Female patient, 99 years old, dependent for activities of daily living.
Undergoes to the Emergency Department, for two weeks of food refusal, associated, since the previous day, with abdominal distension, fecaloid vomiting and associated pallor.
Was confused and with aggressive behavior, apyretic (36.1°C), hypotensive (88/70mmHg) and tachycardia (125bpm), with distended abdomen, painful on palpation in all quadrants. Personal history of arterial hypertension and fracture of the proximal femur with surgical intervention in 2015.
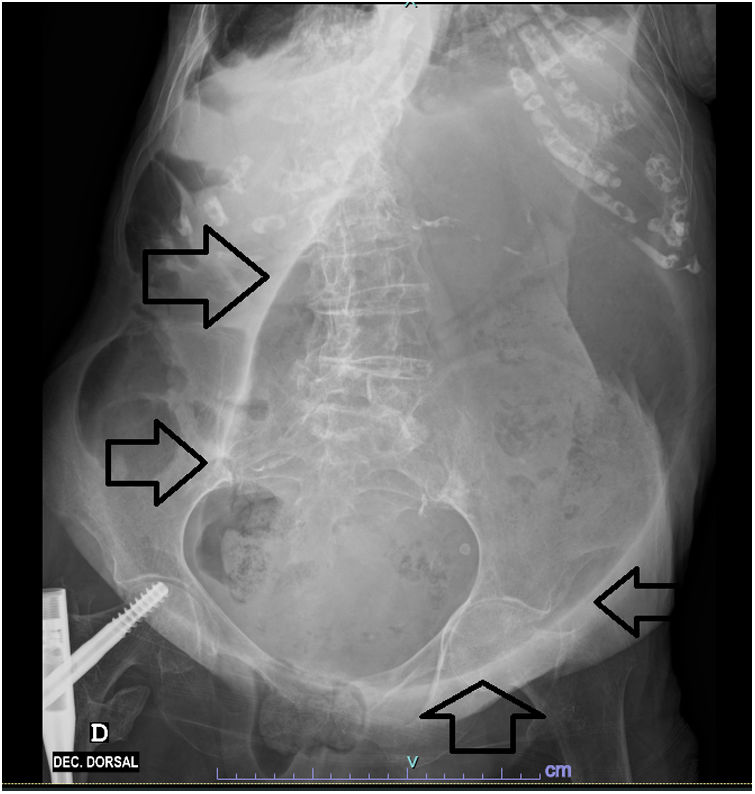
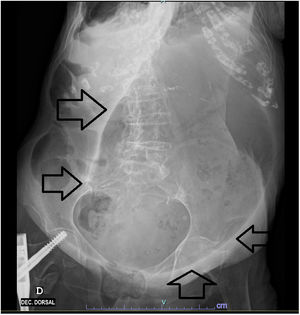
Analytically, he had leucocytosis, acute kidney injury, elevated troponin (973.2ng/l – reference value 0–15.6ng/l), pro-BNP (16407pg/ml – reference value 0.0–125pg/ml) and C-reactive protein (8.95mg/dl – 0.0–0.5mg/dl). Electrocardiogram with atrial fibrillation, with no apparent acute pathology. Radiography of the abdomen with marked gastric distention with the presence of air-fluid levels (Figs. 1 and 2).
She was medicated with metoclopramide and, after evaluation by surgery, a nasogastric tube was placed, with drainage of fecal content. Moments later, the patient died, having chosen not to initiate invasive measures.
The drainage of gastric contents may have provoked vascular collapse at the abdominal level, not forgetting, given analytical changes, the possible associated myocardial or mesenteric ischemia.