After a passed oral food challenge (OFC), regular and normal food consumption is attended. The main objective of this study is to assess the safety of tested food dietary re-introduction after a passed OFC.
Patients and methodsIn 2014, a telephone survey was submitted to patients who passed OFC and those who failed it only presenting with contact urticaria (we consider these OFC as passed), between 2009 and 2013. Questionnaire items included demographic data, food allergy details, food consumption after the OFC was performed, recurring symptoms and life style changes.
Results249 OFC questionnaires were collected from 199 children, 228 OFC were passed, 21 were failed exclusively due to contact urticaria. The most tested food was cows’ milk. In 71% of cases target food was re-introduced in patients diet in normal amounts. We found children >2 years introduced less frequently tested food than infants. In 2% of cases adverse reactions to offending food were reported, but severe reactions never occurred.
DiscussionThe majority of children of this study ate target food regularly and their family's quality of life improved. In our study, adverse reactions frequency in patients who passed OFC was very low and never serious. We highlight the importance of re-assessing proper food consumption in every patient who passed OFC.
Food allergy (FA) plays an important role in children and their family's quality of life. If FA is diagnosed, then strict allergen avoidance is officially recommended. Oral food challenge (OFC) is the gold standard for FA diagnosis; moreover, it helps to find out if a patient has outgrown a food allergy.1,2 A passed OFC demonstrates that tested food is tolerated and it can be safely included in patients’ diet. Inappropriate or overly long food elimination diets should be avoided as they may cause several disadvantages. First of all, they may reduce the children's and their family's quality of life; secondly they could induce patient's improper growth3; and lastly they may have negative effects on health expenditure. However, tested food dietary re-introduction does not always follow from a passed OFC. In fact, many patients prolonged their elimination diet even if they passed the OFC, as well as some parents fear to give their children the offending food at home; in fact, there are some reports about adverse reactions occurring even after a passed OFC.4,5,7–9 Therefore, it would seem that OFC can have false negative; this fact could be due to daily life co-factors such as infections or physical exercise, which may increase allergic reactivity.10
Moreover, there is scant literature4,5 regarding whether re-introducing the offending food is adhered to, and, when some patients prolonged the elimination diet, what type of dietary advice these children received, and who gives this advice and why.
The main objective of this study was to assess if, after a passed traditional OFC or a failed one exclusively due to contact urticaria, food re-introduction is safe. We considered the latter a passed test as we allowed patients to include tested food in their diet. For instance, we evaluated if any adverse reaction occurred when food was taken in different situations of daily life. In other words, basing on our population, we rated how many times traditional OFC ended up with a false negative result. Moreover, we wanted to assess: (a) level of parents’ adherence to given instructions (strict or not) and (b) presence of any children/patient characteristic which could influence the adherence to a re-introduction diet.
Patients and methodsAt the paediatric allergy clinic of Agostino Gemelli Hospital in Rome, during the years 2009–2013, patients with a passed OFC or with a failed one due to exclusively contact urticaria were retrospectively identified and included in the study. Among those patients, IgE-mediated FA or Food Protein Induced Enterocolitis Syndrome (FPIES) were previously suspected basing on symptoms and IgE tests.
Final diagnosis was issued from a failed OFC, except those cases of IgE-mediated FA in which anaphylaxis occurred within 12 months, as well as patients affected by FPIES who experienced at least two episodes of repeated vomiting, pallor and lethargy. In all children, skin prick tests (SPT) were performed. They were conducted at the time of diagnosis and prior to each OFC, using fresh food (prick-by-prick with raw and cooked suspected food) and if available, using commercial allergen extracts (Lofarma, Milan, Italy). SPT results were considered positive if the mean wheal size was >3mm than negative control.
With the aim of testing a possible gain of tolerance, many OFCs were performed 1 year after the last adverse reaction to culprit food had occurred. We conducted open OFCs feeding patients suspect food in measured doses. We started with very small doses and increased food amounts every 20min. In the last three doses total food amount was almost equal to the patients’ average daily intake (one egg, 200ml of cow's milk). When the last dose was given, patients remained under clinical observation for 2h. OFC was interrupted and considered failed in case of objective symptoms and/or serious and/or persistent and/or reproducible ones.11 Patients presenting exclusively with contact urticaria during the OFC were able to tolerate a full dose of tested food. After a passed OFC or a failed one due to limited contact urticaria, all families were told to start a normal diet containing the offending food in normal amounts.
In 2014, parents of enrolled patients were contacted and underwent a telephone interview based on a questionnaire; all parents gave informed consent. Questions included demographic data, food consumption after the OFC, adverse reactions recurrence, and a request for explanation of any food avoidance.
The study was approved by the local Ethics Committee (protocol P/68/CE/2011).
Statistical analysisAll data were entered into an Excel spreadsheet and analysed using Excel 2010 (Microsoft, Redmond, WA, USA). Fisher exact test (two tailed) was used to analyse the significance of the association between variables (p<0.05).
ResultsPatients’ characteristicsDuring the study period, 297 OFC with the required characteristics were recorded. 48 families (16%) were not reached by telephone, therefore the interviews focused on 249 OFC in 199 children. 228 OFC were passed, and 21 were failed due to the presence of exclusively contact urticaria. Tested foods were cows’ milk (CM, 112), hens’ egg (77), fish and shellfish (18), fruit or vegetables (15), grains (8), peanuts (5), nuts (3), hazelnut (2), pistachio (1), soy (3), beef (4), and chicken (1). 53/199 children (26%) were also affected by respiratory allergies. Median age at diagnosis was 19 months (range 0–13 years) and tolerance OFC was performed at a median age of 30 months (3 months–13 years).
At the time of diagnosis, clinical manifestations were urticaria and angio-oedema (121 children), vomiting and abdominal pain (51 children), generalised non-anaphylactic allergic reaction (26 children), anaphylaxis (16 children), FPIES (14 children). Median time length between OFC and data collection was 2.5 years (6 months–5 years).
Adherence to dietary adviceIn 71% of cases (176/249) tested food was re-introduced regularly and in normal amounts (i.e. doses were appropriate to children age and food type), while in 21% (52/249) food was given occasionally and in small amounts. In 8% of cases (21/249) food was not given at all and parents’ motivations were: fear of an adverse reaction,6 doubts regarding the persistence of allergy,7 different advice of general practitioner or other allergist,6 and children lack of preference.2 Patients who did not re-introduce tested fish or shellfish into their diet did not take any other type of fish or shellfish either.
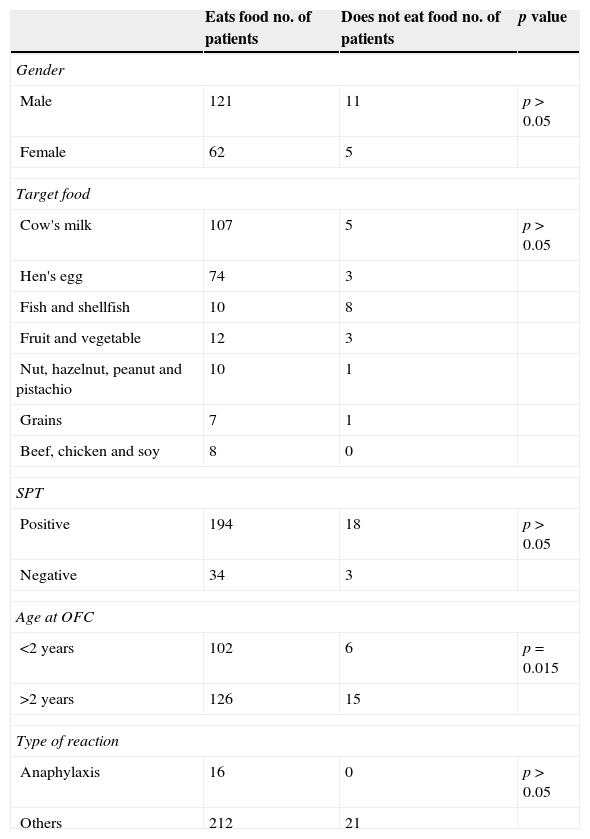
We investigated factors, which may influence food introduction after OFC is performed (Table 1). We found no difference in the consumption patterns according to gender, initial reaction's severity, type of food, presence of specific IgEs, or further allergies. We noticed that children >2 years old introduced tested food less frequently than infants (p=0.015).
Factors potentially influencing tested food introduction after OFC.
| Eats food no. of patients | Does not eat food no. of patients | p value | |
|---|---|---|---|
| Gender | |||
| Male | 121 | 11 | p>0.05 |
| Female | 62 | 5 | |
| Target food | |||
| Cow's milk | 107 | 5 | p>0.05 |
| Hen's egg | 74 | 3 | |
| Fish and shellfish | 10 | 8 | |
| Fruit and vegetable | 12 | 3 | |
| Nut, hazelnut, peanut and pistachio | 10 | 1 | |
| Grains | 7 | 1 | |
| Beef, chicken and soy | 8 | 0 | |
| SPT | |||
| Positive | 194 | 18 | p>0.05 |
| Negative | 34 | 3 | |
| Age at OFC | |||
| <2 years | 102 | 6 | p=0.015 |
| >2 years | 126 | 15 | |
| Type of reaction | |||
| Anaphylaxis | 16 | 0 | p>0.05 |
| Others | 212 | 21 | |
OFC=oral food challenge, SPT=skin prick test.
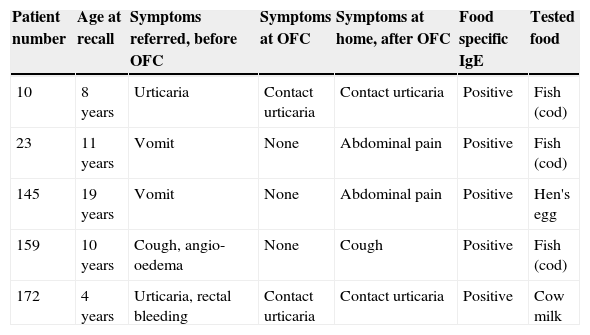
In 2% of questionnaires (5/249) adverse reactions to tested food were reported by parents (Table 2). However, none of them showed a severe reaction. In our opinion, three patients presented with symptoms which were not consistently related to the tested food (no. 23, 145, 159) (i.e. symptoms appeared over a period longer than 2h after food ingestion occurred and persisted over more than 8h). Two patients showed food-induced contact urticaria (patients no. 10, 172), which was already observed during the OFC.
Patients reporting symptoms at diagnosis and after OFC.
| Patient number | Age at recall | Symptoms referred, before OFC | Symptoms at OFC | Symptoms at home, after OFC | Food specific IgE | Tested food |
|---|---|---|---|---|---|---|
| 10 | 8 years | Urticaria | Contact urticaria | Contact urticaria | Positive | Fish (cod) |
| 23 | 11 years | Vomit | None | Abdominal pain | Positive | Fish (cod) |
| 145 | 19 years | Vomit | None | Abdominal pain | Positive | Hen's egg |
| 159 | 10 years | Cough, angio-oedema | None | Cough | Positive | Fish (cod) |
| 172 | 4 years | Urticaria, rectal bleeding | Contact urticaria | Contact urticaria | Positive | Cow milk |
OFC=oral food challenge.
21 children failed the OFC exclusively due to the presence of contact urticaria. In 57% of cases (12/21) food was re-introduced regularly and in normal amounts, while in 29% (6/21) it was given occasionally and in variable amounts. In 14% of cases (3/21) the tested food was avoided, in fact two children reported on their fear of a hypothetical allergy persistence, as one child followed different advice received from a general practitioner or another allergist.
In our survey, 8/21 children, among those who had regularly eaten the target food, showed contact urticaria. Anyway, their parents declared that this symptom did not stop them from feeding the tested food to their children.
Family satisfaction90% of families (180/199) were fully convinced of OFC's accuracy and safety, 7% (14/199) declared to be uncertain, and 3% (5/199) were not convinced at all. After the phone survey all parents have been willing to repeat OFC if necessary and in 98% of cases (195/199) they reported an increase in their family's quality of life thanks to the implementation of OFC.
DiscussionIn this study, adverse reactions prevalence reported by parents, after their children passed an OFC or even if they failed one presenting with contact urticaria only, was 2% (5/249 questionnaires). All reactions were mild and in three cases the causal relationship between the ingestion of involved food and patients symptoms was not clear. Two other children presenting with contact urticaria during the OFC, afterwards showed the same problem. In our opinion, this is the most relevant result of our research, as it underlines the high negative predictive value of traditional OFC (virtually 100%). Unfortunately, the majority of OFCs were performed with CM and hen's egg. There were only a few individuals who underwent other food OFCs, so that there is insufficient information to draw conclusions about other food (including fish, nuts, etc.) adverse reactions prevalence.
Other studies have examined this issue (4, 5, 7–9). Caffarelli et al.7 performed 370 OFC in 242 children, aged from three months to 14.6 years (mean 3.2 years). Five (3%) of the 193 children tolerating foods on challenges developed immediate symptoms (urticarial, angio-oedema, rhinitis, conjunctivitis) when the same food was ingested openly the next day at home. Authors suggested that open feedings under observation, the day after patients passed the OFC, could be useful to exclude false negatives. Eigenmann et al.4 studied 73 children, median age at diagnosis was 12 months (range 0–12 years), and challenge was performed at a median age of 4 years (11 months–15 years). The tested foods were milk (23), hen's egg (22), peanuts (13), fish and shellfish (4), soy (3), fruits or vegetables (2), grains (2), food dye and preservatives (2), beef (1) and nuts (1). Four questionnaires reported that food re-introduction was conducted in large amounts, 35 in normal amounts and 14 occasionally. In 14 cases the tested food was avoided, while four patients did not eat it at all. These results show that in 25.4% of cases food was not re-introduced after a negative challenge test. At re-introduction time, some parents (5/73, 7%) reported symptoms such as oral itching, urticaria with larger food amounts, atopic dermatitis flares, perioral skin rashes, and sneezing. In two patients these symptoms were not consistently food-related, two others had an adverse reaction possibly due to raw egg's persisting allergy; in fact they passed a challenge performed with cooked egg. The fifth child showed food-induced contact urticaria. None of these patients had a severe reaction. Flammarion et al.5 studied 67 children [median age: 5.2 years (0.9–16.0)]. The main tested foods were hen's egg (27 cases, raw eggs=17), cow's milk (17 cases) and peanut (11 cases). The target food was eaten regularly in 83% of cases, and nine patients ate it less frequently. In two cases the tested food was never administered (lentil and tomato) as parents feared their children could have an allergic reaction. Three children refused to eat it at all (almond, peanut, egg). Six parents (9%) reported symptoms after the OFC were conducted; they were never severe (diarrhoea, sneezing, facial oedema, urticarial) and in four cases they were likely to be FA-related. Niggeman et al.8 prospectively performed 490 OFC with the six most common food allergens: cow's milk (109), hen's egg (166), wheat (35), soy (20), peanut (103), and hazelnut (57). On the total amount, 289 (59%) were considered positive. Among the last ones, 251 (87%) turned to be positive during the seven increasing dose steps and 38 (13%) after having administered the cumulative dose on another day. Twenty-six of the 38 children (9% of all positives) presented with urticaria and/or angio-oedema, and the other 12 with stomach ache, nausea, redness, worsening of eczema, or contact urticaria. Similar results were obtained for all foods. The authors point out that these data show that a considerable number of OFC may be assessed as false negative if a cumulative dose is also not administered on another day. Koplin et al.9 performed OFC in 936 infants and reported that 1.6% of them did not react on day 1 of the challenge (raw eggs and peanut), but they had symptoms afterwards; they were at home on days 2 or 3 after the challenge was performed. Any reaction occurring at home required epinephrine.
Basing on our results and the current literature, we can state that tested food dietary re-introduction, after a passed OFC, does not expose paediatric patients at risk of severe adverse reactions, regardless of daily living different conditions (infections, physical activity, food of a different variety). The same concept can be extended to those paediatric patients who presented with only contact urticaria during the OFC.
However, in spite of these results, the percentage of adherence to allergist prescriptions is lower than 100%. Basing on literature4,5 it is known that not every patient who acquired tolerance to a specific food always re-introduces it into his/her diet. These data were confirmed in our research. As in previous studies,4,5 our results showed that adherence to allergist's requirements was not related to any socio-demographic factors, neither to other allergies coexistence, nor to the first allergic reaction severity. In our study, children >2 years introduced tested food very less frequently than infants; this fact could be explained by children acquisition of autonomy skills and its own feeding behaviour. Another explanation could be related to food type: it is easier to avoid fish than cow's milk or egg, as those ones are very common in children's foods. As fish allergy is more common in children >2 years, this could explain the difference, rather than the age. However, the number of children >2 years who ate fish did not differ from those who are <2 years old who ate fish. The same result was observed among those who did not eat fish (data not shown).
In conclusion, our results encourage to use traditional OFC method, without variations. Moreover, we wish to highlight the importance of re-introducing the tested food for all those patients who passed the OFC.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Protection of human subjects and animals in researchThe authors declare that no experiments were performed on humans or animals for this investigation.
FundingNone.
Conflict of interestNone.