2018;65:414-6" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:19 [ "pii" => "S0034935618300495" "issn" => "00349356" "doi" => "10.1016/j.redar.2018.02.001" "estado" => "S300" "fechaPublicacion" => "2018-08-01" "aid" => "914" "copyright" => "Sociedad Española de Anestesiología, Reanimación y Terapéutica del Dolor" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Rev Esp Anestesiol Reanim. 2018;65:414-6" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 76 "formatos" => array:2 [ "HTML" => 46 "PDF" => 30 ] ] "es" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Carta al Director</span>" "titulo" => "Embolismo de trombo ventricular izquierdo gigante hacia aorta abdominal" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "414" "paginaFinal" => "416" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Giant left ventricular thrombus embolism into the abdominal aorta" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0010" "etiqueta" => "Figura 2" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr2.jpeg" "Alto" => 2067 "Ancho" => 1583 "Tamanyo" => 271997 ] ] "descripcion" => array:1 [ "es" => "<p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">TC toracoabdominal. A) Extensión de trombo en aorta abdominal a la arteria renal principal derecha. B) Trombo flotante de 75<span class="elsevierStyleHsp" style=""></span>mm en aorta abdominal.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "J. Urmeneta Ulloa, A. Pérez Guerrero, I. Molina Borao, F. Fuentes Gorgas, A. Miñano Oyarzabal" "autores" => array:5 [ 0 => array:2 [ "nombre" => "J." "apellidos" => "Urmeneta Ulloa" ] 1 => array:2 [ "nombre" => "A." "apellidos" => "Pérez Guerrero" ] 2 => array:2 [ "nombre" => "I." "apellidos" => "Molina Borao" ] 3 => array:2 [ "nombre" => "F." "apellidos" => "Fuentes Gorgas" ] 4 => array:2 [ "nombre" => "A." "apellidos" => "Miñano Oyarzabal" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2341192918300982" "doi" => "10.1016/j.redare.2018.06.004" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2341192918300982?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0034935618300495?idApp=UINPBA00004N" "url" => "/00349356/0000006500000007/v1_201807200902/S0034935618300495/v1_201807200902/es/main.assets" ] ] "itemSiguiente" => array:19 [ "pii" => "S2341192918301185" "issn" => "23411929" "doi" => "10.1016/j.redare.2018.04.009" "estado" => "S300" "fechaPublicacion" => "2018-08-01" "aid" => "932" "copyright" => "Sociedad Española de Anestesiología, Reanimación y Terapéutica del Dolor" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Revista Española de Anestesiología y Reanimación (English Version). 2018;65:416-7" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Director</span>" "titulo" => "Anesthesia technique and quality of recovery after laparoscopic cholecystectomy: Case closed?" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "416" "paginaFinal" => "417" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Técnica anestésica y calidad de la recuperación tras colecistectomía laparoscópica: ¿un caso cerrado?" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "L.J. Castro Alves, M.C. Kendall" "autores" => array:2 [ 0 => array:2 [ "nombre" => "L.J." "apellidos" => "Castro Alves" ] 1 => array:2 [ "nombre" => "M.C." "apellidos" => "Kendall" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0034935618300963" "doi" => "10.1016/j.redar.2018.04.005" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0034935618300963?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2341192918301185?idApp=UINPBA00004N" "url" => "/23411929/0000006500000007/v1_201807260406/S2341192918301185/v1_201807260406/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2341192918301124" "issn" => "23411929" "doi" => "10.1016/j.redare.2018.02.015" "estado" => "S300" "fechaPublicacion" => "2018-08-01" "aid" => "919" "copyright" => "Sociedad Española de Anestesiología, Reanimación y Terapéutica del Dolor" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Revista Española de Anestesiología y Reanimación (English Version). 2018;65:413-4" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Director</span>" "titulo" => "Reflections on the “opioid crisis”: Prevention is better than cure" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "413" "paginaFinal" => "414" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Reflexiones sobre la «crisis de los opioides»: más vale prevenir que curar" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "A. Alcántara Montero, A. González Curado" "autores" => array:2 [ 0 => array:2 [ "nombre" => "A." "apellidos" => "Alcántara Montero" ] 1 => array:2 [ "nombre" => "A." "apellidos" => "González Curado" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0034935618300549" "doi" => "10.1016/j.redar.2018.02.005" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0034935618300549?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2341192918301124?idApp=UINPBA00004N" "url" => "/23411929/0000006500000007/v1_201807260406/S2341192918301124/v1_201807260406/en/main.assets" ] "en" => array:16 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Director</span>" "titulo" => "Giant left ventricular thrombus embolism into the abdominal aorta" "tieneTextoCompleto" => true "saludo" => "To the Editor," "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "414" "paginaFinal" => "416" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "J. Urmeneta Ulloa, A. Pérez Guerrero, I. Molina Borao, F. Fuentes Gorgas, A. Miñano Oyarzabal" "autores" => array:5 [ 0 => array:4 [ "nombre" => "J." "apellidos" => "Urmeneta Ulloa" "email" => array:1 [ 0 => "javierurmeneta@hotmail.com" ] "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] 1 => array:2 [ "nombre" => "A." "apellidos" => "Pérez Guerrero" ] 2 => array:2 [ "nombre" => "I." "apellidos" => "Molina Borao" ] 3 => array:2 [ "nombre" => "F." "apellidos" => "Fuentes Gorgas" ] 4 => array:2 [ "nombre" => "A." "apellidos" => "Miñano Oyarzabal" ] ] "afiliaciones" => array:1 [ 0 => array:2 [ "entidad" => "Hospital Universitario Miguel Servet, Zaragoza, Spain" "identificador" => "aff0005" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Embolismo de trombo ventricular izquierdo gigante hacia aorta abdominal" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 2059 "Ancho" => 1583 "Tamanyo" => 147089 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0020" class="elsevierStyleSimplePara elsevierViewall">Modified two chamber apical TEE: (A) left ventricular thrombus (LVT) and (B) SonoVue<span class="elsevierStyleSup">®</span> contrast showing the giant, pedunculated apical LVT.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">A 65-year-old woman, ex-smoker, diabetic and dyslipidaemic, with a history of acute anteroseptal myocardial infarction (AMI) in 2007 that was treated with fibrinolysis and subsequent urgent coronary angiography, during which percutaneous coronary intervention (PCI) was performed on the mid segment of the anterior descending artery (DA) and on the mid to proximal segment of the right coronary artery (RA), was admitted in May 2017 for a stroke. Transthoracic echocardiography (TTE) showed a suboptimal transthoracic window, so SonoVue<span class="elsevierStyleSup">®</span> contrast medium was administered. The resulting image showed: dilated left ventricle (LV), mild-moderate LV systolic dysfunction (40% left ventricular ejection fraction [LVEF] estimated by the Simpson method), extensive apical akinesia with aneurysmal formation, and a pedunculated, mobile, echodense image measuring 38<span class="elsevierStyleHsp" style=""></span>mm<span class="elsevierStyleHsp" style=""></span>×<span class="elsevierStyleHsp" style=""></span>35<span class="elsevierStyleHsp" style=""></span>mm in the same region that was not captured by the SonoVue<span class="elsevierStyleSup">®</span> contrast, compatible with apical thrombus (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>).</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0010" class="elsevierStylePara elsevierViewall">In view of this finding, the patient was transferred to cardiology, where she was immediately started on intravenous heparin (5.1<span class="elsevierStyleHsp" style=""></span>mg/kg every 24<span class="elsevierStyleHsp" style=""></span>h, activated partial thromboplastin time 45.5<span class="elsevierStyleHsp" style=""></span>s), and the surgical and medical teams discussed the need for thrombectomy. After the start of anticoagulant therapy (24–48<span class="elsevierStyleHsp" style=""></span>h), the patient presented acute pulmonary oedema. Urgent echocardioscopy showed severe LV systolic dysfunction (estimated visual LVEF of 15–20%), akinesia in the mid and apical segments, with no sign of apical thrombus. The patient then presented cardiorespiratory arrest, but recovered sinus rhythm after advanced CPR manoeuvres and early defibrillation due to ventricular fibrillation. Emergency thoracoabdominal CT scan showed a filling defect with a free-floating thrombus measuring 75<span class="elsevierStyleHsp" style=""></span>mm in length in the abdominal aorta extending to the main right renal artery and the proximal segment of the inferior mesenteric artery (<a class="elsevierStyleCrossRef" href="#fig0010">Fig. 2</a>). We also observed splenic and left renal infarctions, and absence of right renal perfusion caused by the thrombotic obstruction of the renal artery. At the thoracic level, the scan showed bilateral pleural effusion and collapse of both lower pulmonary lobes, without images compatible with pulmonary thromboembolism at any level.</p><elsevierMultimedia ident="fig0010"></elsevierMultimedia><p id="par0015" class="elsevierStylePara elsevierViewall">The patient was sent for emergency vascular surgery involving thrombectomy of the superior mesenteric, aorto-iliac, iliofemoral and femoropopliteal arteries, during which a large amount of thrombotic material was extracted. Macroscopic findings of small bowel ischaemia were observed during surgery, so a new arteriotomy of the thrombosed superior mesenteric artery was performed using a horizontal incision to extract the thrombus. The incision was closed with a biological patch. Intestinal perfusion improved, and after an evaluation by general surgery a wait and see approach was decided. On arrival at the ICU the patient presented considerable haemodynamic instability, and was given maximum-dose noradrenaline and intravenous dobutamine. She then presented multiorgan failure, which was treated with renal replacement therapy with ultrafiltration, despite which she progressed to fulminant sepsis within 6<span class="elsevierStyleHsp" style=""></span>h and died.</p><p id="par0020" class="elsevierStylePara elsevierViewall">The formation of a large left ventricular thrombus (LVT) is considered an infrequent and very serious complication of ischaemic heart disease, particularly in the context of an acute myocardial infarction. The clinical relevance of this complication is the increased risk of the thromboembolism migrating to the arterial<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">1</span></a> system, including the abdominal aorta.<a class="elsevierStyleCrossRef" href="#bib0035"><span class="elsevierStyleSup">2</span></a></p><p id="par0025" class="elsevierStylePara elsevierViewall">Guidelines currently recommend treating LVT with anticoagulation agents. This is questioned by some groups. For example, Lee et al.<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">1</span></a> evaluated various therapeutic LVT strategies (anticoagulation, antiplatelet therapy, or surgical treatment) in 62 patients with LVT over a mean follow-up period of 24 months, the longest to date. Their results show that high embolic risk patients (female sex, previous cerebrovascular disease, large, multiple, pedunculated or highly mobile thrombi, and increased left ventricular diastolic diameter) could benefit more from surgical thrombectomy than medical treatment: a greater number of post-treatment embolic events and a higher rate of bleeding were observed in the medical treatment group.<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">1</span></a> Some authors have suggested that thrombectomy using the left atriotomy approach, extracting the thrombus through the mitral valve, could be an alternative to conventional ventriculotomy in patients with large, mobile pediculated thrombi, and would avoid deterioration of the LV function that is associated with ventriculotomy.<a class="elsevierStyleCrossRef" href="#bib0040"><span class="elsevierStyleSup">3</span></a></p><p id="par0030" class="elsevierStylePara elsevierViewall">Leick et al., on the other hand, showed that high-dose intravenous heparin resolved 83% of cases of mobile, protruding thrombi.<a class="elsevierStyleCrossRef" href="#bib0045"><span class="elsevierStyleSup">4</span></a> Finally, groups with experience in fibrinolysis have shown this technique to be a promising therapeutic option in these cases. Other authors, in contrast, have reported embolic events after fibrinolysis.<a class="elsevierStyleCrossRef" href="#bib0045"><span class="elsevierStyleSup">4</span></a></p><p id="par0035" class="elsevierStylePara elsevierViewall">There is currently no consensus on the best therapeutic strategy in these cases; however, our experience and that of several other authors,<a class="elsevierStyleCrossRefs" href="#bib0045"><span class="elsevierStyleSup">4,5</span></a> suggests that surgical thrombectomy is probably the best first-line therapy in patients with large, pedunculated, mobile thrombi that are typically associated with high embolic risk. The management of intraventricular thrombi, therefore, is a medical-surgical emergency, where speed and aggressive action are key to mitigating the high risk of mortality in these patients.</p></span>" "pdfFichero" => "main.pdf" "tienePdf" => true "NotaPie" => array:1 [ 0 => array:2 [ "etiqueta" => "☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">Please cite this article as: Urmeneta Ulloa J, Pérez Guerrero A, Molina Borao I, Fuentes Gorgas F, Miñano Oyarzabal A. Embolismo de trombo ventricular izquierdo gigante hacia aorta abdominal. Rev Esp Anestesiol Reanim. 2018;65:414–416.</p>" ] ] "apendice" => array:1 [ 0 => array:1 [ "seccion" => array:1 [ 0 => array:4 [ "apendice" => "<p id="par0045" class="elsevierStylePara elsevierViewall"><elsevierMultimedia ident="upi0005"></elsevierMultimedia><elsevierMultimedia ident="upi0010"></elsevierMultimedia><elsevierMultimedia ident="upi0015"></elsevierMultimedia></p>" "etiqueta" => "Appendix A" "titulo" => "Supplementary data" "identificador" => "sec0010" ] ] ] ] "multimedia" => array:5 [ 0 => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 2059 "Ancho" => 1583 "Tamanyo" => 147089 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0020" class="elsevierStyleSimplePara elsevierViewall">Modified two chamber apical TEE: (A) left ventricular thrombus (LVT) and (B) SonoVue<span class="elsevierStyleSup">®</span> contrast showing the giant, pedunculated apical LVT.</p>" ] ] 1 => array:7 [ "identificador" => "fig0010" "etiqueta" => "Figure 2" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr2.jpeg" "Alto" => 2067 "Ancho" => 1583 "Tamanyo" => 289249 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0025" class="elsevierStyleSimplePara elsevierViewall">Thoracoabdominal CT: (A) thrombus extending from the abdominal aorta to the right main renal artery and (B) floating thrombus measuring 75<span class="elsevierStyleHsp" style=""></span>mm in the abdominal aorta.</p>" ] ] 2 => array:6 [ "identificador" => "upi0005" "tipo" => "MULTIMEDIAECOMPONENTE" "mostrarFloat" => false "mostrarDisplay" => true "Ecomponente" => array:3 [ "fichero" => "mmc1.mp4" "ficheroTamanyo" => 367739 "Video" => array:2 [ "flv" => array:5 [ "fichero" => "mmc1.flv" "poster" => "mmc1.jpg" "tiempo" => 0 "alto" => 0 "ancho" => 0 ] "mp4" => array:5 [ "fichero" => "mmc1.m4v" "poster" => "mmc1.jpg" "tiempo" => 0 "alto" => 0 "ancho" => 0 ] ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Video 1 Four chamber apical TTE. Sub-optimal transthoracic window. Difficult visualization of the left ventricular apical thrombus.</p>" ] ] 3 => array:6 [ "identificador" => "upi0010" "tipo" => "MULTIMEDIAECOMPONENTE" "mostrarFloat" => false "mostrarDisplay" => true "Ecomponente" => array:3 [ "fichero" => "mmc2.mp4" "ficheroTamanyo" => 248274 "Video" => array:2 [ "flv" => array:5 [ "fichero" => "mmc2.flv" "poster" => "mmc2.jpg" "tiempo" => 0 "alto" => 0 "ancho" => 0 ] "mp4" => array:5 [ "fichero" => "mmc2.m4v" "poster" => "mmc2.jpg" "tiempo" => 0 "alto" => 0 "ancho" => 0 ] ] ] "descripcion" => array:1 [ "en" => "<p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">Video 2 Parasternal TTE. Sub-optimal transthoracic window.</p>" ] ] 4 => array:6 [ "identificador" => "upi0015" "tipo" => "MULTIMEDIAECOMPONENTE" "mostrarFloat" => false "mostrarDisplay" => true "Ecomponente" => array:3 [ "fichero" => "mmc3.mp4" "ficheroTamanyo" => 339496 "Video" => array:2 [ "flv" => array:5 [ "fichero" => "mmc3.flv" "poster" => "mmc3.jpg" "tiempo" => 0 "alto" => 0 "ancho" => 0 ] "mp4" => array:5 [ "fichero" => "mmc3.m4v" "poster" => "mmc3.jpg" "tiempo" => 0 "alto" => 0 "ancho" => 0 ] ] ] "descripcion" => array:1 [ "en" => "<p id="spar0015" class="elsevierStyleSimplePara elsevierViewall">Video 3 TEE with SonoVue<span class="elsevierStyleSup">®</span> contrast. Left ventricular apical thrombus.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0015" "bibliografiaReferencia" => array:5 [ 0 => array:3 [ "identificador" => "bib0030" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Left ventricular thrombus and subsequent thromboembolism, comparison of anticoagulation, surgical removal, and antiplatelet agents" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "J.M. Lee" 1 => "J.J. Park" 2 => "H.W. Jung" 3 => "Y.S. Cho" 4 => "I.Y. Oh" 5 => "C.H. Yoon" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "J Atheroscler Thromb" "fecha" => "2013" "volumen" => "20" "paginaInicial" => "73" "paginaFinal" => "93" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/22986555" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0035" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Migration of left ventricular thrombus causing abdominal aortic embolism during cardiac surgery in a child with severe left ventricular dysfunction" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "M. Nagashima" 1 => "S. Takano" 2 => "E. Yamamoto" 3 => "T. Higaki" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1510/icvts.2008.201517" "Revista" => array:6 [ "tituloSerie" => "Interact Cardiovasc Thorac Surg" "fecha" => "2009" "volumen" => "8" "paginaInicial" => "596" "paginaFinal" => "598" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/19240058" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0040" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Surgical removal of a large mobile left ventricular thrombus via left atriotomy" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "D. Tanaka" 1 => "S. Unai" 2 => "J. Diehl" 3 => "H. Hirose" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.12998/wjcc.v2.i2.32" "Revista" => array:6 [ "tituloSerie" => "World J Clin Cases" "fecha" => "2014" "volumen" => "2" "paginaInicial" => "32" "paginaFinal" => "35" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/24579068" "web" => "Medline" ] ] ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0045" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Mobile left ventricular thrombus in left ventricular dysfunction: case report and review of literature" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "J. Leick" 1 => "S. Szardien" 2 => "C. Liebetrau" 3 => "M. Willmer" 4 => "U. Fischer-Rasokat" 5 => "J. Kempfert" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1007/s00392-013-0565-2" "Revista" => array:6 [ "tituloSerie" => "Clin Res Cardiol" "fecha" => "2013" "volumen" => "102" "paginaInicial" => "479" "paginaFinal" => "484" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/23584757" "web" => "Medline" ] ] ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0050" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Treatment options for patients with mobile left ventricular thrombus and ventricular dysfunction: a case series" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "E. Cousin" 1 => "M. Scholfield" 2 => "C. Faber" 3 => "C. Caldeira" 4 => "M. Guglin" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Heart Lung Vessel" "fecha" => "2014" "volumen" => "6" "paginaInicial" => "88" "paginaFinal" => "91" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/25024990" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23411929/0000006500000007/v1_201807260406/S2341192918300982/v1_201807260406/en/main.assets" "Apartado" => array:4 [ "identificador" => "70434" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Letters to the Director" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23411929/0000006500000007/v1_201807260406/S2341192918300982/v1_201807260406/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2341192918300982?idApp=UINPBA00004N" ]
Share
¿Aún no está registrado?
Información relevante
Consulte los artículos y contenidos publicados en éste medio, además de los e-sumarios de las revistas científicas en el mismo momento de publicación
Máxima actualización
Esté informado en todo momento gracias a las alertas y novedades
Promociones exclusivas
Acceda a promociones exclusivas en suscripciones, lanzamientos y cursos acreditados
Crear Mi cuenta
* = Required fields
Enter your email address
Buscar en
Revista Española de Anestesiología y Reanimación (English Edition)
Toda la web